Is Just ONE Cigarette a Day Harmful to Your Health?

Are you down to only one cigarette a day and think you’re off the hook from any harmful effects?
Just how “light” a smoker can you be before this habit starts ruining your body?
Some smokers like to think that their number of cigarettes per day falls below a threshold, above which the habit then starts causing harm to the heart, lungs and other systems.
How many smokes a day?
Few people smoke only two or three, let alone one, cigarette a day — as a chronic habit.
Many who are trying to quit will taper down to just a few, and eventually one, cigarette a day.
But those who want to keep smoking usually go through at least half a pack on a daily basis. Certainly, there are exceptions, e.g., those who smoke four or five cigarettes a day.
But just ONE a day as a regular habit? Not likely.
One Cigarette a Day Is Still Enough to Significantly Raise the Risk of Clogged Arteries
The British Medical Journal (January 2018) says just one cigarette a day increases the risk of coronary heart disease and stroke enough such that smokers should quit 100 percent. Not even one smoke a day.
The risk of developing heart disease and stroke from one cigarette a day is HALF as much as with 20 cigarettes a day. HALF. Gee, that’s still pretty bad.
The Study
• Professor Allan Hackshaw at the UCL Cancer Institute at University College London led the investigation.
• The results of 141 studies were analyzed including the relative risks for smoking one, five or 20 cigarettes a day.
The Results
• Men who puffed on only one cigarette a day had 46 percent of the increased risk for blocked arteries that men who smoked 20 cigarettes a day did. That’s about half of something really bad.
• The risk for stroke was 41 percent.
• For women, it was 31 percent for heart disease and 34 percent for stroke when compared to women who smoked 20 cigarettes every day.
One a Day
One cigarette a day may seem like nothing. But 365 cigarettes a year mean a lot to the body: a lot of bad things.
There is no safe level of smoking.
“We know that smoking contributes to all stages of development of atherosclerosis, including endothelial dysfunction and thrombus formation,” says says Natasha Fuksina, MD, an internal medicine and obesity specialist who combines traditional, integrative and functional medicine to restore health and function.
“Smoking causes inflammation and oxidation of low-density lipoprotein cholesterol which causes heart disease.
“Research shows that cigarette smoking increases oxidative stress as a potential mechanism for initiating cardiovascular dysfunction.”

Shutterstock/Bogdan Vija
It’s always a perfect time to kick the habit!
 Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick.
Source: sciencedaily.com/releases/2018/01/180125230308.htm
Can a Sleep Disorder Be Causing Your Child’s ADHD?
If your child’s been diagnosed with ADHD, you should first have a sleep study done on them before you start doling out the ADHD drugs.
When adults don’t get enough sleep, the most obvious symptom is drowsiness.
Kids who do not get restorative sleep may seem to have energy during the day, but their symptoms of inadequate sleep can mimic those of ADHD.
It’s no secret among pediatricians that many of their young patients who’ve been diagnosed with ADHD experience behavior improvement once their sleep quality is improved.
If your son or daughter has been diagnosed with ADHD, or you’ve been told by a school counselor that “he probably has ADHD,” there is no rush to get a drug prescription.
Take some deep breaths and consider the possibility that sleep-disordered breathing is responsible for the hyperactivity, lack of focus, short attention span, etc.
“I agree that poor sleep quality can imitate ADHD symptoms,” says Dr. Lisa Lewis, MD, a board certified pediatrician in Fort Worth, Texas, and author of “Feed the Baby Hummus, Pediatrician-Backed Secrets from Cultures Around the World.”
“When screening a child for symptoms of ADHD, sleep quality is a top question that should be asked.
“It is important to know whether their child snores, sleeps fitfully, has insomnia or gets a good night’s sleep.
“If the parents are unsure, they should observe the child at night.
“Symptoms to observe for are significant snoring with restless sleep.
“It also helps to log how many hours’ sleep they get at night, daytime fatigue and whether they are difficult to awaken in the morning.
“If the tonsils are enlarged, it never hurts to get an opinion from an ENT (ear, nose and throat) doctor to ensure the enlarged tonsils are not obstructing the airway at night.
“Also, children with ADHD who have difficulties sleeping at night or insomnia tend to have heightened symptoms of ADHD during the day.”
Never assume that your child can’t have sleep-disordered breathing just because he or she is thin.
Other Things for Parents to Watch for While Their Child Is Sleeping
- What appears to be strained or forced inhalation or some other issue with breathing.
- Constant movement and adjustment of their body and arms; frequent fidgeting. The child never attains a prolonged phase of appearing peaceful and STILL.
- Pauses in their breathing. Watch the rising and falling of their stomach. Does it remain in the “fallen” position for too long?
- When breathing finally resumes, is it noisy? This is especially a red flag for a sleep disorder.
If anyone has told you that your child might have ADHD, or, if you yourself have come to this conclusion, the first doctor your child should see is a pediatrician who’s knowledgeable of obstructive sleep apnea.
This may be a general pediatrician or a pediatric otolaryngologist.
Ultimately, a full evaluation by an ear, nose and throat physician may be in order, along with a sleep study.
Having 25+ years’ experience, Dr. Lewis completed her pediatrics residency at Texas A&M University Health Science Center, Scott and White Memorial Hospital. For two years afterward she was assistant professor in the department of pediatrics at Texas A&M University Health Science Center.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
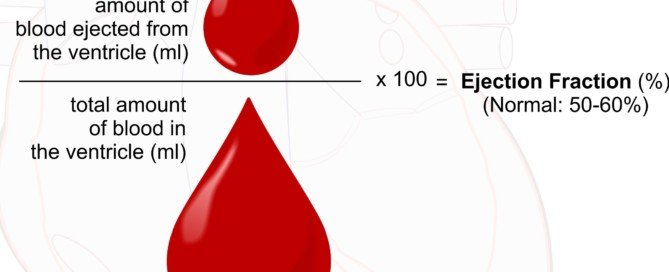
The Lowest Ejection Fraction a Person Could Live With?
How is it that some will have acute heart failure with an ejection fraction of 15% and die, while others are quite alive with a much lower ejection fraction?
I was inspired to write this article after reading posts on a site for heart failure patients.
People were saying their ejection fractions were 10 percent, eight percent … even five percent. None were saying they were dying or in hospice.
Meanwhile, people with ejection fractions in the 20s have been known to suffer acute decompensation and die.
- What’s going on here?
- Just how low can ejection fraction get before it becomes fatal?
- Is there more to survivability than just that number?
“That’s a tough question to answer,” says Mark Pool, MD, a board-certified cardiothoracic surgeon based in TX who’s been in private practice since 2011.
Dr. Pool continues, “I would liken it to asking, ‘How fast could a motorcycle rider go on the highway?’ Lower is worse for ejection fraction, just like faster is more dangerous on a motorcycle.
“But there is no specific speed at which all motorcycles will crash. There is no ejection fraction that means automatic death.
“I’ve seen some patients with an ejection fraction of 10 percent who thought they were fine — minimal shortness of breath or foot/ankle swelling — and I’ve had patients with terrible shortness of breath and swelling with an ejection fraction of 20 percent.
“I’m not sure why that is, other than the human body is very adaptable, and some people can get used to a low EF and not have many untoward bodily effects.”
Why can a person with an EF of 15 percent suffer liver and kidney injury due to poor cardiac output, while others are living their lives with ridiculously low ejection fractions?
Sure, they may have chronic renal insufficiency (e.g., stable creatinine between 2 and 2.5), but that’s the key word: stable.
“This is unclear to me, too!” says Dr. Pool. “Why are some people seven feet tall and some five feet tall? Genetics, hormones, etc., etc., but it is still a bit unclear, because differences exist within siblings; same with heart failure.”
Keep in mind that someone who claims an ejection fraction of five percent and is not in hospice is probably under age 65. Well under.
A younger body, just in general, is better able to compensate for a very badly functioning organ.
Which heart would you rather have? One with an EF of five percent or one with an EF of 15 percent? Well, the answer is obvious.
But what if you then learned that the one with the EF of five percent is 45 years old, and the one with the EF of 15 percent is 90 years old? Don’t bet the farm on that higher EF, 90-year-old heart.
Another explanation for why someone could be surviving with a super low ejection fraction is because of the filling volume of their heart chambers before each beat.
Ejection fraction is not an absolute number.
A patient with an EF of five may still have a greater output of oxygenated blood per minute than a person with an EF of 15 or even 20.
Remember, EF is a percentage of the blood pumped out of the heart, not an absolute amount.
Five percent of a moderate amount of blood can be more than 20 percent of a small amount.
In other words, how much blood is in the heart before each ejection of blood factors into how adequately or poorly the organs are perfused.
“Yes, there are physiologic factors that may account for failure or success clinically when it comes to a set low EF,” says Dr. Pool.
“That is why attention to salt intake and fluids and medications are very important.
“There must be factors that are poorly defined that allow one person to do okay with extremely low ejection fraction but another person to struggle with a modestly low EF.”

Dr. Pool performs some of the most complicated and high-risk heart surgeries in North Texas, including redo operations and multi-valve surgery, and has performed over 3,000 major operations.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ellepigrafica
Heart Failure Cause Liver & Kidney Failure at the Same Time?

Heart failure can cause liver failure AND kidney failure, but what are the odds that the liver and kidneys decide to fail at the exact same time?
Is it more likely that heart failure injures the liver first, and then the liver injury causes a reduction in blood flow to both kidneys, thereby making both of them fail? (more…)
Can Ascites Cause Acute Decompensated Heart Failure?

Are you wondering if excess abdominal fluid, called ascites, can cause an already weak heart to be strained, leading to ADHF?
And if so, would this be due to a mechanical type of pressure or just what, exactly? (more…)
Why Can ADHF Occur at Any Time in Chronic Heart Failure?

A fully functioning patient with CHF who’s medically stable, although with chronic renal insufficiency, could have acute decompensated heart failure at any time.
There are people with chronic heart failure who go dancing, bike riding, even hiking.
It’s scary to think that at any time, with seemingly no triggers, they can acutely decompensate. (more…)
5 Percent Ejection Fraction without Acute Renal Failure?

“For unknown reasons, some patients are able to tolerate very low ejection fraction without failure of other organs” including the kidneys, says Dr. Mark Pool, MD, a board-certified cardiothoracic surgeon based in TX who’s been in private practice since 2011. (more…)
Can the Liver Suddenly Fail Acutely from Heart Failure?
There are several mechanisms by which you can suffer acute liver failure as a result of your chronic heart failure.
The kidneys get virtually all of the attention in medical literature when it comes to organ damage secondary to heart failure. (more…)
Does Fluid Buildup Always Occur with Acute Heart Failure?

Can ejection fraction suddenly get a lot worse (acute heart failure) without filling the lungs with fluid or causing peripheral edema?
When people are hospitalized with acute decompensated heart failure (ADHF), is this commonly because of respiratory distress from fluid buildup in the lungs? Yes. (more…)
How to Eliminate the Spinach Taste in a Spinach Smoothie

I accidentally discovered a way to greatly blunt the spinach taste in a spinach smoothie despite loads of spinach in the blend!
Recipes for spinach smoothies often call for small amounts of this green superfood because it’s quite unpalatable in liquid form for many people.
But there IS a way to cram a LOT of spinach into a smoothie.
In fact, here’s a way to create a large smoothie that’s virtually ALL spinach — without hardly tasting any of it. No kidding!
And why make a spinach-full smoothie if you don’t want to taste the spinach?
Because this vegetable is a superfood: full of health-giving nutrients.
How to Practically Neutralize the Spinach Taste Despite a Ton of Spinach in Your Smoothie

Use a NutriBullet or NutriNinja processor. This recipe will not work with “juicers” or juice extractors.
Place an apple slice or small amount of any other non-leafy produce at the bottom, as depicted in the image above.
This will prevent spinach leaves from sticking to the bottom (which becomes the top when you flip it over to process).

Cram as much spinach as possible up to the black limit line of the container.
You can breach this rule a little, as I’ve done here, as I’ve done in the image above.
Don’t just drop in the leaves. Cram and stuff them down with your fingertips so that the volume is compact.
Cram as much as possible up to or a little past the black line. Then add a small palm-full of raw almonds.

Add water to a little past the black line or marker. Then turn on the NutriBullet or NutriNinja.
Let it grind away for at least 60 seconds. The machine will NOT overheat or malfunction.
You want to be sure to completely pulverize the almonds and leaves. The result will be a rich green color.
I like to pour the contents into a very large glass, like the huge stein shaped glass below.
There will be a LOT to drink, due to the required water content.
If you don’t add enough water, the drink will be thick like a shake. If you prefer this, then fine.
But I like to get green smoothie ingestion over as fast as possible, and the only way to accomplish this is to have a thinner drink so that I can easily guzzle a lot in a long breath.

Add one and a half tablespoons of the following to the drink (which can be purchased in ground form):
- GROUND chia seeds
- GROUND flaxseeds
- The seeds do not have to be processed by the NutriBullet or NutriNinja. They will easily mix into the processed product.

Ground chia seeds (above)

Ground flaxseeds
Stir vigorously with an object that reaches the bottom of the glass, such as a butter knife. If it seems too thick (not easily “guzzable”).
Then add water and stir in. It’s never too late to add more water to thin out the beverage.

Now I’m not exaggerating when I say this, but you will hardly — and I mean barely, if at ALL — taste the spinach.
So what, then, will you actually taste? First of all, the taste will be highly tolerable. It will totally lack that unpalatable, awful taste of earth and mud that some people describe as the taste of liquified spinach.
Depending on what other produce you put at the bottom (to prevent the leaves from sticking), it will be a bland, weak taste, almost like nothing.
If you use grapes instead of an apple, you’ll taste the grapes, not the spinach, and the drink will have more flavor, but it will still be weak.
With an apple slice, it will almost be neutral, actually. It will not taste like cardboard or paper.
Trust me, you will easily tolerate it. You will not have to plug your nose as you drink this spinach smoothie, nor will you dread your next sip or guzzle.

Strangely, it will not taste nutty or seedy. You may detect a vague taste of almonds.
But what happens is that the almonds and seeds cancel out the taste of the spinach, and the spinach cancels out the taste of the almonds and seeds. It’s really strange, but it works.
You can now drink large amounts of spinach without ever gagging on the taste ever again!
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.