Acid Reflux – Increases Cancer Risk, Can Affect Throat
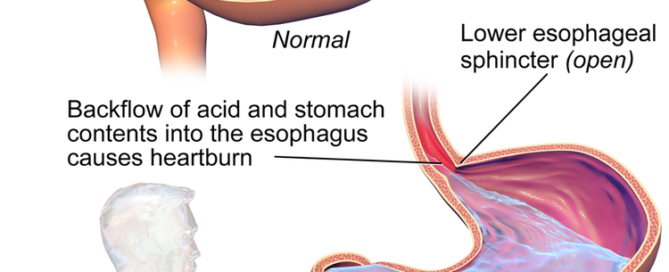
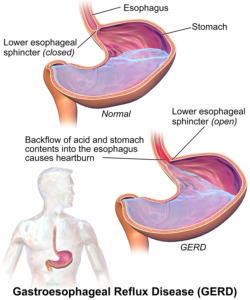
Acid reflux is a very common problem and can cause a number of symptoms, but the most common is “heartburn.”
“Acid reflux is a common condition which produces heartburn and chest pains,” says Natasha Fuksina, MD, an internal medicine and obesity specialist who combines traditional, integrative and functional medicine to restore health and function.
“It affects more men than woman and is associated with advancing age, smoking and obesity.”
Reflux can ocur due to increased acid production and/or a weak esophageal sphincter muscle that doesn’t close properly, allowing acid to go up the esophagus.
“Rare but feared complication of acid reflux is esophageal cancer (adenocarcinoma) and its precursor, Barrett’s esophagus,” says Dr. Fuksina.
Barrett’s esophagus may result from untreated chronic acid reflux.
This is why you should never blow off the situation with “Oh, it’s just acid reflux.”
Dr. Fuksina explains, “With longstanding damage from acid reflux, the lining of the esophagus — normally consisting of flat squamous cells — can transform into columnar cells — leading to a precancerous condition (Barrett’s esophagus) and possibly esophageal cancer.”
TV commercials for heartburn are typically of a comical nature. This creates the illusion that cancer is nowhere downstream from this common condition.
But once a person develops Barrett’s esophagus, they must receive lifelong surveillance of the interior of their esophagus to catch any abnormal changes in time before they transform into a malignancy.
About one to two percent of cases of Barrett’s turn into esophageal cancer — which has a poor prognosis.
Chronic acid reflux that affects the throat is a risk factor for laryngeal cancer, though that risk is small as well.
Acid reflux that affects the throat on a chronic basis is called LPR: laryngopharyngeal reflux disease.
Symptoms include cough, a hoarse voice, a sore or burning throat, a sensation of a lump in the throat and an unpleasant taste in the mouth.
Not Always a Burning Sensation
However, the discomfort of chronic acid reflux, also known as gastroesophageal reflux disease (GERD), isn’t always a burning sensation.
It can also be described as “pain” by some sufferers — and very bad pain in the chest that can make a person think they’re having a heart attack.
When the throat is affected, this doesn’t mean that there are chest symptoms; sometimes the only symptoms are throat related.
Despite the absence of chest symptoms, however, there may still be acidic contents in the esophagus.
“Treatment includes dietary modifications, weight loss strategies and medications aiming to suppress acid production,” says Dr. Fuksina.
Here are numerous articles about acid reflux — you’ll probably find exactly what you are looking for.
 Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus
Chest Pain: Heart Problem, Indigestion or Pulled Muscle?

Chest pain is the No. 1 reason people head to the emergency room.
But does this mean that most of the diagnoses for these patients relate to a heart problem?
Believe it or not, most are not related to heart disease. Chest pain has common causes that are not related to the heart.
But to play safe, people with unexplained and persisting chest pain, or chest pain upon exertion, should get a prompt evaluation.
Unfortunately, many people who experience this unnerving symptom don’t bother visiting the ER, figuring that it’s a little indigestion and that “it will pass.”
And often, a heart related problem that causes chest pain will, indeed, pass, tricking the person into thinking it was nothing serious.
Chest pain, aching and soreness have quite a few causes; in fact, even cancer can cause chest pain!
This is why this troubling symptom should always be investigated to rule out serious causes.
“Various risk factors must also be considered when evaluating chest pain,” says Waqar Khan, MD, who’s been providing state-of-the-art cardiology services to the Houston area for over 20 years, and is author of “Be Heart Smart: Understand, Treat, and Prevent Coronary Heart Disease.”
“Risk factors that are associated with coronary heart disease include diabetes, high cholesterol, family history of heart disease, history of smoking and high blood pressure,” continues Dr. Khan.
“A patient with two or more than two of these risk factors would certainly need an EKG and further workup to diagnose coronary heart disease or heart attack.”
Additional Risk Factors for Coronary Artery Disease
- Untreated sleep apnea
- Obesity and even moderate overweight, especially an apple shaped body
- Diet high in processed food, especially trans fats
- Excess dietary sodium
- Poor stress management
- Sleeping more than nine hours/night
- Sleeping fewer than six hours/night
- Insomnia
- Lack of exercise
- Sitting too much

Waqar Khan, MD, has a private practice and serves as an affiliate faculty member at Baylor College of Medicine in Houston, TX. Amazon.com/Be-Heart-Smart-Understand-Coronary/dp/1732268606
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Headache Pain: Brain Tumor? Sinus Problem? Stress, Tension?

A headache from a sinus problem can hurt as much as one from a brain tumor.
Headaches from sinus issues, however, are very significantly more common than those caused by a brain tumor.
If you’ve been having persistent headaches but no other symptoms such as nausea, slurred speech, balance difficulties, one-sided weakness, memory problems or confusion, then chances are pretty high that the cause is not a brain tumor.
Headaches are commonly caused by a problem going on with the sinus cavity. And this is a VERY common problem.
Treatment for Sinus Headaches
“Correction varies depending on the cause of your sinus headaches,” says Dr. C. Phillip Amoils, MD, a board certified otolaryngologist with SC-ENT Ear, Nose & Throat Specialists in CA.
“It can be as simple as a short course of antibiotics and decongestants for an infection, or allergy medication plus a decongestant for allergies.
“Should no relief be found, limited in-office dilation of the sinus openings using removable balloon-type catheters under endoscopy can result in relief for many of these patients.
“A few patients with severe chronic sinus obstruction causing severe headaches may need operative intervention in the form of endoscopic sinus surgery and septoplasty in an outpatient setting.
“Mild headaches are often sinus related headaches, but if more severe — consider migraine if visual symptoms are associated with the headache.”
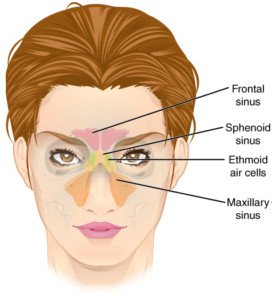
Shutterstock/OpenStax College
My mother was once troubled by headaches that came out of the blue, almost daily.
This can be scary, because some people will automatically fear the worst: a brain tumor.
She went to her primary care physician who referred her to a “headache clinic,” but the doctor at the clinic was not able to figure out what was causing her problem.
Then she saw another doctor (not at the headache clinic) who quickly zeroed in on the cause after ordering an MRI of her head and sinuses, and prescribed a successful antibiotic treatment for a sinus infection.
Oddly, she had not been experiencing any nasal congestion or stuffy feeling in her nose.
Sinus infections can affect different parts of the sinuses and respiratory system in varying ways.
In some cases, the infection may primarily affect the sinus cavities that are not directly linked to nasal passages.
For instance, a sinus infection may cause pressure or pain in the frontal sinuses (located behind the forehead) or the maxillary sinuses (located near the cheeks) without necessarily causing a blockage or thick mucus in the nasal passages.
In such cases, the headache could be the most prominent symptom, with minimal or no nasal congestion at all.
A headache is suspicious for a brain tumor if it’s accompanied by other symptoms (again, balance problems, slurred speech, cognitive changes, one-sided weakness, or vision issues, a bulging eye or nausea/vomiting) — and especially if it does not respond to painkillers.
And it goes without saying: Stress is a leading cause of headaches — the so-called tension type. These can feel a lot like a sinus headache.

Dr. Amoils is considered among the best surgeons worldwide for sinus surgery and OSA, having helped thousands of patients for 30+ years. He also demonstrates to physicians the protocols he’s developed for mouth breathing, nasal congestion, obstructive sleep apnea and snoring using minimally invasive procedures.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
Shortness of Breath: Many Causes like Heart Attack, Cancer

Suddenly experiencing unexplained “shortness of breath” is frightening.
But you need to know that there is a big difference between being short of breath, and having mechanical difficulty getting air down your airway or out when exhaling (“trouble breathing”).
People interchange these two terms all the time, but the experience is very unsettling nonetheless.
Heart Disease vs. Cancer As Cause of Feeling Short of Breath
“Shortness of breath denotes a feeling of insufficient air intake disproportionate with the physical activity,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
For instance, if you run up four flights of stairs, you’re bound to feel short of breath; you will be breathing heavily and faster than usual – but there should not be any problems with the mechanics of inhaling and exhaling.
You’re simply out of breath or “winded.” (More aerobic exercise can solve this problem.)
But a disproportionate feeling of insufficient air intake could be, for example, having to pant to catch your breath when all you did was hurry from one room in the house to the other.
This panting occurs in very out of shape people who are otherwise free of disease. But it also occurs as a result of disease.
“It is a symptom resulting from a wide variety of disorders, often involving lung or heart diseases, but extending far beyond those to include anemia or even psychological disorders,” explains Dr. Tavel.
“Heart disorders cause shortness of breath only when the heart function is decreased to the extent that blood pools in the lungs behind the poorly pumping heart.
“Cancer, on the other hand, generally causes shortness of breath only when directly invading the lungs, or more rarely, when producing severe anemia.
“This breathing problem is less common than that associated with heart failure.”

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
FOOT, HEEL and ANKLE PAIN

Are you suffering from pain in your ankle, heel or foot in general? Foot pain has many, many causes. Some are very serious, too.
The medical specialty that involves treatment of the foot is called podiatry.
A doctor of podiatric medicine (DPM) has completed four years of medical school and after that, has completed the required internships (as all medical doctors do), and then a residency in podiatry.
“Most foot, heel and ankle pain can be attributed to overuse,” says Bruce Pinker, DPM, who specializes in sports medicine and surgery of the foot and ankle.
“Foot pain can often be due to bunion pain, or hammertoe pain (associated with a corn on top of the toe).
“Ankle pain is often due to a sprain or strain from too much activity, especially if running on uneven surfaces.
“Many ankle sprains occur while running or participating in sports or while walking and stepping off a curb irregularly or stepping into a pothole on the street.
“Heel pain is extremely common, often due to plantar fasciitis or a heel spur on the bottom of the heel bone.
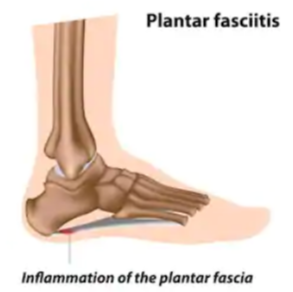
Shutterstock/Alila Medical Media
“The pain is usually due to overuse, as the plantar fascia ligament is elastic in nature and will stretch and contract.
“When it contracts, after inactivity for as little as one to six or seven hours, it contracts and tightens, leading to difficulty walking.
“Usually, conservative treatment resolves heel pain, but some cases can be challenging.
“Physical therapy, orthopedic strappings, cortisone injections and custom-made orthotics often resolve the issue.
“Occasionally, shock wave therapy may need to be utilized, or even surgery, to address the condition.”
Please visit the links below to read numerous articles on foot pain.
 Dr. Pinker is with Progressive Foot Care, which provides state-of-the-art, full diagnostic testing and treatment of the foot. He’s a professional foot and ankle health and wellness speaker who delivers many original seminars annually such as “Keep On Running.”
Dr. Pinker is with Progressive Foot Care, which provides state-of-the-art, full diagnostic testing and treatment of the foot. He’s a professional foot and ankle health and wellness speaker who delivers many original seminars annually such as “Keep On Running.”
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ Elvira Koneva
Fast Resting Pulse in Fit People Who Exercise: Danger

What does it mean if a physically fit person has a fast resting heart rate?
Do you exercise a lot, consider yourself physically fit, but have a fast resting heart rate and wonder if this will negatively affect your risk for all-cause mortality or heart problems?
A resting heart rate of between 60 and 100 is normal. However, the question is this:
Is mortality affected if someone’s pulse is usually around 85 versus 65, even if that person exercises?
Does it make a difference if that individual’s resting pulse is towards the higher end of normal as opposed to the lower end of normal?
Researchers wanted to find out if resting heart rate influenced a person’s risk of mortality, regardless of fitness level.
The Study
For the study, the health of almost 3,000 Caucasian men was tracked for 16 years.
All sorts of vitals were measured, including aerobic fitness (cycling test), height, weight, blood fats, blood sugars and blood pressure. And of course, resting heart rate.
As expected, men who had a high resting heart rate also tended to have the lowest levels of physical fitness, plus hypertension and more blood fats.
Physically fit men tended to have lower resting pulses.
But the results can’t be denied:
The faster the resting heart rate, the greater was the risk of mortality. And this result was independent of fitness level.
What about factors that could influence results? These were adjusted for.
– A resting heart rate of 51-80 bpm was tied to a 40-50 percent increased death risk.
– Between 81 and 90 bpm doubled the mortality risk, when compared to men with the lowest rate.
– Above 90 bpm meant a tripled risk.
Every 10-22 additional bpm increased mortality by 16 percent, overall.
The paper points out that regardless of a study participant’s level of fitness, those with a high resting heart rate fared much worse than those with a lower RHR.
In other words, a high RHR is an independent risk factor for a shortened lifespan.
What should you do?
First off, re-evaluate your exercise habits. It’s a well-known fact that a regular exercise program lowers resting heart rate.
It’s also a well-known fact that many people unknowingly inflate their perception of just how much they exercise.
“I get plenty of exercise” is an assertion spoken by many men and women who — in actuality — don’t even have a regular, consistent workout regimen.
Many belong to the “any movement counts towards exercise” camp.
“Any movement,” to these men and women, may include standing in one spot for 10 minutes tossing a rubber toy for their dog to fetch, or doing basic housework.
This just isn’t enough to effectively train the heart to be more efficient.
A second point to consider, regarding this study, was that the population involved was very limited: white middle aged men.
“So you can’t assume the same would be true for, say, young women from a different ethnic group,” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
Other than fitness, the following factors can affect RHR, says Dr. Beatty:
• Anemia
• Valvular heart disease
• Stress / anxiety / emotional factors
• Hormone factors such as a raised thyroid hormone
• Pregnancy (not relevant to this study)
“It’s conceivable that a few of the study group had one of these problems which in turn might have reduced their life expectancy,” says Dr. Beatty.
“For instance, anemia might be due to bowel cancer which causes premature death.
“Someone with aortic or mitral valve regurgitation might pass their ECG test, done at the start of the trial, but it would put extra strain on the heart as the years go by.
“The result of the trial was very clear-cut, so my overall impression is that there is a correlation between higher heart rate and earlier mortality,” in white, middle aged men.
How to Lower RHR with Exercise
To lower resting pulse, you may want to consider high intensity interval training.
This can be done only twice a week, on any cardio equipment or outdoors.
Here is more about high intensity interval training.
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/VGstockstudio
Source: heart.bmj.com/content/early/2013/03/21/heartjnl-2012-303375.short?g=w_heart_ahead_tab
Great Responses and Comebacks to Being Told “You Look Tired”
If you’re tired of being told by strangers “You look tired,” here are some really clever and feisty responses and comebacks!
But when a stranger says this to me, or to anyone else — it is just plain rude.
It hasn’t happened that often with me, actually, but the few times that it has, it completely caught me off guard, because in every case I was wide awake!
I wonder if the people who will think I’m being too petty are the same people who’d think nothing of swatting the daylights out of a three-year-old child for a minor infraction. Talk about over-reaction!
Great Responses to “You Look Tired”
#1. “Actually, I’m wide awake.”
State this matter-of-factly and then give a neutral gaze to the stranger as that person tries to deal with the embarrassing realization that they just insulted you.
#2. “Yep, I was up all night having really amazing sex. And you look very well-rested.”
#3. “Wow, your powers of observation are stunning!”
#4. “Must be the cancer.”
#5. “And your point?”
#5. “Yep, I’m tired of rude comments by total strangers.”
#6. “Really? Can you explain what it is about my face that looks tired?”
(This will embarrass them perhaps more than the cancer response, as they are now being requested to point out a stranger’s wrinkles, sagging mouth, dark eye circles, etc.)
Being told you look tired should not be ignored.
When an adult makes an inappropriate comment to a stranger, they should be called on this.
If children should be corrected on being ill-mannered, why shouldn’t adults?
You should never feel the stress or pressure to enhance your face before every venture into the public just so you can look wide-awake for strangers.
If I look tired, that’s nobody’s business except that of my loved-ones.
Why would a stranger have a true, sincere concern if you look tired?
I think these are people who are desperate for a social connection and lack the cognitive prowess to come up with anything less lame than “You look tired.” They deserve a good response.
The fact that they mean no harm is beside the point. The child who makes a disrespectful comment to an adult may also mean no harm, yet as mentioned already, most people would be quick to correct the child, some of them going as far as a scolding or even corporal punishment.
So why should ADULTS get away with insolvent comments to strangers?
“You look tired” may, in a very small percentage of cases, trigger a conversation between two strangers in an elevator, in a long line or on a bus. But that’s beside the point.
If you want conversation, say something neutral or make a comment about the latest national headlines.
It’s just plain rude to make a negative comment about a stranger’s face.
You’ll lose nothing by refraining from telling a stranger “You look tired.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Why Do Red Wine Daily Limits Differ for Women & Men?

There’s a reason why the wine consumption recommendations for women are just one glass a day while men get to have two.
That seems unfair, right? If you enjoy red wine and are a woman, you might already know that the American Heart Association, as well as other medical organizations, cite the limit of one glass a day for women…but then raise it to two for men.
Many women weigh as much as the average man, and many men are small in stature and slightly built.
Yet this rule of “one glass of wine a day for women and two for men” stands as universal—a one box fits all.
“Alcohol is metabolized differently in women and men,” says Suzanne Steinbaum, MD, a New York cardiologist for 20+ years and founder of SRS heart — a groundbreaking program for womens’ holistic health prevention.
“In general, women have a smaller amount of body water, and simply adding alcohol to less water saturates the system greater.
“Women also have a lower activity of the alcohol metabolizer in the stomach, causing a larger proportion of alcohol to reach the bloodstream.”
Does this apply to tall, active, muscular women with fast metabolisms, and to short, underweight, inactive men?
Dr. Steinbaum responds, “Clearly, different sizes of people and body types play a role in how the body will respond to alcohol, but in general, women simply can’t process it as efficiently.”
The rule of one glass of wine a day for women and two for men is generalized so that it’s easier to follow, and so that it leaves little room, if any, for confusion or misinterpretation.
Interestingly, this rule rarely comes with the definition of “glass.”
However, here it is: One “glass” of wine = four ounces. That’s half a cup.
The rule, in a more refined presentation, is as follows: Women should limit their daily wine consumption to four ounces, and men to eight ounces.

Dr. Steinbaum has been awarded a New York Times Super Doctor, a Castle and Connolly Top Doctor for Cardiovascular Disease, and New York Magazine’s prestigious Best Doctors in the New York edition. She is on the NYC Board of the American Heart Association.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Best Responses to Why Don’t You Have Kids? & Rude Comments

If you’re childless by choice, ever get asked, “Why don’t you want kids?”
Here are many great comebacks to this never-ending question.
Obviously, “Why don’t you want kids” is asked after the childless by choice woman or man announces that she or he does not want kids. Even people you just meet will ask, “Why don’t you want kids?” upon finding out your choice to stay childfree.
“WHY DON’T YOU WANT KIDS?”
“Not my thing and besides my dog’s allergic.”
“Didn’t you hear? I’m actually due February 30th! I can’t believe no one told you. I’m so excited!!”
“Oh, no one under 14 is permitted in my house. It’s a rule!”
Then there’s the question: Well, what are you going to do when you are old??
“Die, just like everyone else.”
“Hire someone to care for me.”
“Hang out with friends, travel, do whatever I want. The same like now.”
“Pose nude!!”
“No kids, no pets, no plants.”
“When I was kid my mother always told me that when I grew up I would be just like her!”
“WHEN Are You Going to Have Kids?”
“After I make my first billion.”
“When it stops being illegal to leave them alone for 8 hours a day with a cold bowl of water and a toy.”
“When I can stand to be around a kid or a parent for more than 10 minutes without wanting to either kill them or myself.”
One Last Point About Being Asked Why You Don’t Want Children
Sometimes, this question is asked because the person is sincerely interested in knowing your reason, and is not out to judge you.
It could very well be that she — or he — chooses to remain childfree, and is always interested in learning why others make the same lifestyle choice.
There is a difference between being asked, “Why don’t you have children,” (asker doesn’t know if you want them or not), and, “Why don’t you want children” (asker knows you wish to stay childfree).
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Smith Machine 20-Rep Killer Squat Workout for Burning Fat

You’ll burn loads of fat with the 20-rep killer squat workout with a Smith machine.
Though Smith machine squats aren’t the best for building huge quad muscles, this equipment can fire up your body’s fat burning engines.
Smith Machine Workout
Perform 20 parallel (half) squats with a rapid pace. Pay very close attention to your thighs to make sure they actually hit parallel.
The rapid pace may fool some folks into thinking they’re hitting parallel when in fact, they’re falling just short of it. Explode up from each squat.
It’s not necessary to rise all the way back up after each squat. If you come up a little short, that’s fine; your muscles are under constant tension this way.
However, if your style is to go all the way back up, do not lock out the knees and do not hang there, either; immediately come back down into the next squat.
Do the 20 reps as quickly as possible while hitting parallel for every rep and keeping your lower back arched.
At the end of 20 reps, you should be breathless, like you just ran fast up a hill.
Rest 45 seconds and repeat four more times for five total sets, with 45 seconds in between each one.
This doesn’t mean that at the end of 45 seconds is when you step under the bar to get positioned. This means that the time it takes you to get set under the bar is included in the 45 seconds.
These short rests are crucial for maximal fat burning. The breathlessness is also a key feature of optimizing the fat burning process.
And though the routine can be completed in about five minutes, the fat burning will continue afterwards: post-exercise fat-burning.
What if you’re not breathless?
Then the bar didn’t have enough weight on it. You will need to experiment with this. The rapidity of the reps makes the exercise more difficult.
Hitting parallel will also make things harder for people used to doing incomplete half squats.
You should be so out of breath that you can’t complete a sentence.
This Smith machine killer squat routine is NOT for beginners, no matter how badly they want to burn off the fat.
These type of Smith machine squats, with their short rests, are for conditioned people.
Don’t assume that it doesn’t make any difference if you’re a few inches above parallel.
For 20 explosive reps, coming a few inches short makes a whopping difference.
So either use a heavier weight load for the next set (and this may take several sets to figure out; you don’t want to go too heavy), and/or hit parallel for every rep.
If the resistance is too heavy, you won’t be able to explode. You may be able to complete 20 reps, but they’ll lack rapidity and thrust.
The explosiveness yields the cardio component and is key to burning fat.
Though the emphasis is on burning fat, you’ll find that this Smith machine killer squat routine will dramatically strengthen your legs and knees, plus shape and contour the muscles.