4 Jaw Exercises for TMJ Relief by a Facial Pain Expert
A facial pain and TMJ disorder expert describes four jaw exercises for facial pain that are comfortable to perform.
TMJ disorder (aka TMD) causes quite a few symptoms, but among the most common is pain, including that in the face.
Before beginning these exercises, you should have a diagnosis of TMJ disorder rather than just assuming you have this common problem.
“The following exercises are often helpful to patients with facial pain,” says Donald R. Tanenbaum, DDS, MPH, a board certified TMJ and orofacial pain specialist, and author of “Doctor, Why Does My Face Still Ache.”
These jaw exercises for facial pain do not represent the full scope of jaw exercises available, adds Dr. Tanenbaum, but these are a great start if you’ve been suffering from facial pain.
Very important: Don’t hold your breath; breathe normally as you perform these movements. There should not be any pain while doing them.
Jaw Exercise 1
Goal: Release tension in jaw-closing muscles
Place your thumb directly under your chin. Place your tongue on the roof of your mouth, halfway back.
Attempt to open your mouth against gentle thumb resistance, as your tongue is kept in contact with the roof of your mouth.
Resist for 3-4 seconds without letting your jaw reach the maximum open position. Repeat 6 times.
Jaw Exercise 2
Goal: Help coordination of muscles that move jaw from side to side
Take a tongue depressor and gently rest it between your upper and lower teeth.
Swing your jaw to the right, gliding on the tongue blade, and feel the resistance. Hold it for 3-4 seconds. Repeat on the opposite side. Do 10 repetitions of both.
Jaw Exercise 3
Goal: Stretch jaw-closing muscles
While sitting down, place your left elbow on a table and lean your forehead into the palm of your hand.
With the index and middle fingers of your right hand, pull down on the lower front teeth to open the jaw until you feel a stretch in your facial muscles. Hold for 3-4 seconds, release, and repeat 10 times.
Jaw Exercise 4
Goal: Limit forward movement of jaw on mouth opening
Place your tongue on the roof of your mouth, halfway back. Open your mouth in front of a mirror.
Try to open in a straight line. Hold in a limited open position for 5 seconds. Release. Repeat 5-10 times.
Be consistent with these exercises, and the pain situation from your TMJ disorder should improve.

Dr. Tanenbaum’s practice focuses on facial pain, TMJ disorder and sleep-related breathing disorders. He is the past president of the American Academy of Orofacial Pain and takes a multidisciplinary approach to his patients’ care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/michaelheim
Is Dizziness from Exercise Different than from Anxiety?

Anxiety can cause you to feel dizzy, and so can exercise.
There are different kinds of dizziness, and each has different causes.
Anxiety is a common cause of dizziness.
However, if you feel dizzy after or during exercise, this can be caused by 1) Lack of nourishment; low blood sugar, or 2) The actual exercise itself, such as pivoting ‘round and ‘round on a stepper.
After all, the dizziness from anxiety is triggered by the rapid breathing that anxiety causes.
However, exercise, too, causes rapid breathing, but normally, a person will not get dizzy from exercise.
I’m a former certified personal trainer and rarely did my clients report feeling dizzy during or after exercise.
The few times this has happened involved clients who hardly ate anything the entire day prior to their exercise session with me.
Why would rapid breathing from anxiety leads to dizziness, and why would rapid breathing from exercise not lead to it?
“When people exercise they breathe rapidly because their muscles require more oxygen, and they also need to breathe out the excess carbon dioxide that is produced during exercise,” explains Peter Swanljung, MD, chief of psychiatry at the Malvern Institute in Willow Grove, PA.
“So the increased breathing is a result of the body functioning appropriately in response to exercise.
“When someone is anxious, they are breathing more rapidly than the body needs them to, and thereby are releasing too much carbon dioxide, which can cause the pH of the blood to rise and cause a constriction of the blood vessels in the brain, leading to a dizzy sensation.”
There are many other causes, such as premenstrual syndrome, and quickly rising to a standing position after being seated for a while.
A very pervasive cause is prescription medications, such as statins and antidepressants.
And of course, pregnancy can cause the sensation as well. Sometimes, unknown causes are at play.
In general, for the most part, if you feel dizzy, this is no cause for alarm.
Often, you know what the cause is right then and there: Are you premenstrual?
Did you just quickly stand up from a seated position? Have you not eaten anything all day?
Did you just try a new dance move that required some spinning?
Are you ill from a “bug” or the flu? Did you recently bang your head?
Are you on a new medication?
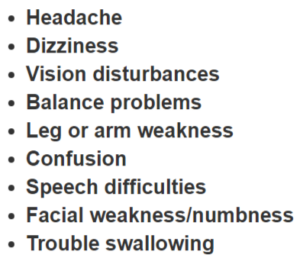
Rarely, dizziness is a sign of serious trouble, such as a transient ischemic attack.
A TIA is recognized by the medical establishment as an emergency situation that signals the possibility of a full-blown stroke in the near future.
However, the dizziness of a TIA is usually accompanied by any of the symptoms listed below.
 Dr. Swanljung is the former medical director of the general adult unit at Friends Hospital in Philadelphia and treats a variety of psychiatric conditions.
Dr. Swanljung is the former medical director of the general adult unit at Friends Hospital in Philadelphia and treats a variety of psychiatric conditions.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com yanalya
Bloody Urine: Top Causes Including Cancer

Blood in the urine has many causes, including cancer, and the sight of blood in your urine can be very frightening.
Obviously, this isn’t normal.
Or is it at times? It’s important to take a look at your urine on a regular basis.
What are the top 8, in order of likelihood, causes of blood in the urine?
Answering questions is Dr. Andrew Stephenson, MD, Section Chief and Director, Urology Oncology; Professor (PAR), Department of Surgery, Division of Urology, Rush Medical College.
Dr. Stephenson: Infection; Stones; Benign prostatic enlargement; Kidney cancer; Bladder cancer; Ureteral cancer; Medical renal disease; and Trauma.
In other words, if you see blood in your urine, it’s not necessary to suddenly fear you must have cancer.
In fact, if you see blood in your urine, you might want to ask yourself if you’ve been exercising strenuously lately. This is a type of “trauma” that can cause blood in the urine.
The following exercises can lead to urinary blood: distance running, rigorous cycling, and jumping/plyometric routines. Accident trauma can also cause urinary blood.
Top medications likely to cause bloody urine?
Dr. Stephenson: Anticoagulation therapy, e.g., Coumadin, Plavix, Heparin.
According to Ohio Health Online, here are more causes for blood in the urine:
Red: A red tinge may appear to be blood, when it’s not. One cause of a red tinge is porphyria, a skin and nervous system disorder; red or deep purple foods such as blackberries, beets and rhubarb pie; laxatives like Ex-lax; and other prescription drugs including Thorazine, an antipsychotic that’s also used to treat nausea from chemotherapy.
Blood in: Urinary tract infections, cancer of the kidney or bladder (seldom), and also, a leading cause of visible hematuria in kids is kidney inflammation caused by a bacterial/viral infection.
Guidelines for urinalysis for bacteria in the urine (bacteriuria), that is without symptoms. (Symptoms include urinary tract infections and inflammation of the kidneys and bladder.)
These guidelines are from Surgeon General Reports:
- American Academy of Family Physicians and U.S. Preventive Services Task Force — asymptomatic bacteriuria screening, by urine culture, should be performed on all pregnant women.
- The American College of Obstetricians and Gynecologists recommends screening for this, for women over age 65, or women with type 1 diabetes, as a routine part of physical exams.
- The American College of Physicians advises against routine screening.
- Canadian Task Force on the Periodic Health Examination — For patients with type 1 diabetes, a screening for protein to prevent renal disease is advised. But for the elderly, a screening to detect symptom-free bacteriuria is not advised.
 Dr. Stephenson’s clinical and research focus is the treatment of prostate, bladder, kidney and testes cancer. He has published over 100 articles in peer-reviewed journals.
Dr. Stephenson’s clinical and research focus is the treatment of prostate, bladder, kidney and testes cancer. He has published over 100 articles in peer-reviewed journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Eag1eEyes
Can Diarrhea Be the Only Symptom of Microscopic Colitis?

A sudden onset of diarrhea, including a lot of diarrhea, but with no other symptoms, may signal an inflammatory bowel condition known as microscopic colitis.
Microscopic colitis falls under the category of “colitis,” which falls under the category of “inflammatory bowel disease.” Don’t confuse this with irritable bowel syndrome.
Inflammatory bowel disease simply means a flare-up, or inflammation, of the inner lining of the large colon.
A colonoscopy is necessary to confirm this, and depending on the type of IBD, a gastroenterologist can make the diagnosis visibly right there on the spot.
However, microscopic colitis is not visible to the un-aided eye. A colonoscopy exam should include a routine collection of large colon tissue, to be sent for a pathology report.
This is where the diagnosis of microscopic colitis is made. There are two types of microscopic colitis: lymphocytic and collagenous.
Mayoclinic.com reports that microscopic colitis can present with the following symptoms: watery diarrhea (no blood in it), abdominal cramping, abdominal pain, abdominal bloating, some weight loss, stool leakage, nausea, dehydration, and urgency to relieve the diarrhea.
However, it is entirely possible for microscopic colitis to produce just one symptom: the diarrhea.

This “sort of” happened to me, although I did have some abdominal cramping (mild) going on, but this was often from the bowel movements building up inside me, and was relieved once I used the restroom.
I say “sort of” because at the time, I didn’t know that the joint aches that I had were part of microscopic colitis.
I thought they were related to my menstrual cycle, even though the menstruation had ceased.
I would later learn that joint aches are a recognized symptom of MC, and involve the same hormones (prostaglandins) that cause the joint aches of PMS!
In my case, the joint aches persisted after my period stopped, and historically, this had never happened; my PMS joint aches had always been just that: PRE-menstrual, not POST-menstrual.
I also had dehydration in the form of notable thirst in the middle of the night. These latter symptoms are secondary to the diarrhea.
I had absolutely no abdominal bloating or distention, and certainly no fecal leakage, nausea, or any actual pain in my abdomen.
I simply had this annoying diarrhea, which wasn’t always watery, and the suspicious joint aches.
Sometimes many small and medium pieces of poorly formed BMs plopped out at once, but technically, they were not formed stools because a gentle poking of them with a cotton swab would cause a dispersal of the matter.
Flushing the toilet would also disperse the stools; that’s diarrhea.
A change in diet can alter the appearance of the diarrhea, making it appear less “diarrheaic.”
A change in diet can pretty much eliminate it as well, but this does not mean that the microscopic colitis has been resolved; it’s still there and must run its course.
When I eliminated fruit from my diet, the diarrhea stopped, but I continued to have a change in stool caliber.
They were greasy looking, layered, appearing to be made up of several different kinds of material; containing a lot of undigested food; light brown; sometimes tinged with green or a little orange, depending on the colors of the foods I had eaten.
A course of only diarrhea can also be caused by a local infection in the intestines (my doctor’s initial diagnosis pre-colonoscopy), and stress.
However, stress is not likely to change the caliber of your stools. If you suspect microscopic colitis, a colonoscopy is needed for diagnosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How to Prevent Esophageal Cancer if You Have GERD
What is the best way to help prevent esophageal cancer if you have GERD (gastroesophageal reflux disease)?
Or, to put it another way, are there specific ways to lower the odds of ever developing esophageal cancer if you have GERD?
Chronic acid reflux disease is a risk factor for cancer of the esophagus.
The esophagus is the so-called food pipe.
How GERD Raises Risk of Esophageal Cancer
The chronic coating of the stomach’s acidic contents on the interior lining of the esophagus changes its cellular structure over time.
The cells become similar to those of the small intestine when this happens. This is a condition called Barrett’s esophagus.
If you’ve been diagnosed with Barrett’s esophagus, you have a risk factor for developing a malignant tumor in the esophagus.
Prevention Tactics for Esophageal Cancer if You Have GERD
There are things that you can do, says Dr. Maxwell Chait, MD, gastroenterologist at ColumbiaDoctors Medical Group in Westchester County, NY.
Dr. Chait says, “Lifestyle modification with weight loss; avoid fried and fatty foods, caffeine, alcohol and tobacco.”
This may sound like advice to stop having fun, but giving up your vices sure beats sitting for hours receiving chemotherapy through a drip bag after being told you have a disease with a five-year survival rate of only 19.2 percent.
Is that next cigarette, drink or bucket of fast-food fried chicken worth it?
Think you’re too young to worry about any of this?
Additional data from the National Cancer Institute Surveillance, Epidemiology, and End Results Program says that 10.4 percent of new diagnoses occur in people 45 to 54, and 27.1 percent occur in people 55 to 64.
If you’re in your 20s or 30s, you’re not immune.
But another point to consider is that the sooner you start prevention tactics for esophageal cancer, the better your chances are of never being diagnosed with this illness later on in life.
Dr. Chait continues, “Treatment of GERD with acid reducing medication to lower acid reflux” is yet another strategy.
Prilosec is an acid-reducing drug.
But “use of NSAIDS such as aspirin is controversial since they can also damage the GI tract.”
Dr. Chait adds, “Surgery to prevent acid reflux remains controversial.”
If you’ve already been diagnosed with Barrett’s, he says that the progression of this condition can be prevented “using endoscopic methods to ablate the Barrett’s.”

Dr. Chait’s practice interests include digestive conditions such as colon cancer, gastrointestinal endoscopy and internal medicine. He has authored numerous publications in reputed journals.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/goodluz
Is Sex Necessary for Anal Cancer from an HPV Infection?

Though anal cancer is strongly linked to HPV, anal intercourse is not necessary to contract this virus that can lead to this cancer.
Did you know that 95% of anal cancer cases are caused by the human papillomavirus (HPV)?
This stat comes from analcancerfoundation.org, though cdc.gov/hpv/cancer.html says it’s 91%.
Intercourse is not necessary to transmit HPVs that ultimately can cause anal cancer, says analcancerfoundation.org.
Intercourse (vaginal or anal) is also not required to transmit the HPVs that can eventually cause cervical, vulvar, penile or oral cancers, says the foundation.
In fact, the foundation states that HPV can also be transmitted from person to person by deep kissing, manual stimulation of the genitalia, rubbing, sex toys…
In addition, researchers with the University of Hawaii HPV Cohort Study point out that “the majority of cervix-to-anus transmission” of HPV “happened in the absence of anal intercourse.”
The article concludes: In short, anal intercourse is not a pre-requisite for getting anal cancer.
Sources: analcancerfoundation.org/learn/anal-cancer/ and cdc.gov/hpv/cancer.html
Another site, cancer.org, specifically states: HPV is passed from one person to another during skin-to-skin contact with an infected area of the body.
The site notes that HPV can be spread during the act of sex—any kind (anal, vaginal and oral)—but that sex is not necessary for HPV to spread.
All that is needed is for there to be skin-to-skin contact with an area of the body infected with HPV.
In fact, HPV can be spread through non-intercourse genital-to-genital contact, and even with just hand-to-genital contact.
This ubiquitous virus can spread from one body part to another, e.g., from genitals to anus—without the assistance of the victim’s partner.
HPV is really out there. The site states that it “might be possible” to protect against a genital infection with this virus by forbidding people to contact your genital and anal regions.
However, the site says that there may still be undiscovered ways that HPV can make it into someone’s body.
For reasons not known, HPV infections mainly occur in women when they are under age 30.
Cancer.org says that the mean age of diagnosis (men and women) is 62. It takes many years for an HPV infection to develop into anal cancer.
This is not a disease where one contracts HPV in a particular year, and then three years later gets the dreaded diagnosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/pressfoto
Sources:
cancer.org/cancer/analcancer/detailedguide/anal-cancer-risk-factors
cancer.org/cancer/analcancer/detailedguide/anal-cancer-what-is-key-statistics
Why Are the Cramps from Microscopic Colitis Painful?

“Typically, people have symptoms of abnormal pain in conjunction with diarrhea when they have microscopic or collagenous colitis,” says gastroenterologist Sander R. Binderow, MD.
“If a physician looks at the colon, it appears to be normal, but if the patient continues to have problems, the doctor will likely take random biopsies, which are sent to a lab and come back with results showing the lining as abnormal, which is called mucosa,” says Dr. Binderow, who’s with Atlanta Colon & Rectal Surgery.
“Cramps are the same with both diarrhea and microscopic colitis. The level of pain is not associated with the difference between regular diarrhea and colitis.
“Symptoms of microscopic colitis are less abnormal than obverse or gross colitis.”
Sometimes, cramps can get really bad preceding the voiding of diarrhea.
Dr. Binderow explains, “Any colon or bowel pain is due to distension, which is when the colon is distended due to extra air.
“Colitis, or inflammation itself, does not cause any extra or extreme pain; it’s distension due to more air in the colon that can cause pain.”
Microscopic colitis is NOT a risk factor for colon cancer, no matter how painful the cramps.
Symptoms of colon cancer, that are not shared with microscopic colitis, are as follows: blood in the stools, unexplained weight loss, a persistent feeling of malaise, unexplained fatigue, abdominal pain that’s not related to diarrhea or BMs, feeling you still have to void BMs even after you “got everything out,” pencil-like stools, and constipation that alternates with diarrhea.
If you have any of these symptoms, you should see a gastroenterologist, who may recommend a colonoscopy as a diagnostic tool.
But if you’re free of symptoms and simply want to be screened for colon cancer, you can take an at-home colon cancer screening exam called Cologuard.

Cologuard
Your sample will then be analyzed for abnormal cells using the latest DNA technology.
If the cells are atypical, a colonoscopy will be recommended.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Zetar Infinity
Can Tight Socks Cause Edema?

Is it edema when you roll down your tight socks and see that big indent in your leg?
“I have a memory of my grandmother, who used an elastic band to hold up her stockings,” begins Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
“At the end of the day, when she would roll them down, there was a clear groove in her leg above slightly swollen calves.
It turns out that blood pumped down to the legs requires the relatively weak pumping action of calf muscles to return that blood to the circulation.
“External compression on surface veins can cause that blood, and another body fluid called lymph, to stagnate in the legs.
“This produces the surface irregularities that mirror the constricting devices that had been used on the legs.
“These days, tight socks can do the same thing, as can about anything else that impedes the circulation.
“Avoiding such constriction, walking around a bit to get those body fluids back in circulation, and even elevating the legs once freed of constraints all help to obliterate those nasty lines.”
If only your tight socks are causing edema, you have nothing to worry about.
However, you may already have edema that’s being caused by a medical problem or lifestyle habit, and the tight socks are simply making this fluid buildup more noticeable or aggravating it.
Lay off the tight socks to see if it disappears. If not, you need to find out why this swelling is occurring.
Common Causes of Edema
- Heart Failure: When the heart struggles to pump blood efficiently, fluid can accumulate in the legs.
- Kidney Problems: Conditions affecting the kidneys can impair the body’s ability to manage fluid balance, leading to swelling.
- Liver Disease: Liver conditions like cirrhosis can disrupt normal fluid balance and lead to fluid retention in the legs.
- Venous Insufficiency: Poor circulation in the veins, often due to damaged or weakened vein walls or valves, can cause blood to pool in the legs, causing swelling.
- Medication Side Effects: Certain medications can puff up the legs.
- Pregnancy: Increased blood volume and pressure on the veins from the growing uterus can lead to swelling in the legs, especially later in pregnancy.
- Infections: Infections in the leg can cause swelling along with redness, pain and warmth.
- Lymphedema: A condition where the lymphatic system is damaged or obstructed, leading to fluid buildup in the tissues of the legs.
- Menstruation: One’s period can lead to a puffiness in the feet that may extend a little bit above the ankle.
- Poor Diet: High salt intake can cause fluid retention, leading to swelling in the legs.
Again, if you’re worried, avoid wearing tight socks or any socks, for that matter, and see what happens over the next several days.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
What Kind of Doctor Treats Vertigo?
Vertigo has many causes, so what kind of doctor should you first see?
A common cause of vertigo involves the inner ear canal. This might be the cause of your vertigo — which to some sufferers, is described as the room “spinning,” “whirling” or moving. It may also be described as sort of like a motion sickness.
“Vertigo, or more precisely, benign paroxysmal positional vertigo [BPPV], is a condition in which little particles contained within the inner ear’s balance organ lose their positioning accuracy, and you feel dizzy,” says Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
“You can feel so dizzy that you become nauseated, vomit and even fall down,” he explains.
BPPV can also be very mild, in that the patient feels just slightly dizzy or “heady,” but is otherwise fully functional.
“Once diagnosed, the proper treatment is to put those little particles, called canaliths [otoconia], back where they belong,” says Dr. Leavey.
“By moving the head in a precise pattern, called an Epley maneuver, BPPV can often be easily treated in the office.
“While many physicians can treat vertigo, the therapy is often practiced most skillfully by trained physical therapists, who have the skill and facility to render effective treatment.”
What Type of Doctor to See
If you believe you have benign paroxysmal positional vertigo, your family practitioner will be able to make this diagnosis. Describe the situation. Don’t just say, “I feel dizzy.”
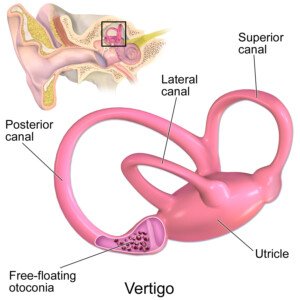
The free-floating otoconia or “crystals” can get out of place and cause vertigo. BruceBlaus/CreativeCommons
A hallmark feature of BPPV is that the patient feels the dizziness only when they move their head.
For example, you’re busy at your computer. Your head is not moving left to right because your eyes are glued to the screen. All is fine.
You then turn your head 90 degrees to the right to grab your coffee mug…and you feel a wave of dizziness.
The room may seem to shift a little, but this isn’t always the case. Sometimes with benign paroxysmal positional vertigo, you feel only that annoying dizziness.
For some patients this disappears when they lie down. For others it gets worse. Often, rising from a lying position will trigger the dizziness.
If they close their eyes while feeling the dizziness, they may feel a sensation of their body or the room spinning about.
In severe cases, the symptoms can be way out of proportion to the benignity of this disorder.
Intense dizziness, especially accompanied by vomiting, will be frightening to someone who doesn’t realize this is due to those canaliths.
So if BPPV sounds like what you have, see your general doctor. If your symptoms don’t quite fit this benign type of vertigo, you should still first see your primary care doctor.
Dizziness can have so many causes, and also, some people think they’re dizzy when actually they are experiencing a faintness type of feeling.
Feelings of faintness can be caused by heart arrhythmias, low blood pressure, low blood sugar, pregnancy and side effects of medications, among many other causes.
A neurological cause, too, may be behind a wave of dizziness, so as you can see, depending on the cause of the “vertigo,” you may be referred to a specialist by your primary care physician.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
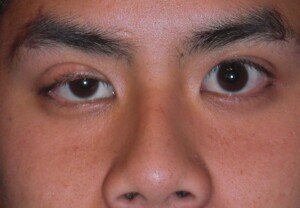
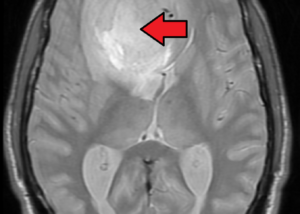
What Is Ptosis and Miosis?
Ptosis, as it pertains to symptom of a leaking aneurysm, refers to a drooping eyelid.
The drooping, or ptosis, can have a variety of causes, including a brain aneurysm that has begun to leak.
Another cause of what appears to be eyelid ptosis (perhaps Paris Hilton and Taylor Swift have this?) is “looseness of the skin of the eyelid, causing it to hang down, and even block the visual field,” says Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
Ptosis can be acquired later in life as well. The ability to control the eyelid involves muscles and nerves.
Eyelid ptosis is divided into four basic classes: myogenic, neurogenic, mechanical and involutional.
- Myogenic (“myo” means muscle) means something is wrong with the muscle of the upper eyelid.
- Neurogenic (“neuro” means nerves/neurons) means that the nerve that supplies the eyelid muscle with movement commands, is impaired.
When the muscles in the eyelid have weakened, the result is involutional ptosis.
Mechanical eyelid drooping is when the weight of the eyelid has become too great for muscular control, and hence, the drooping.
The myogenic version can result from a muscle disease. Neurogenic-caused drooping can be caused by aneurysm, stroke, diabetes, injuries and the dreaded brain tumor.
But Dr. Leavey explains, “Very rarely, tumors or growths in the brain, or leaking or swelling blood vessels in the brain can press on a nerve headed to the eyelid, producing a ptosis.”
As for mechanical ptosis, excess skin, fat and tumors can cause this.
Finally, aging is the primary culprit with involutional ptosis. The muscles and nerves work just fine here, actually.
The problem is when the muscle detaches from the eyelid structures. Thus, the muscle is able to contract, but it’s not attached enough to the eyelid any more to move it.
Ptosis can be corrected with surgery—depending on the cause.
“A key diagnostic question is if the drooping lid is on one side or both,” says Dr. Leavey.
In general, bilateral ptosis is caused by a systemic condition, one that is not specific to the region of one eye, or even the eyes themselves.
“While very uncommon, they include conditions as wide ranging as myasthenia gravis to a whole raft of genetic diseases.”
Miosis simply means a constriction of the eye’s pupil. Miosis is not to be confused with meiosis, which is a type of cell division.
“By itself, unilateral miosis [one eye only] is quite a bit less common; eye drops or other external chemicals can be one cause,” says Dr. Leavey.
If you have one-eye miosis, you should see a physician to rule out a disease process, though if disease is the cause, you’ll very likely have ptosis with it.

Ptosis and miosis. Source: physio-pedia.com
Dr. Leavey continues, “Many sedative drugs, and even deep sleep itself, can cause constricted pupils.”
Being in the dark or dim light and then flipping on bright lights will cause miosis.
One such medical condition, that can cause miosis, is an aneurysm, when it starts leaking.
This does not mean you should become fixated on your pupils and spend time examining them in the mirror because you just read that miosis can be a symptom of a leaking aneurysm.
Additional Information on Aneurysms and Brain Tumors