WHY You’re Starving the Day After Leg Workout

Okay, you know it happens, but here’s WHY you’re freaking starving the day after a badass leg workout!
You thrashed your legs in the gym, and usually a grueling leg workout includes at least one of two famed compound exercises: the back squat and the deadlift.
But other leg movements can also be very taxing: leg press, hack squat, front squat, weighted lunge, squat overhead press hybrid, and more.
When these exercises are done at intense levels, they drain the muscle cells of their fuel source: glycogen. Glycogen refers to the blood sugar that’s stored in muscle cells.
Muscle cells need this substance for fuel—not just to function, but to recover from a gym thrashing.
If your leg workout is punishing enough, your muscle cells will be left in such a deficit that they’ll be gulping any glycogen that comes along.

Shutterstock/Olena Yakobchuk
Glucose (blood sugar) is transported to the muscle cells via insulin, which is secreted by the pancreas.
The insulin shuttles glucose to the insulin receptor sites on muscle cells—where the transfer occurs, fueling the muscle cells.
If this transport service can’t keep up with the recovery demands of thrashed muscle fibers, then this means that the blood sugar levels are too low.
Low blood sugar will cause hunger.
The day after a leg workout, blood sugar levels may still be low, resulting in crazy hunger.
Athletes who suffer with this often claim that they keep eating and eating, but the hunger persists all throughout the day after their strenuous leg workout.
The supply (food) is not matching the demand (muscles starved for recovery fuel).
But why is this hunger so pronounced the day after the leg workout rather than the day OF the leg workout and leading up to bedtime?

Shutterstock/Photology1971
Though some muscle-building enthusiasts report insane hunger in the hours after the leg workout on the same day, many report that their appetite becomes a bottomless pit only on the day after.
Are you eating enough carbs or is it mostly meat/fish, low carb protein shakes (hardly satisfying) and low carb produce?
When blood sugar gets too low, this causes a signal to go to your brain that translates to FEED ME! I’M STARVED!
If you’re truly cramming down a lot of food and still suffering with hunger, you’re eating the wrong foods.
Processed foods from the supermarket, fast-foods and restaurant foods are notorious for stimulating hunger.
Even if you eat a “heavy” meal of such, don’t be surprised if two hours later you’re famished.
“Fatigue, tiredness, lack of sleep can stimulate hormones that make you feel hungrier than you actually are,” says Carolyn Dean, MD, ND – Medical Advisory Board Member, Nutritional Magnesium Association at nutritionalmagnesium.org.
Solutions to Insane Hunger Day after Leg Workout
• “Recovery from such workouts by supplementing with magnesium and other electrolytes and making sure you get enough sleep for recovery is the best remedy,” says Dr. Dean.
• Loading up on protein and low carb vegetables may fill up your stomach, but will do little to raise blood sugar; hence, you may still feel famished after two chicken breasts and a pile of steamed broccoli.
• Many muscle builders are hesitant to eat more on the day following a leg workout because they’re in a cutting phase or trying to lose excess body fat.
But depriving drained muscle fibers of needed recovery fuel will impede growth.
You must find that right balance, that sweet spot, that subdues raging hunger yet won’t cause fat gain.
• Opt for healthier high carb foods such as naturally sweetened oats, a boiled potato, barley, brown rice, quinoa or geez, even a whole grain (all natural) bagel.
Have protein alongside the carb dense food.

• Plan and be logistical, rather than spontaneous and frustrated.
Have a second potato and a tossed green salad and yogurt an hour later rather than mindlessly cramming down highly processed mac ‘n cheese and an ice cream bar.
• Loading up on water to kill the hunger won’t work. Drink water for its many benefits, but accept the fact that water intake won’t replace depleted blood sugar.
Face it; it’s a part of life: You will likely be crazy hungry the day after a crucifying leg workout!

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monkey Business Images
How an ER Doctor Diagnoses a Transient Ischemic Attack

If you suspect you just had a transient ischemic attack (TIA), get to the ER stat (have someone drive you) so that a doctor can make a diagnosis.
It’s interesting to wonder just how a transient ischemic attack is diagnosed in the emergency room.
After all, when the TIA event is over, which may last less than a minute, the patient may have no symptoms to show for it by the time they get to the emergency room.
“A TIA is, by definition, a transient ischemic attack,” begins Rob Lapporte, MD, who is board certified in emergency medicine.
How a TIA Is Diagnosed in the Emergency Room
Dr. Lapporte continues, “In an ER setting, in order to meet criteria, a patient would have to:
-Have stroke-like symptoms within the last 24 hours
-Have a CT scan that showed no evidence of bleed or infarct, and
-Have complete resolution of his/her symptoms prior to being released from the ER.”
The “bleed” that Dr. Lapporte mentions refers to bleeding in the brain.
A chronic subdural hematoma, which is a common type of bleeding in the brain among the elderly, produces symptoms that are clinically indistinguishable from that of a TIA, other than that they are persistent rather than transient.
A TIA Can Be Misdiagnosed As a Stroke
“Sometimes patients are diagnosed with a stroke from the ER, and the symptoms resolve within a few hours,” says Dr. Lapporte.
“At that point his/her diagnosis would be a TIA rather than a stroke because of the transient nature of the symptoms.”
Symptoms of a TIA (or stroke) include:
#1 Sudden one-sided weakness or paralysis, which can also occur in the face
#2 Sudden-onset double vision, or a sensation that a shade is being pulled over one eye, obstructing vision
#3 Sudden heaviness or numbness on one side of the body
#4 Sudden clumsiness on one side of the body
#5 Sudden slurred speech or difficulty forming words
#6 Sudden cognitive difficulty or understanding speech
#7 Sudden severe headache
#8 Sudden difficulty swallowing
If these symptoms pass after only 30 seconds, this is just as emergent as if they were persisting for two hours.
GET TO THE ER for a proper diagnosis, whether it turns out to be a transient ischemic attack or some other condition.
 Dr. Lapporte has been practicing evidence-based clinical medicine in emergency rooms and urgent care centers for 25+ years. His experience includes that of medical director for Legacy ER and Urgent Care.
Dr. Lapporte has been practicing evidence-based clinical medicine in emergency rooms and urgent care centers for 25+ years. His experience includes that of medical director for Legacy ER and Urgent Care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Blue Planet Studio
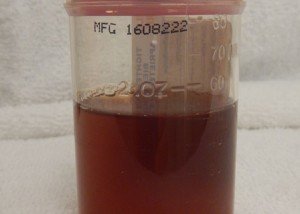
When You Need to Worry About Cloudy Urine: Urologist Answers Questions

If you’ve ever had cloudy urine, you’ve no doubt wondered what’s causing the cloudiness and may have even been troubled by this odd symptom.
After all, is cloudy urine a sign of cancer or some other serious problem?
I interviewed a urologist who specializes in urinary tract infections to uncover all the information you need to know about cloudy urine, such as when it’s time to see a doctor, and what you can do to check if your cloudy urine might mean a viral infection.
It’s important to keep tabs on the color of your urine, so that you’re on top of any changes in the color or appearance, such as cloudy or a murky quality.
I asked questions to Elizabeth Kavaler, MD, a board certified urologist with Total Urology Care in NY, and author of “A Seat in the Aisle, Please! The Essential Guide to Urinary Tract Problems in Women.”
What is the most common cause of cloudy urine?
Dr. Kavaler: Cloudy urine is most commonly caused by inflammation in the bladder. White blood cells, mucous, and debris can build up if the bladder is irritated or inflamed.
The most common cause of bladder inflammation is a urinary tract infection.
Other causes include food irritants, environmental irritants and chemical irritants.
What other variables can cause this symptom?
Dr. Kavaler: Cloudy urine can be a transient event. If irritating foods, like citrus or spices, are ingested, they can cause bladder irritation which will lead to inflammation and cloudy urine.
Once the food is eliminated, the cloudiness will resolve. That is true for viral cystitis, which is when the bladder is irritated by a viral syndrome.
If you have a cold and the urine is cloudy, the urine will clear when the cold clears up.
Certainly, there are people who, upon seeing the cloudy appearance one day, start fearing cancer somewhere, maybe bladder cancer.
Can this ever be a symptom of cancer?
Dr. Kavaler: Cloudy urine is not an indication of cancer. Cancer is indicated by blood in the urine; either obvious blood or microscopic blood that is found on a urine test performed in the physician’s office.

Shutterstock/Eag1eEyes
If cloudy urine is present without symptoms of frequency, urgency or discomfort, it does not need to be addressed.
(The murkiness, in and of itself, is not a notable symptom of a more serious bladder condition.)
Can certain foods cause the murkiness?
Dr. Kavaler: Certain foods, such as spicy foods, citrus and caffeine can irritate the bladder lining and lead to inflammation. The result may be cloudy urine.
Although not dangerous, the inflammation can lead to irritating symptoms.
What causes urinary tract infections?
Dr. Kavaler: Contrary to what some believe, urinary tract infections (UTIs) are not caused by “extra” bacteria getting into the bladder, but by the bacteria that does not get out.
A person with a healthy urine flow should be able to flush all bacteria out of the bladder normally each time they urinate.
A strong and steady flow naturally cleanses the urinary tract and surrounding area of unwanted bacteria.
However, if something is inhibiting normal urination, that’s when bacteria can be trapped inside the urinary tract, leading to a urinary tract infection (UTI).
Can a UTI resolve on its own?
Dr. Kavaler: No, a urinary tract infection can not resolve on its own. It is important to see a doctor as soon as possible.
Your healthcare provider will take a urine culture so that the proper course of antibiotic therapy may be prescribed to cure the urinary tract infection (UTI).
If you are prone to urinary tract infections (UTIs), you should also discuss a uroflow exam (which measures the flow and force of your urine stream) with your physician, as well as talk to your doctor about taking Cystex as a preventative measure.
Drink plenty of water to flush the system and take the over-the-counter (OTC) medication Cystex, as this medicine can help ease the pain of the infection and will not interfere with the antibiotic.

Freepik.com
Antibiotics begin fighting the infection immediately, but they can’t stop all the symptoms right away, such as the pain in your bladder.
When should you see a doctor regarding cloudy appearance?
Dr. Kavaler: If there is cloudy urine with symptoms, see a practitioner.
If there is only cloudy urine, there is unlikely to be a problem, but it is worth mentioning to your physician if it persists.
The physician can be sure that nothing is wrong, such as the beginnings of an infection.
Be sure to also alert your doctor to any changes in the way that you urinate (i.e. flow, pain, and urinary urgency).
Dr. Kavaler adds that if you only have cloudiness and the physician does not find a problem, there is nothing to be worried about.
 Dr. Kavaler and her colleagues at Total Urology Care work to ensure that all patients receive the care and services they need while being treated with the utmost respect. She is double-board certified in urology and female pelvic medicine & reconstructive surgery. Her expertise spans both male and female urological issues, from adolescence to end-of-life.
Dr. Kavaler and her colleagues at Total Urology Care work to ensure that all patients receive the care and services they need while being treated with the utmost respect. She is double-board certified in urology and female pelvic medicine & reconstructive surgery. Her expertise spans both male and female urological issues, from adolescence to end-of-life.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Guschenkova
source: cystex.com
Why It May Be Safe to Lose Over Two Pounds a Week
Yes, it CAN be safe to lose more than two pounds a week as long as you understand some really simple math. And the keyword is “can.”
Certainly, a “starvation” or “crash” approach to dieting is not healthy and can have serious side effects such as fatigue and passing out.
But losing more than two pounds a week does not necessarily require insufficient calories, gimmicks or cutting out entire food groups.
As a former personal trainer, I’ve given the following explanation multiple times to clients about why it can be very safe to lose more than two pounds a week — depending on circumstances.
- There are 3,500 calories in one pound of fat.
- Thus, in order to lose one pound of fat, you must create a caloric deficit of 3,500 calories.
This can occur over a week’s time by cutting back 500 calories per day (7 days X 500 = 3,500).
Lose More than Two Pounds a Week Safely
Suppose on the average, you consume 5,000 calories per day. You decide to go on a diet:
- Controlling your portions
- Avoiding fast-food fare
- Saying “No” to gravies, thick sauces and fried foods
- Cutting back on sugary foods
- Eliminating sodas and replacing them with water
- Eating more fruit, vegetables, salads, beans and whole grains.
Your new eating habits come in at about 2,000 calories per day.
Your body has been used to 5,000 calories a day all this time. Now it gets 2,000.
That means each day, there is a calorie deficit of 3,000 calories (5,000 – 2,000 = 3,000).
Multiply this daily deficit of 3,000 calories by seven days (7 days x 3,000) and you get: 21,000 calories.
This means that each week, with your healthy eating habits, you are consuming 21,000 calories LESS than what your body is accustomed to.
Divide 3,500 calories into 21,000, and what do you get? SIX. This means that you’d be losing six pounds a week of fat!
Yet at the same time, you’re getting adequate calories and nutrients.
The weight coming off is not water, contrary to common belief when large amounts of weight are lost. It’s also not muscle.
After all, 2,000 calories/day are enough to feed your body, assuming that your activity levels aren’t off the chart.
When Losing More than Two Pounds a Week Is Not Safe
How much weight you lose per week depends on variables:
- Resting metabolism
- Pre-existing body composition
- Willingness (or not) to gain lean muscle mass through exercise
- Willingness (or not) to do aerobic exercise
- General overall daily activity level
- Presence of medications or a medical condition
“The guideline to lose 0.5-2 pounds per week is a recommendation based on what is most likely a sustainable weight loss rate for most people,” says Amanda A. Kostro Miller, RD, LDN, whose specialties are nutrition counseling, weight loss and medical nutrition therapy.
“However, some research shows that making drastic changes and losing more than two pounds per week can work for some people as well.”
Remember, “drastic” doesn’t necessarily mean a starvation diet or cutting out major food groups.
“The rate of weight loss may also be dependent on what you are losing,” continues Kostro Miller.
“When our weight drops on the scale, we may be losing fat, water weight or even muscle (which can be dangerous).
“Underlying health conditions can cause us to lose more than two pounds per week, so be sure to be followed by a dietitian and doctor.
“Regardless of where your start in your weight loss journey, small changes can be more manageable than bigger changes. However, everyone operates differently.
“If you consume 5,000 calories per day at baseline, dropping to 2,000 calories per day may be way too much of a step for you,” from a psychological standpoint.
“The sweet spot to weight loss is finding a routine that you can do for the rest of your life (because weight management is lifelong) and one that is actually effective.
“Depending on where you start, drastically decreasing your calories may be dangerous and/or not recommended.
“According to the Harvard School of Medicine, even if you’re trying to lose weight, women should consume no less than 1,200 calories per day.
“Men should consume no less than 1,500 calories per day. Consuming less than these thresholds may actually deter weight loss.”
Amanda Kostro Miller has worked with U.S. veterans, people with eating disorders and those with various acute and chronic diseases.
has worked with U.S. veterans, people with eating disorders and those with various acute and chronic diseases.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Why You Should Brush Your Teeth Before Gym Workouts

Few gym-goers realize how wicked their workout breath smells to other exercisers.
Yes, you read that right: Before stepping foot into your health club or gym, you should thoroughly brush your teeth.
After all, you’re going to be huffing and puffing and breathing heavily near other people. How could they not smell whatever gets exhaled from your mouth?
A better question is how come so few people think about this?
One day I was at the gym pedaling a stationary bike, and with almost every inhalation, I suffered the stench of someone’s breath.
But oddly, nobody was really near me at all. I suspected a woman across the aisle on a bike, but at some point, she left, and I still smelled the odor.
I ruled out the man ahead of me on the elliptical, because he didn’t seem close enough. The woman on my left, several bikes down, eventually left also.
So that left only one person, a man several machines behind me. But he, too, didn’t seem close enough.
But never underestimate the pervasiveness of human bad breath.

Shutterstock/pathdoc
A person with bad breath can actually create a zone of his or her breath that’s a good 10 or 12 foot radius around their body.
But both these men were more than 12 feet from me, and I highly doubted that I could pick up someone’s bad breath whose back was facing me.
Thus, I finally concluded that the culprit was the man behind me…about 25 feet behind me.
I figured that if he was breathing hard enough, it was very possible that I was getting wafts of his breath.
Whom else could it have been? Well, one thing was for sure: SOMEONE had bad breath. SOMEONE didn’t brush their teeth before going to the club. Phooey!
The man eventually left, and so did the odor!
It takes only five minutes before going to the gym to brush your teeth.
Don’t Let Your Breath Stink up the Gym
Even if you’re coming from the workplace, bring with you a toothbrush and toothpaste (keep those always in your gym bag if you have a gym bag) and brush your teeth and mouth at the gym.
Chances are, if you haven’t brushed your teeth for a while, you are going to stink up the air within a 10 foot radius of your body.
“Unfortunately, bad breath (halitosis) can occur at any location, including the gym!” says Marco L. Tironi, DDS, who practices dentistry in Rochester, MI.
The gym workout itself doesn’t directly cause bad breath. A brutal set of deadlifts won’t make your breath stink any more than will a light warmup on a stationary bike.
But a knockout set will leave you huffing and puffing – blowing your smelly breath into the air around other people.
Reasons for Bad Breath at the Gym or Anywhere Else
“Bactera: Bad breath-causing bacteria naturally live in our mouths,” says Dr. Tironi. “When we eat, the bacteria feed on the food left behind in our mouths and give off a foul smelling byproduct.
“Gum disease: Gum disease, which is caused by bacteria, not only is a cause for concern for the long-term health of your gums and mouth, it also causes bad breath.
“Types of food: The type of food you eat affects the air you exhale, even if there aren’t remnants of the food remaining in your mouth.
“Medical conditions: Several other medical conditions can cause bad breath including gastric reflux, diabetes, liver/kidney disease, sinus conditions.
“Dry mouth: If you aren’t producing enough saliva, you may not be able to adequately wash your mouth out. This can lead to bad breath and a higher chance of developing cavities and gum disease.”
It happens all the time.
I’ll be walking past a man who’s on a piece of equipment or one who’s between sets, even, and suddenly, BAM, I get nearly knocked over by a waft of his breath.
Women, too, can have bad breath at the gym.
No matter how hard you work out, there’s just no excuse for this.
Please, everyone who steps into a gym — brush your teeth first!
 A member of the Academy of General Dentistry, Dr. Tironi is trained in sedation dentistry, dental implantology, orthodontics and dentofacial orthopedics.
A member of the Academy of General Dentistry, Dr. Tironi is trained in sedation dentistry, dental implantology, orthodontics and dentofacial orthopedics.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/wavebreakmedia
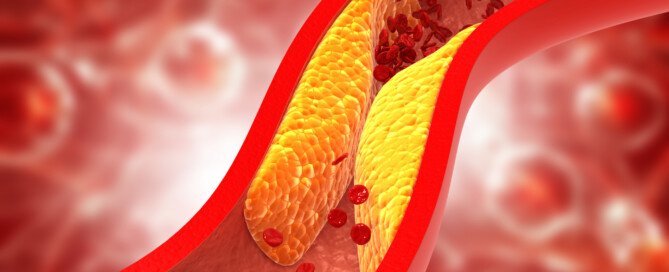
Can You Have Severe Heart Disease but Good Cholesterol Numbers?
It’s actually possible to be a ticking time bomb with severe coronary heart disease while also having a “normal” cholesterol (lipid) profile.
This is why you shouldn’t assume you’re automatically out of the woods just because your cholesterol numbers came back terrific.
Not every heart attack sufferer had bad cholesterol numbers.
Perhaps you’ve heard that about one-half of people who suffer a heart attack have “normal” cholesterol. This brings to mind the interior of coronary arteries looking pretty good. And how can this be?
“Cholesterol is only one risk factor for CAD,” says Pilar Stevens-Cohen, MD, FACC, Department of Cardiology, South Nassau Communities Hospital.
CAD stands for coronary artery disease (a.k.a. heart disease).
“We recognize that it is only part of the picture,” she continues. “Diabetes [prevention of], smoking cessation, blood pressure management are all key factors in secondary prevention.”
Cholesterol Defined
“It’s a moving target,” says Dr. Stevens-Cohen. “When I was training, the bad cholesterol target was under 100.
“Now we say less than 70. Do we know how low to go? We also now recognize that LDL is only part of the equation.”
LDL is the “bad” cholesterol: high density lipoproteins.
“Newer tests, NMR [nuclear magnetic resonance spectroscopy], evaluating particle size [of LDLs], may be more helpful in managing patients than actual LDL levels.
“A person can seemingly have a good cholesterol panel, but when you do specialized testing, you see that their particle size is shifted and you should be managing them more aggressively.”
The bigger the LDL particles, the more desirable. A person can have normal cholesterol numbers, but if the particles are very small…this can mean heart disease — which can ultimately lead to an attack.
Another reason a person with normal cholesterol could have a heart attack is due to atrial fibrillation, an arrhythmia that can cause blood clots to form in the heart.

Dr. Stevens-Cohen is board certified in cardiology, nuclear cardiology, echocardiography and internal medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Explode
Why Even One Crumb of Gluten Is Harmful for Celiacs

Just one crumb of gluten may as well be an entire loaf of bread to someone with celiac disease.
Celiac patients can’t even have a tiny crumb; that’s all it takes to trigger their immune system into attack mode–on their own body!
Celiac disease is not like heart disease or diabetes, in which an offending agent (i.e., saturated fats, refined sugars) can occasionally be eaten without damage to the body.
In celiac disease, foods containing gluten must be eliminated 100 percent, down to the last crumb.
In fact, so strict must the elimination of gluten be, for people with celiac disease, that they should also avoid using cutting boards that gluten-containing bread was placed upon.
I wondered why those with celiac disease can’t occasionally eat something with gluten.
It’s as though the body can’t differentiate between an occasional pretzel and multiple daily servings of bread, cereal and pasta.
I was thinking of this as an “all or nothing” approach, which isn’t fair to people with celiac disease.
“Actually, it is all or nothing when it comes to eliminating gluten,” says Nicole Kuhl Visnic, CCN, a dietitian and nutritionist in Santa Monica, CA.
“When a person with celiac consumes gluten, there is an immune cascade that is occurring in the body, even if there are no obvious GI symptoms.”
In other words, the occasional pretzel may not cause any observable reactions in the celiac patient, such as diarrhea or upset stomach, but something unseen and unfelt gets triggered.
“For every patient with CD, there are eight patients with CD and no GI symptoms,” says Kuhl Visnic.
The immune response to this protein is so strong, that a person with celiac disease must avoid non-gluten foods that were prepared in the same facility as gluten foods are.
A pizza with a wheat flour crust, consumed after being gluten-free for 12 months, really will make a difference in the patient.
Kuhl Visnic explains, “The reason a little bit of gluten is harmful is because people with celiac disease have hypersensitivity to gluten. Kind of the way a light switch turns the light on or off, gluten turns the immune system on or off.”
In celiac disease, the body thinks that this protein is a foreign invader, and this faulty recognition triggers an immune attack on the protein molecules.
Eating gluten-containing foods means a chronic immune response that, over time, damages the inner lining of the small intestine, impairing its ability to absorb important nutrients.
This malabsorption leads to a litany of medical problems including brittle bones.
But can just one occasional pretzel in an otherwise gluten-free diet cause such damage?
Kuhl Visnic says, “Another way to think about it would be to consider the effects of adding a couple drops of cyanide to a glass of water. A couple of tablespoons would be more toxic than a couple drops, but a couple of drops is still toxic.”
The presence of the wheat protein in that tiny pretzel will activate “T cells,” which are the body’s defense against foreign invaders.
T cells then release certain chemicals that would be valuable in the event of a microbial attack.
But in the presence of gluten, T cells that are activated harm the intestinal cells that are responsible for nutrient absorption.
So if someone has celiac disease and you can’t understand why he or she thinks “one little bite” will indeed hurt, Kuhl Visnic explains, “The immune cells in someone with CD sit on the intestinal epithelial cells ready to pounce, as soon as gluten is recognized,” in any amount.
 Nicole Kuhl Visnic specializes in custom-designed diets tailored to the individual and has worked with numerous celiac disease patients.
Nicole Kuhl Visnic specializes in custom-designed diets tailored to the individual and has worked with numerous celiac disease patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Mia Stern
Negative Celiac Blood Test, but Stool Sample Shows Antigliadins

What if the blood test for celiac disease is negative, but a stool sample is positive for elevated antigliadins?
Was your celiac blood test negative, but a stool sample positive for elevated antibodies for gluten?
]And suppose you don’t have symptoms that can be ascribed to celiac disease. What should you do?
How telling is that stool sample that shows an immune response to gluten? Gliadin is a component of gluten, and antigliadins are the antibodies.
Celiac disease cannot be diagnosed based on a stool sample.
However, a stool sample showing elevated antigliadins definitely means that an immune response is occurring to gluten.
This doesn’t necessarily mean celiac disease; it can also mean mere gluten intolerance.
A person can have the gene/s for celiac disease and gluten sensitivity; different genes are involved.
The elevated antigliadins can be the result of the gluten-sensitivity genes expressing themselves, not the celiac disease gene/s expressing itself.
If the person does not have symptoms, it gets trickier, since the symptoms will start vanishing once gluten is eliminated.
“Research is continuing to show that antibodies are predictive of certain degenerative diseases including celiac disease,” says Nicole Kuhl Visnic, CCN, a dietitian and nutritionist in Santa Monica, CA.
“Anti-transglutaminase antibodies are one type of antibody that may indicate a predisposition to celiac disease.
“However, there are other antibodies and markers such as antigliadin, glutenin, and gluteomorphin that may show up sooner than anti-transglutaminase antibodies.
“These markers alone are reason enough to eliminate gluten. Unfortunately, anti-transglutaminase antibodies are related to mucosal damage.
“Waiting for anti-transglutaminase antibodies to show up on the labs before you take action is like sticking your head in the sand.”
Transglutaminase refers to the blood test.
“The preventative medicine field has advanced greatly by way of lab testing. Cyrex laboratory has a new test for gluten sensitivity that is far more sensitive than stool tests.
“Doing this kind of test is important because it is not likely that an individual will take dietary restrictions seriously without ‘proof.’ Continuing to eat gluten, even small amounts, provokes an immune response that perpetuates the disease process.”
Can a person have celiac disease if the transglutaminase test is negative, but the stool sample has antigliadins?
Kuhl Visnic explains, “No. There are typically three steps taken to establish diagnosis for CD. The first step is a blood test (including transglutaminase), the second is biopsy of small intestine, and the third is implementation of a gluten-free diet.
“If the small intestine returns to its former healthy state following a gluten-free diet, a diagnosis is made.
“It’s important to understand that diagnoses are made late in the game. Celiac disease is a result of ongoing damage that has progressed to the disease stage.
“In the prevention model of health care, the goal is to prevent the damage from ever occurring.
“This is why it is prudent to avoid gluten if you have positive markers for gluten sensitivity.”
 Nicole Kuhl Visnic specializes in custom-designed diets tailored to the individual and has worked with numerous celiac disease patients.
Nicole Kuhl Visnic specializes in custom-designed diets tailored to the individual and has worked with numerous celiac disease patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Scorpp
Fast Resting Heart Rate Increases Death Risk from All Causes

An elevated resting heart rate is associated with an increased risk of death from all causes. This includes cardiovascular disease.
Are you familiar with what your pulse normally is when you’re at rest? If not, you’d better get familiar with it — because research shows that it’s a risk factor not to be ignored.
This is the conclusion by researchers from the Ronald O. Perelman Heart Institute at New York-Presbyterian Hospital/Weill Cornell Medical Center; over 9,000 patients were studied.
This conclusion applies to tracking resting heart rate over time.
Study authors urge doctors to track the pattern of patients’ HRs over the years, rather than relying upon a single reading.
The Study Is Something to Think About
“Based on this study, we believe that an elevated heart rate seen over a number of years is worrisome, signifying that these patients need further evaluation to see what might be causing the high heart rate,” says lead investigator and cardiologist Dr. Peter Okin in the paper.
The researches followed patients for an average of five years, and found that readings of 84 beats/minute or more were associated with a 55 percent higher risk of cardiovascular death, as well as a 79 percent higher risk of all-cause death.
Cardiovascular risk factors such as hypertension were adjusted for.
Normal RHR should be between 60 and 80 beats/minute according to some cardiologists, while others extend that range to 100 bpm.
- A 16 percent greater risk of death from cardiovascular disease, and a 25 percent increased risk of death from all causes, came with every extra 10 beats/minute greater than normal resting heart rate.
Why would an elevated resting heart rate be associated with more cardiovascular disease anyways?
Faster resting heart rate increases automatic nervous system activities, and this heightened response is connected to increased risk of atherosclerosis (plaque buildup inside arteries) and abnormal heart rhythms, as well as heart ischemia (restricted blood supply).
“Heart rate remains a significant predictor of increased mortality,” says Dr. Okin in this report.
Should you panic if your resting pulse is frequently over 80 and especially 102 or so?
Most cardiologists are not concerned if a patient’s resting pulse is between 80 and 100 — especially if that patient shows no signs of cardiac abnormality elsewhere and reports no concerning symptoms.
But what if many times when you take your pulse, it’s a little above 100 — even though you’ve been at rest for a while?
“The resting heart rate range can be deceiving,” says Yaser Elnahar, MD, a cardiologist with Hunterdon Cardiovascular Associates in NJ, whom I interviewed for this article.
Dr. Elnahar continues, “The best way to look at this data is to evaluate resting heart rates in young professional athletes (40-60 beats per minute) — since their hearts are well-trained and more efficient at pumping the same amount of blood at less work.
“In people who exercise regularly, don’t smoke and don’t consume much caffeine, I would question the hydration, weight and any other medical conditions that are causing the fast resting heart rate.”
If such an individual keeps well-hydrated, tests negative for medical conditions, is of a healthy weight, restricts caffeine and doesn’t smoke — yet STILL often has a resting heart rate on the fast side (e.g., 102 or even in the 90s), then it’s quite possible that this person has too much anxiety going on.
Leading a stressful life can keep the heart rate on the fast side for extended periods.
The patient may be a jumpy or edgy type of person who can’t really maintain calmness for too long. Something is always up, giving that person the jitters.
The complete study is in the July 2, 2010 online European Heart Journal.
 Dr. Elnahar has publications in the Journal of Atrial Fibrillation, the Journal of Clinical Medicine and Research, Reports in Medical Imaging, and more.
Dr. Elnahar has publications in the Journal of Atrial Fibrillation, the Journal of Clinical Medicine and Research, Reports in Medical Imaging, and more.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Freepik.com
Source: sciencedaily.com/releases/2010/08/100812151640.htm
Does High Cholesterol Mean You Should Take Statin Drugs?
If you have high cholesterol, statin drugs may come to mind as something you must necessarily take.
As to whether or not high cholesterol is an automatic green light for taking statins:
“Absolutely not! Since half the people with high cholesterol never have heart disease, we are overprescribing medications with significant costs and side effects,” explains Dr. Larry Santora, MD, a cardiologist with Orange County Heart Institute and Research Center, and author of “OC Cure for Heart Disease.”
Dr. Santora continues, “If you have high cholesterol and a zero coronary calcium scan, you can safely be treated with diet and exercise for five years.”
My brother’s coronary calcium score was not zero (he won’t reveal the number), but he did say that the score prompted him to “aggressively” treat his condition, and the treatment includes a statin.
My mother never had a coronary calcium scan; she had a catheter angiogram which revealed near-complete blockage in all major coronary arteries – she underwent quintuple bypass surgery only a few hours after the angiogram.
Immediately after, she was put on a statin and continues to take the statin today. Her cholesterol profile, pre-surgery, was poor.
It has since improved significantly, despite no change in eating habits.
Dr. Santora continues, “On the other hand, if you have normal cholesterol, but one other risk factor like diabetes, etc., you may be one of the potential heart attack victims who has normal cholesterol.
“If you get a heart scan and have plaque or calcium, being on cholesterol meds will reduce dramatically the heart attack risk.”
Risk factors for heart attack that many people cannot name are: sleep apnea, insomnia, less than six hours of sleep a night, chronic mental stress, insulin resistance or pre-diabetes, and excess belly fat even though the rest of the body is not “overweight.”
Dr. Santora adds, “The new paradigm approach for cholesterol should be: 1) This person has high cholesterol; can this patient get a heart scan and not be put on medications?
“2) This patient has normal cholesterol; should this patient be on cholesterol medications?
“The $300 or less for a scan will more than pay for the savings in medications and lives.”
Even if your insurance will cover the cost of statins, statin drugs serve up a lengthy list of possible side effects, some of which are serious (though rare).
Why would a person with normal cholesterol, but a high calcium scan score, be put on a statin?
Because statins are also designed to slow the progression of coronary plaque buildup.
Many natural supplements have the same cholesterol-lowering effects of statins, such as vitamin B3 (niacin), plant sterols, aged garlic extract, fish oil, green tea extract and turmeric.
Exercise also has the same effect, especially intense exercise.