Walking vs. Medication for Type 2 Diabetes to Lower Sugar

Wow, it’s now been shown that walking, in the form of a daily step count, is at least as good as medication for lowering blood sugar in type 2 diabetes.
This happens when a doctor writes a prescription – not for a drug, but for a daily step count – and hands it to the diabetic patient.
A very clever study comes from the Research Institute of the McGill University Health Centre.
Dr. Kaberi Dasgupta already knew that regular walking can bring a 40 percent reduction in vascular event rates in a 10 year period for type 2 diabetics.
But Dr. Dasgupta says in a report in Diabetes, Obesity, and Metabolism that merely telling patients “to be more physically active simply doesn’t work.”
The directive of “be more physically active,” or something similar like “get more exercise” is way too abstract for a sedentary person who’s drawn to spending large amounts of time in a chair or couch.
Dr. Dasgupta, principal author of the study, says that the objective of the study was “to use step counts almost as a medication.”
She specializes in prevention and management of blood vessel disease in diabetics and those at risk for diabetes.
For years, she’s been intrigued by the concept of counting daily steps and how this impacts health.
Counting steps eliminates the hassle of keeping track of distances or times.
The counting is done with a pedometer, absolving the patient from any conscious tracking other than to periodically check the pedometer to make sure they’re on course for completing a minimal number of steps by bedtime.
The Step Counting Study
• 364 patients and 74 doctors representing different Montreal hospitals
• Some patients had written prescriptions for step counts and were given a pedometer.
• One year later it was found that the patients who’d been given the step count prescriptions had taken 1,200 more steps per day, on the average, than the patients who’d not been given the prescription.
• It’s amazing what difference a piece of paper can make, though the pedometer certainly helped as well. The other patients were merely TOLD to walk more.
• Patients with type 2 diabetes, on the step count prescription, lowered their glucose levels.
This is the first study showing that a written prescription for taking more steps can benefit health.
Hmmm, what if a prescription was written for strength training?

Freepik.com
It would have to be very specific, since “do strength training” is far more abstract than “get in 10,000 steps a day and this pedometer will record your steps.”
But perhaps a prescription for strength training can come with a tension band and illustrated instructions for the band!
I’d love to see a study on how effective this would be for people with type 2 diabetes or other kinds of patients including healthy who are simply having their annual physical.
At least 10,000 steps a day is recommended for all people, not just those with type 2 diabetes.
Under 5,000 steps a day is a potential forerunner of developing this metabolic disorder as well as suffering from vascular events like a transient ischemic attack.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos.com
Feeling off Balance after Treadmill Walking: Causes, Solutions

There’s basically one reason why you feel off balance after stepping off the treadmill, but there’s more than one solution to this benign problem.
First of all, when I was a personal trainer at a health club for several years, I worked with many treadmill users.
What I found was that in 100 percent of the cases in which a person reported feeling off balance or “dizzy” upon getting off the treadmill, that individual had been HOLDING ONTO the machine.
Before you assume that you have a medical problem that causes you to feel off balance after getting off a treadmill, I recommend you break the habit of holding on.
New to Treadmill Walking?
If you’re new to using this machine, the best time to break a bad habit is when it hasn’t yet become a habit. Do not hold on.

Start out slowly. Don’t feel you must jack the incline up to 15 percent, the speed at 4 mph, then grip the front bar and yank with each fake step. I see this all the time and it’s ridiculous and worthless.
Cause of Feeling off Balance after Walking on Treadmill
If you’re holding on, this deactivates your body’s balance mechanism. It’s like flipping off its switch. There is no need to balance if you’re holding on. It’s that simple.
So — you’re walking for, say, half an hour, even 10 minutes, all while your internal balance device is switched off (because you’re holding on).
You then step off the treadmill. Bam! Your body’s balance device is suddenly switched back on and must work immediately.
This causes that off balance feeling. It’s a sudden transition from total deactivation to total reactivation. It takes your body several moments to adjust.
But what if you haven’t been holding on yet still feel balance issues after you get off the treadmill? And what if this is the only time you feel this strange dizziness?
Quite simply, your body is not used to walking on a moving tread belt.
However, your body will quickly adjust to this.
But I’m betting that near 100 percent of people who feel dizzy or unsteady after walking on a treadmill were holding onto the machine.
Remove your hands for your next session.
Use a slow speed.
Avoid high inclines until your body acclimates.
I had senior citizens and obese beginners walking on the treadmill without holding on.
I even had a client with Meniere’s disease (which causes unsteadiness and dizziness) walking without holding on.
Walking on a treadmill without holding on will improve your body’s internal balancing device!
Model: Sharon Smith, 71 years young.
Sharon Smith has been in the fitness industry for 25+ years and specializes in the over-40 client.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Treadmill HIIT: Will Time Taken Switching the Speed Interfere ?

It’s entirely possible to do a blistering HIIT workout on a treadmill without having to worry about time being used to switch the speed settings.
Having to switch the speed settings will NOT interfere with HIIT on a treadmill. (more…)
Steady State Cardio vs. HIIT for Congestive Heart Failure

The question isn’t just if HIIT is safe for congestive heart failure patients, but does it improve the function of their heart better than steady state cardio. (more…)
MRI Breast Cancer Screening for Non-Dense Breasts? Why Not?

If the MRI is so sensitive to picking up cancer in very dense breasts, why shouldn’t women with non-dense or fatty breasts ALSO benefit from annual MRIs?
After all, MRIs can pick up a lot of things that mammograms (and ultrasounds) can’t.
A study from Germany says that MRI screening makes early diagnosis more possible in women with average breast tissue – women at average risk – and this means non-dense breasts.
Traditionally, the MRI has been recommended only for women at high risk for breast cancer.
This imaging tool has never been the one of choice for women with average risk of breast cancer, even though mammograms have a 20% “miss” rate for women with average risk of disease.
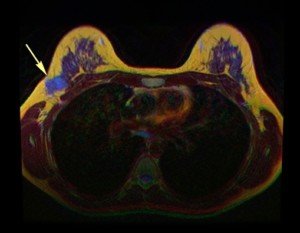
The arrow in this breast MRI points to cancer. © Nevit Dilmen/CreativeCommons
MRI Study: Intriguing Results
Christiane Kuhl, MD, decided to pursue the efficacy of MRI for detecting breast cancer in “regular” breasts.
- The impact of MRI on 2,120 women, 40-70, was studied.
- The women had been determined to have a less than 15 percent lifetime risk of disease.
- The women’s mammograms were normal.
- Women with dense breasts also underwent ultrasound with normal results.
Disturbing Discoveries
- MRI of the subjects detected 60 cancers.
- This translates to a detection rate of 15.5 per 1,000 women.
- The study, which appears in the Feb. 2017 Radiology, also revealed MRI’s superiority over ultrasound.
With about 240,000 women in the U.S. every year getting diagnosed with breast cancer, why isn’t MRI as standard as the mammogram – even if a woman is willing to pay out of pocket and doesn’t mind lying inside the equipment?
Dr. Kuhl’s paper points out that MRI finds malignant tumors that mammography would eventually find – but that MRI detects them sooner.
The report also notes that if the MRI had not been done, those additionally-caught masses would have progressed to interval cancers.
Interval masses refer to those that the patient or doctor discover with the fingers in between imaging procedures.
The earlier that breast cancer is caught, the more curable it is. So why then, aren’t MRI’s routine for non-dense breasts?
“This study was evaluating average-risk women, meaning, those with background lifetime risk (12%, 1/8 over the course of their lifetime), with non-dense breasts and history of normal imaging,” begins Anjali Malik, MD, a board certified diagnostic radiologist with Washington Radiology in Washington, DC., who was not involved in the study. She interprets mammograms, breast MRIs and ultrasounds, and performs biopsies.
“Screening examinations are meant to be accessible, easy, quick, cheap tests with good sensitivity and specificity to detect a disease that, when caught early, is curable.
“This study clearly demonstrates the excellent specificity and sensitivity of contrasted breast MRI.
“However, the cost, limited accessibility (less centers, magnets and techs for MRI, length of time, even if abbreviated, due to IV placement, checking renal status), and risk (gadolinium contrast is not without risk) make MRI a poor screening examination for those with average risk.”
Issues with MRI
- If a woman with non-dense breasts and no other high risk factors doesn’t mind lying in the “tube” and paying out of pocket, she can still pursue a breast screening MRI for her peace of mind. But she also needs to know that MRI has a much higher false-positive rate than do mammograms.
- All people who undergo a contrast MRI must be injected with the gadolinium dye.
- If the patient has compromised kidney function, they will be refused the procedure because the chemical dye is toxic to the kidneys.
- Furthermore, in very rare cases, the patient has a life-threatening allergic reaction to the dye.
- So overall, it’s not efficacious for MRI to be a routine screening procedure for women with non-dense breasts and average risk.
“Thus, it is reserved for those women with increased lifetime risk for the development of breast cancer, where MRI certainly has a place as part of a high risk breast cancer screening protocol,” says Dr. Malik.
For example, a woman with non-dense breasts but who’s positive for a BRCA mutation would be a candidate.
A woman with heterogeneously dense breasts whose sister was diagnosed with the disease would also be a candidate for MRI screening.
 Dr. Malik is a frequent public speaker and advocate for breast health awareness. She has lectured on the latest advances in breast cancer screening including 3D Mammography™. Follow her on Instagram: @AnjaliMalikMD
Dr. Malik is a frequent public speaker and advocate for breast health awareness. She has lectured on the latest advances in breast cancer screening including 3D Mammography™. Follow her on Instagram: @AnjaliMalikMD
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/tugol
Source: sciencedaily.com/releases/2017/02/170221080523.htm
Carpal Tunnel Wrist Brace: Hand Falls Asleep at Night: Solution

If your hand falls asleep at night from a wrist brace for your carpal tunnel syndrome, there’s a cause & solution, straight from a carpal tunnel doctor. (more…)
Can You Suddenly Get Carpal Tunnel Syndrome in Both Hands ?

Sudden carpal tunnel syndrome in both hands is also referred to as “acute bilateral” carpal tunnel syndrome.
And yes, this can happen: A person can develop sudden-onset carpel tunnel syndrome affecting both hands in a simultaneous fashion. (more…)
Can Carpal Tunnel Syndrome Cause Pain in the Entire Arm ?
Carpal tunnel syndrome can cause pain in your entire arm, but not without the help of another neurological disorder.
To relieve the whole arm pain, you must have both conditions treated. (more…)
Which Burns More Fat? Running Level Courses or Walking Hills?

The question of “Which burns more fat, walking hills or running on level land?” is too broad a question to say one or the other burns more fat. (more…)
Exercise Guidelines for TIA Patients: Transient Ischemic Attack

The idea of starting an exercise program after suffering from a transient ischemic attack can be daunting to some patients.
People who’ve had a TIA will often wonder if it’s safe to exercise.
A TIA (transient ischemic attack) is a mini stroke, or, to put it another way, a temporary stroke, caused by a blood clot that chokes off blood supply to part of the brain.
TIA symptoms (weakness or numbness or heaviness on one side of body, unsteady gait, loss of balance, vision disturbances, severe headache, slurred speech, confusion) will last a few minutes to up to 24 hours, then spontaneously resolve.
However, the disappearance of TIA or transient ischemic attack symptoms does not mean all is well.
Since high blood pressure is a major risk factor for stroke, and exercise increases blood pressure, you absolutely must delay your next workout session until you have had clearance from a cardiologist to resume (or begin) exercise.
“Exercising in individuals who may have had a TIA is dangerous,” says Teresa Caulin-Glaser, MD, a cardiologist and senior vice president with Service Lines, OhioHealth.
“It is important for individuals to understand that TIAs associated with even brief periods of ischemia (symptoms) can cause permanent brain injury.
“If you have had symptoms of a TIA, you are at increased risk of a stroke.
“Anyone with a new symptom that may be suggestive of a TIA needs urgent evaluation and treatment, since immediate intervention may substantially reduce the risk of a significant debilitating stroke.”
If you had a TIA but don’t get treatment, and then exercise or physically exert yourself (heavy yard work, roughhousing with grandkids, taking out garbage, etc.), the blood pressure increase from the physical activity can outright cause a stroke — not necessarily another TIA, but a full-blown stroke.
But does this mean that exercise is permanently off-limits to a person who had a transient ischemic attack?
“Exercise at a moderate level of intensity is beneficial to individuals who have had a TIA once the patient has been treated and cleared by their physician to begin an exercise program,” says Dr. Caulin-Glaser.

Source: cancer.gov
“It is important to remember, if a patient has cerebral vascular disease they are at higher risk for also having coronary artery disease, and therefore beginning an exercise program should be initiated only after physician assessment and approval.”
What about people, who were already regularly exercising, prior to the TIA?
Dr. Caulin-Glaser explains, “The individuals still have newly diagnosed vascular disease, and as such should have a stress test with an exercise prescription stating the appropriate heart rate ranges for exercise.
“The stress test will confirm their blood pressure and heart rate responses to maximal exercise are appropriate on the new medications.”
Must people with a TIA history permanently par back on exercise intensity, even if their blood pressure is under control?
Dr. Caulin-Glaser says, “It may not be necessary to par back; the stress test will help make the determination on what is the appropriate level of exercise for each individual.
“Increasing awareness and education regarding the safe approach to a great exercise program is not a limitation, but an endorsement for them to continue lifelong exercise.”

Dr. Caulin-Glaser is an experienced physician, teacher and researcher in the specialty of cardiovascular disease, and formerly the system vice president for Heart & Vascular Services at OhioHealth.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.