Can a Brain Tumor Cause a Swooshing Noise in the Ear?

The potential causes of a swooshing noise inside the ear can be deadly.
When someone begins noticing a “whooshing” sound in their ear, a brain tumor is often the first possible cause that comes to their mind. (more…)
Vaginal Odor from Menopause: Causes and Solutions

Fact is, there is nothing inherent about menopause that causes unpleasant vaginal odors.
Some women have a tendency to immediately blame menopause when something goes awry with their body.
Though menopause is associated with dozens of symptoms, this doesn’t always mean that this “change” is a direct cause of those symptoms or issues.
Causes of Vaginal Odor: Not Menopause
“Vaginal odor can be due to infections such as bacterial vaginosis or other vaginal or uterine infections,” says Mylaine Riobe, MD, founder of Riobe Institute of Integrative Medicine. Dr. Riobe, board certified in OB/GYN and integrative medicine, is the author of “The Answer to Cancer.”
“Odor can also be caused by poor diet and increased toxicity,” says Dr. Riobe.
Now of course, a woman can become depressed upon learning that she’s going through menopause or having the knowledge that she’s just completed menopause, and is now officially “postmenopausal.”
And what can depression lead to? Less attention to personal hygiene — which includes bathing the feminine areas of the body.
Lack of cleanliness can certainly lead to an odor “down there.”
In addition to an unpleasant odor, which can sometimes have a fishy smell to it, bacterial vaginosis can also cause a new-onset discharge.
If you’re experiencing other symptoms with vaginal odor, such as new-onset painful intercourse or a burning sensation while urinating, see your gynecologist.
Infections can be easily treated, but can become very problematic if not promptly treated.

Dr. Riobe has helped thousands of patients overcome difficult illnesses by addressing root causes, not just masking symptoms. The Riobe Method focuses on the prevention of disease, not the prevention of death from disease. She has 20+ years’ experience using integrative techniques to treat diverse patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Why the Leg Press Will Never Make Your Thunder Thighs Worse

Ever notice that women with thunder thighs don’t usually do leg presses, and the women who do a lot of leg presses have sleek firm thighs?
Is this because women with thunder thighs avoid the leg press like the plague, believing it will make their legs even thicker? (more…)
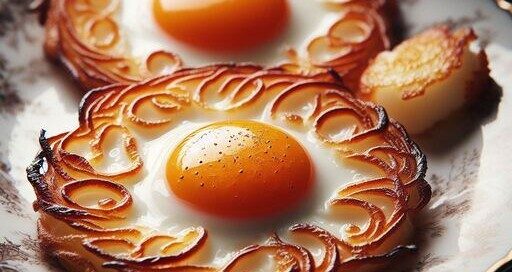
Whole Eggs vs. Egg Whites for Building Muscle: Comparison

Yes, it makes a BIG difference whether you eat whole eggs or egg whites after training to pack on muscle, even if the amount of protein in grams is identical.
Study: Egg Yolks vs. Egg Whites 18 Grams after Lifting Weights
The difference in protein synthesis, when one eats 18 grams of whole eggs vs. egg whites after a muscle building workout, is significant, says a simple study.
The difference is 40 percent more protein synthesis, even when both study groups consumed the same amount: 18 grams.
The report (American Journal of Clinical Nutrition, Dec. 2017) recommends ditching the habit of chucking the yolks when preparing the post=workout omelet or fried egg sandwich.
“Egg whites are great for building muscle because they’re nearly a pure source of protein, while also having little to no fat or carbs,” says Sara Artigues, a registered dietician and certified personal trainer out of New Orleans.
“However, egg yolks also provide about 2.7 gm of protein [each] with extra nutrients that can be even more beneficial to muscle growth.
“While whole eggs contain more calories from fat than protein, this dietary fat can slow protein absorption.
“Thus, eating the whole egg may help you feel more satisfied longer.
“The egg yolk contains various beneficial vitamins like B’s, A, D, E and K as well as calcium and iron.” The yolk also contains a potent antioxidant, selenium.
“This study suggests that eating protein within its most natural food matrix tends to be more beneficial to our muscles as opposed to getting protein from isolated protein sources,” says the study paper.
Including the yolks will not make a bodybuilder or physique athlete gain fat or prevent getting cut for a competition.
If you’re worried about more egg yolks raising your bad cholesterol or adding plaque to your heart’s arteries — you may want to get regular lipid profiles and see if the addition of whole eggs worsens the profile.
Refined carbs are worse for your cardiovascular system than are whole eggs.
If you’re eating three whole eggs in a fried egg sandwich on Wonder white bread, you should be a lot more concerned about the bread.
Study Format
• 10 young men trained with weights, then ate whole eggs or the whites.
• Either way, the protein content was 18 grams.
• Subjects received infusions of amino acids that allowed the researchers to measure the levels of amino acids in the subjects’ blood and muscles.
• The eggs that were used in this study were isotopically labeled with the amino acid leucine for precise tracking of the amino acid levels.
• Blood and muscle biopsy samples were taken multiple times to reveal where the amino acids, from the eggs, were showing up in the blood and muscles.
It’s About Protein Synthesis
It was greater in the participants who’d eaten the yolks – greater protein synthesis immediately after the weight training when compared to those who’d had only the whites.
Though some bodybuilders and physique athletes avoid yolks in the name of stripping body fat, they will want to seriously reconsider this move – and consider other ways to knock down the body fat percentage — such as cutting back on refined carbs or portion sizes of unhealthy food.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
 Sara’s training services include fitness/body composition assessments, nutrition planning, customized programs and spin class instruction for a variety of clients.
Sara’s training services include fitness/body composition assessments, nutrition planning, customized programs and spin class instruction for a variety of clients.
.
Source: sciencedaily.com/releases/2017/12/171220122054.htm
Can a Woman Be Too Old for a Ponytail? Not These Ladies!
If you can sport a badass ponytail, then there’s NO such thing as a woman being too old to wear a ponytail!
Check out the big fluffy ponytail below. The woman’s face told me she was in her early 60s, possibly mid 60s.

The wrinkles on her face in NO way take away from the fact that this ponytail steals the show.
One of the objections to older women wearing ponytails is that the pulling back of the hair reveals every little wrinkle.
Well, if a woman’s face has wrinkles, you’ll know this even if she has bangs and hair framing her face. You can’t hide an aged face with hair unless it’s literally swallowing up the face.
I see women all the time with hair loose and down and framing their face – yet this does not diminish the appearance of wrinkles or sagging.
So if you think a ponytail will make you look older just because you have wrinkles across your forehead or sagging cheekbones, you’re mistaken.

However, from behind, a big gorgeous ponytail will take years off a woman. The golden ponytail above is being rocked by a woman who appeared to be 85, possibly 90.
As she slowly moved with her walker while using portable oxygen, her youthful billowing ponytail was an attention-grabber.
Now here’s another woman (below) who is far from being young … yet her cascading grey ponytail can’t be ignored!


And another long cascading grey ponytail on a mature woman.


I’m in my 50’s and always wear my hair in a ponytail. I’ve been doing so for many years and never once ever considered that I was too old. Below is my big fat ponytail. I just love it.

Remember, there are other features that will make a woman look “old.”
• Sun damaged skin
• Untoned muscles, flab
• Bad posture
• Shuffling or lazy gait
• Poor diet, not enough water
Don’t think for a second that wearing a ponytail will make a woman look older!



However, if you’re still concerned about the pulling back revealing aging skin, why not wear bangs with the ponytail?
You can also grow some hair lower down on your hairline to frame your face a little.
A woman asked in a forum if 33 was too old to wear a ponytail. I don’t know what kind of hair she has, but come on, if 33 is too old for a ponytail, then what’s the cut-off? 29? 31? 27? 27 and a half?
Granted, some hair textures just don’t make good ponytails. But even young women, teens and grade school kids can have thin wispy hair.
• Thin limp ponytail on a 19-year-old woman
• Big poofy ponytail on a 50-year-old woman
• Which will look better?

More Ponytails of Older Women Below





















Senior Age Men with a Full Ponytail


A grey or white voluminous ponytail is quite striking, especially when it’s long.
But regardless of color, there is no age limit to wearing a ponytail.
If you’re an older woman who’s been reluctant to put your glorious hair in a ponytail — either because it’s grey, white or someone said you were “too old,” just DO it anyways!
Hair Loss
Hair loss can result from removing a fastener from a ponytail. Here’s how to take out a thick ponytail without pulling out your hair.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
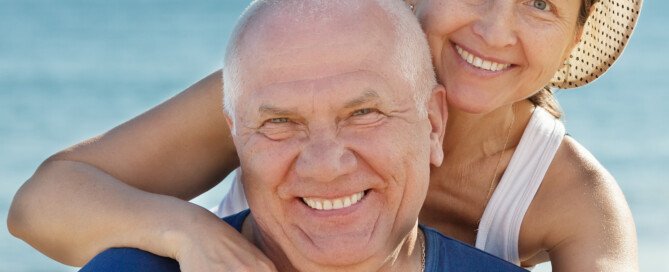
Yoga vs. Cardio Exercise for Heart Disease Patients
When yoga is compared to cardio (aerobic) exercise as part of heart disease treatment, which is better?
Yoga and cardio exercise are both very beneficial forms of physical activity for healthy people as well as those afflicted with heart disease, but is one better than the other for heart disease?
A study found that when yoga was undertaken in addition to cardio exercise, the ensuing benefits were greater than when only one of these forms of exercise were undertaken.
However, the study did not pit yoga alone against aerobics alone.
In fact, there is little to no data showing, from a medical or scientific standpoint, which of these disciplines provides more benefits to a person with heart disease.
We only know that the sum is greater than the parts.
If you have heart disease, don’t choose between yoga and cardio. Do BOTH forms of exercise!

Study Results
In October (2017) the study results were presented at the 8th Emirates Cardiac Society Congress in collaboration with the American College of Cardiology Middle East Conference in Dubai.
When heart disease patients practiced both yoga and cardio workouts, they enjoyed twice the reduction in their blood pressure, body mass index and cholesterol levels when compared to those who did only one or the other.
The 750 patients in the study were obese and had type 2 diabetes, which are two major risk factors for coronary artery disease, which they were all diagnosed with at the start of the study.

• One group did cardio.
• Another did yoga.
• A third did both.
The yoga-only and aerobic-only groups had similar reductions in total cholesterol, LDL, triglycerides, blood pressure and body mass index.
The yoga AND cardio group had a two-times greater reduction than the other groups, plus a big improvement in left ventricular ejection fraction and exercise capacity.
Yoga can be done following an aerobics session, as your body will already be warmed up and looser from the increased blood flow.
Or if you prefer, you can do yoga and aerobics on separate days.
Tips for Treadmill Users
- Do not hold on. Otherwise, you’ll be mimicking the use of a walker.
- For momentary balance checks, yes, hold on, such as when drinking water, but otherwise, let your arms move naturally.
- Incline walking is just as beneficial to the heart as is level walking, and vice versa. It comes down to personal preference.
- Feel free to jog if your knees agree.
- If you can’t walk/jog without holding onto the treadmill, then the speed is too fast and/or the incline is too high.
Tips for Those New to Yoga
- If you have heart disease, don’t hesitate to start yoga no matter how stiff you feel.
- Yoga moves can be modified for stiff, de-conditioned bodies.
- Do not be “intimidated” by yogis who can bend like pretzels.
- Your heart will thank you!
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
,
Top image: Freepik.com, beerfotos
Source: sciencedaily.com/releases/2017/10/171019100951.htm
Why You Shouldn’t Be Screened for Sleep Apnea if You Don’t Have Symptoms

Since millions have undiagnosed obstructive sleep apnea, shouldn’t EVERYONE be screened for OSA, even if they don’t have daytime symptoms?
Voiding a Lot of Urine Overnight: Could Be Sleep Apnea

Is your sleep interrupted by the need to urinate, and a LOT of urine usually comes out, even if you avoid liquids for hours before bedtime?
Sleep apnea could be the reason.
Studies linking untreated sleep apnea to having to get up in the middle of the night more than once to urinate have been around for several years.
But it isn’t just a link. There is an explanation.
There are many reasons why the urge to urinate wakes someone up more than once overnight, forcing them out of bed.
Sometimes the urine output is low, which may indicate nighttime overactive bladder, a prolapsed bladder or an enlarged prostate.
But what if you keep peeing and peeing large amounts, even though you abstain from fluids for several hours before going to bed?
This is susepct for untreated obstructive sleep apnea.
Why does sleep apnea cause a lot of urine overnight?

This has nothing to do with the sleep apnea causing someone to wake up several times, and then — as long as they’re awake, they simply decide they may as well visit the loo.
It’s an issue of a full bladder that needs to be emptied.
When sleep apnea goes untreated, it results in more urine production.
“While there are many mechanisms at play, the most relevant involves the production of atrial natriuretic peptide (ANP), which is a protein produced by certain muscle cells in the heart,” says Daniel Rifkin, MD, a sleep medicine expert at the Sleep Medicine Centers of Western New York.
“The exact reason why an increase in production occurs remains suspect, but an increase in intrathoracic negative pressure (trying to breathe against a closed throat creates a vacuum in your chest!) stretches some of those cells — and your heart falsely thinks that it’s due to too much blood volume.
“The frequent slowing and speeding up of your heart with apnea events also tricks the heart into thinking it’s working too hard.
“So, increasing ANP tells the kidney to diurese, or urinate, to reduce the volume.
“I tend to see this more commonly in severe sleep apnea than in the milder forms.”
A Study on Sleep Apnea and Urine
CPAP treatment reduces the frequency of nighttime urination, says a Dutch study which was presented at the European Association of Urology conference in London in the spring of 2017.
Dr. Sajjad Rahnama’l from the Maastricht University Medical Centre studied 256 patients who wore a CPAP mask for their obstructive sleep apnea.
Prior to treatment, 69 percent reported having to urinate more than once a night.
After starting CPAP, 65 percent of that 69 percent reported a reduction in peeing frequency.
When Treatments Don’t Work
If you’ve been experiencing “overactive bladder” despite a multitude of treatments (drugs, nutritional supplements, Botox injections, acupuncture, pelvic exercises), you may want to ask your doctor about the possibility of sleep apnea — even if you’re not obese.
The kidneys are supposed to be pretty much turned off during sleep so that we can get uninterrupted sleep for optimal restoration.
 Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
Dr. Rifkin is board certified in both neurology and sleep medicine. He also treats insomnia, RLS and narcolepsy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/cliplab
Sources:
sciencedaily.com/releases/2017/03/170327083455.htm
doctorstevenpark.com/sleep-apnea-and-nighttime-urination
Can a Virgin Man Get an HPV Infection ?
HPV is highly contagious and can lead to numerous cancers including that of the penis. So if a man’s never had sex, could he still get infected with this common virus?
SUDDEN Onset Sensitivity of Some Teeth: Causes, Solutions