The answer to why old people are at higher risk of falling goes way beyond “because they’re old and weak.”
In fact, there are fall risks that most people would never even consider when wondering about this question.
Many Causes of Falls in the Elderly: Some Very Surprising Causes and Risks
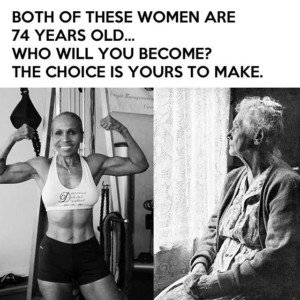
If you don’t begin a serious strength training program by age 30, you will lose about five pounds of muscle per decade after that: 20 pounds of muscle lost by age 70. Muscle loss begets bone loss.
But it doesn’t have to be that way! Risk of falling is incompatible with a hardcore strength training program.
A significant risk factor for falls in the elderly is the absence of weight workouts.
Check out the senior age women below. Who’s more likely to take a bad fall?
There’s also a decline in the neuromuscular system — what I, as a former fitness instructor, call the “recalculation system.”
If you stumble over the edge of a bunched-up carpet or as a result of knocking your leg into the side of a chair, a fit healthy body will instantly “recalculate” to prevent a fall.
This system regresses as the body ages, so that a simple stumble becomes a hard fall to the floor.
“Muscles involved in maintaining our balancing ability are diminished; therefore, statistically we become more at risk of injury or death from falls after the age of 65,” says Dr. Tom Carpenter, corrective exercise specialist, certified personal trainer and chiropractor, inventor of Stand Corrected™, a portable harness-like stretching tool that helps alleviate back, neck and shoulder pain.
The aforementioned variables are the more obvious causes of falls in the elderly.
But following are factors that increase the risk of falls in older people – and some will surprise you.
Cognitive Impairment, Including Mild
The increased risk may be directly from impaired cognition (e.g., changes in brain matter will reduce the ability to recalculate) or indirectly (e.g., not recognizing the hazard of walking fast on ice).
“Falls are a major health problem for older people and are more prevalent in those with cognitive dysfunction,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
“The exact causes of falls in such people have not been well studied, but those with reduced mental function also manifest poor physical fitness resulting from lack of regular exercise,” continues Dr. Tavel.
“Poor physical fitness and muscular weakness are well-recognized risk factors for falling, and these factors alone could explain these events in mentally impaired persons.
“Reduced mental function per se could also play a contributing role, but to an uncertain degree.
“We are encouraged, however, by recent exercise interventions that result in increased gait speed, strength and balance, and these measures have demonstrated significant benefits in reducing falls in cognitively impaired people.
“Moreover, some evidence suggests that regular exercise may even retard or mitigate the progression of cognitive impairment, which could then prevent the development of a ‘vicious cycle’ of decreased physical fitness and deteriorating brain function.”
Sciatica
A sudden sciatica attack (acute nerve pain) can drop an elderly person who’s in poor musculoskeletal condition.
This happened to my mother and resulted in a fractured hip.
Chronic Pain
A report in the Journal of the American Medical Association links chronic pain to increased risk of falls in the elderly.
“Our results suggest that pain should be added to the list of risk factors for falls,” states Suzanne Leveille, PhD, RN, in the paper.
She continues that “persons who have chronic pain in two or more joints, and those who have moderate to severe pain or disabling pain, are at significantly higher risk.”
Reduced Blood Flow to the Brain
A report in Neurology notes that by 85, just 18 percent of people can walk normally.
Small changes in cerebral blood flow (caused by high blood pressure) mean a higher risk of falling in senior age people.
“Blood pressure affects blood flow in the brain and may cause falls,” says study author Farzaneh A. Sorond, MD, in the paper.
Going Barefoot or Wearing Socks or Slippers
A study by Marian T. Hannan, co-director of the Musculoskeletal Research Center at the Institute for Aging Research, found that 52 percent of the elderly participants were not wearing supportive footwear at the time of their fall.
“On the basis of this and other studies, we suggest that advice about wearing shoes whenever possible be included in fall prevention programs,” says Dr. Hannan in the study report.
The higher risk of falling when not wearing supportive footwear is clearly related to the aforementioned diminished neuromuscular control and muscle atrophy.
Poor Vision but Also New Glasses
“Older frail people may have greater difficulty adapting to such changes [large changes in spectacle prescription] and be at increased risk of falling during this adaptation period,” explains David B. Elliott, PhD, in Optometry and Vision Science.
Unaccustomed improvement in vision may cause objects to appear closer or farther than they really are, affecting the elderly’s reflexes linking the balance system with eye movements.
Many Medications
Being on multiple medications is far more likely in someone with compromised mental faculties and/or physical issues that impair recalculation.
“Polypharmacy” (five-plus drugs a day) is also linked to frailty.
The more drugs that one takes, the more likely that adverse interactions will result that lead to frailty, delirium and greater risk of falling.
Blood Pressure Drugs
An elderly person may be on only one drug — for high blood pressure — and be at increased risk for falling due to faintness from a dip in blood pressure.
A report in JAMA Internal Medicine notes that the risk for serious falls was higher in people on blood pressure drugs vs. not on them.
Medications that Disrupt Balance
“Side effects from certain medications can affect our balancing abilities as we age,” says Dr. Carpenter.
For example, a study from the University of Colorado at Boulder showed that the sleep drug zolpidem impaired balance in older people, upping their rate of falls.
Nocturia
Nocturia is having to get up in the middle of the night more than once to use the toilet. Many elderly people are up at least three times overnight to relieve themselves.
This problem is more prevalent in the elderly due to higher rates of chronic heart failure—which is treated with diuretics that cause increased urination.
It’s also more prevalent due to incontinence and untreated sleep apnea.
So what does urinating overnight have to do with falling?
It’s simple: An elderly person who’s unstable on their feet is more likely to fall the more often they’re on their feet — and trips to the toilet overnight often occur in the dark and/or while groggy.
Arrhythmia
Elderly people are more likely to have a heart arrhythmia episode, which can cause dizziness or fainting.

Photo credit: Aleesia Forni
Based upon 30+ years of experience, Dr. Carpenter’s practice approach reflects his belief that restoring optimum health and function will enable his patients to enjoy a much greater amount of vitality and wellness. Chiropractic care is true health care, not sick care!










































