Can Microdiscectomy Be Performed Under Regional Anesthesia?
If you need a microdiscectomy but are not suitable for general anesthesia, this procedure CAN be done using regional.
You may fear general or be a poor candidate for it, but this doesn’t mean you can’t undergo a microdiscectomy with regional anesthesia.
“Lumbar spinal surgery, especially a microdiscectomy, may be performed under regional anesthesia,” says spinal and orthopedic surgeon Kenneth K. Hansraj, MD, who specializes in minimally invasive spine surgery, laminectomies and spinal fusions, and is author of the book, “Keys to an Amazing Life: Secrets of the Cervical Spine.”
He continues, “Usually however, the anesthesiologists use a short-acting fentanyl to assist with analgesia.”
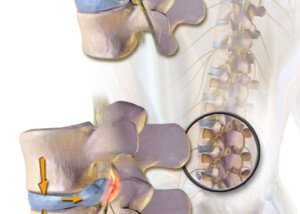
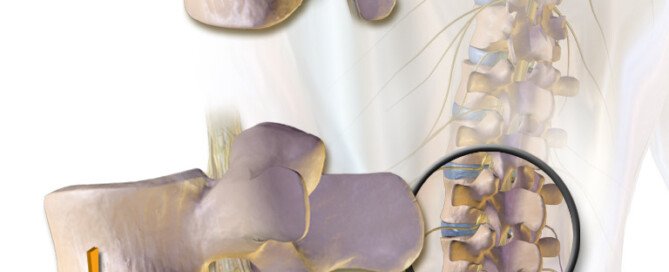
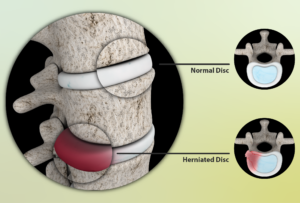
Herniated Disc Surgery
An Internet search may not bring up a lot of information on regional anesthesia being used for a microdiscectomy—a procedure that involves removing the portion of a lumbar disc that’s herniating (protruding out) from its natural space.
Thus, you may think that your only option is general.
“Lumbar microdiscectomy surgery is already performed under spinal anesthesia (SA) in many institutions,” states an abstract from a study (Dagher et al).
Another study (Papadopoulos et al) concludes: “Epidural anesthesia as an alternative to general anesthesia has shown less post-operative nausea and vomiting in lumbar microdiscectomy.”
Contraindications to herniated disc surgery under general include advanced age and severe heart disease.
More About Microdiscectomy
The procedure may be performed by either an orthopedic or a neurosurgeon.
A small portion of the bone over the disc material under the nerve root and/or nerve root is removed.
The surgery is been shown to be more effective as a general rule for relieving leg pain rather than low back pain.
In the case of leg pain, the relief is usually felt almost immediately after the procedure.
However, numbness or weakness symptoms may take weeks or even months to subside.
The microdiscectomy has been around for quite some time, and hence, many spine surgeons are very experienced with it, making this a reliable operation for nearly immediate – and sometimes outright immediate – relief of leg pain from nerve root compression.
Ask your physician about regional anesthesia, as there should be no reason why this can’t be done.
 Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/pressfoto
Sources:
ncbi.nlm.nih.gov/pubmed/15112850
deepdyve.com/lp/elsevier/lumbar-microdiscectomy-under-epidural-anesthesia-a-comparison-study-DBiuVBhDms
Best Medications for Sciatic Nerve Impingement
A spine doctor explains about medications for the pain of sciatic nerve pressure.
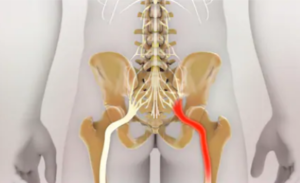
Sciatic nerve impingement can be caused by a herniated disc or a spasming piriformis muscle.
Either way, the pain has been described as “excruciating” by many patients.
It can come on suddenly, seemingly for no apparent reason, no known trigger.
Best medications for sciatic impingement pain?
“Medications in the classes of aspirin, non-steroidal anti-inflammatories, muscle relaxants, oral steroids, antidepressants and narcotics could be recommended to suppress the pain of symptomatic sciatic nerve,” says spinal and orthopedic surgeon Kenneth K. Hansraj, MD, who specializes in minimally invasive spine surgery, laminectomies and spinal fusions, and is author of the book, “Keys to an Amazing Life: Secrets of the Cervical Spine.”
He adds, “Each physician seems to have their own recipe for diminishing inflammation and calming the sciatic nerve.”
Why don’t prescription narcotics work (e.g., two Percocets)?
“Prescription narcotics may not work after a while when the patient develops a tolerance to the medication,” says Dr. Hansraj.
Oral steroid medications are often recommended as a pain reliever for people with sciatic pain, but at the same time, these can be taken only short-term.
“Long-term use of oral steroids may lead to increased blood sugar, osteoporosis, cataracts, muscular weakness and avascular necrosis (loss of blood supply leading to damage of the joints) of major joints including the hips and knees,” points out Dr. Hansraj.
But what if you absolutely cannot have surgery for your herniated disc?
For example, a person with a very bad heart may be a poor candidate for surgery simply because of the anesthesia.
“I have taken care of patients who have medical problems and comorbidities which will never allow them to have spinal surgery,” says Dr. Hansraj.
“Usually these patients are handled with continued conservative options.”
For sciatica these include heat and cold therapy, special chairs, physical therapy and of course, medications such as NSAIDs and antidepressants like Cymbalta.
 Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Nathan Devery
How Painful is Therapy for a Bulging Disc Supposed to Be?
How can a patient do physical therapy for a herniated disc if it hurts too much to exercise?
What if you have a herniated disc and find that the physical therapy exercises are impossible to do because you can’t get into the position without a lot of pain?
Some patients have this experience, yet surgery for the herniated disc is clearly out of the question — either because they are afraid of “going under the knife,” or because they have an unrelated medical condition that makes surgery risky.
Should you just grin and bear it? After all, a person who has never had an exercise regimen will find the pain of physical therapy more unbearable than will someone who is quite used to rigorous workout sessions or physical activity.
One thing that will invariably cross the patient’s mind is if the pain during physical therapy means that the movements are actually making the bulging disc worse.
Can physical therapy worsen a bulging disc?
“Physical therapy is employed to diminish pain and suffering,” says Kenneth K. Hansraj, MD, who specializes in minimally invasive spine surgery, laminectomies and spinal fusions, and is author of the book, “Keys to an Amazing Life: Secrets of the Cervical Spine.”
Dr. Hansraj continues, “Unfortunately, especially in the phases of pain, just touching the involved spinal area may lead to further pain and tenderness.
“I encourage my clients to stay with the therapy at this point, since the therapy will lead to diminished inflammation and restoration of function along with further tolerance of therapy.”
In other words, grin and bear it. Because if you do nothing for a disc herniation, it will likely never get better, and it certainly won’t magically go away.
Risk Factors for a Bulging or Herniated Disc
Several factors can increase the risk of developing a herniated disc.
Age is a primary risk factor, as the discs in the spine naturally degenerate and become more prone to herniation over time.
Physical activity also plays a role; individuals who engage in heavy lifting, repetitive bending, or strenuous activities are at higher risk, especially if they execute poor form.
Obesity adds extra pressure on the spine, increasing the likelihood of disc problems.
Poor posture and prolonged sitting can stress the spine and contribute to disc herniation.
Smoking is another risk factor, as it reduces blood flow to the spinal discs, impairing their health and resilience.
Additionally, genetics can contribute, as some people inherit a predisposition to disc issues.
Physical therapy is one of the best non-surgical treatments for the so-called bulging disc.
Do not give up on physical therapy, even if it causes some pain.
 Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus/CreativeCommons
Risk of Stroke after TIA “Soft” Symptoms vs. “Hard”

The risk of stroke seems to differ depending on type of transient ischemic attack symptoms a person experiences.
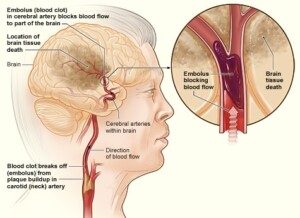
A transient ischemic attack (TIA) is a mini stroke, when a clot forms in a blood vessel in the brain, temporarily cutting off blood (and thus oxygen) to the portion of the brain that the vessel feeds.
Which portion of the brain suffers this event determines the nature of the symptoms; the nature of the TIA.
TIA symptoms vary as much as brain function does, according to Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
TIA symptoms are classified as either “soft” or “hard.”
Typical warning information regarding a transient ischemic attack states that one-third of people, who experience this event, will suffer a stroke within 12 months.
This is a general figure that does not take into account type of symptom.
For instance, what percentage of people, whose TIA(s) consisted of only dizziness and double vision, will go on to have a stroke within 12 months?
And what percentage of people, who have a transient ischemic attack consisting of slurred speech or one-sided weakness or paralysis, eventually will have a stroke within 12 months?
When type of TIA symptom is considered, these percentages will change.
The average is 30 percent when all the symptoms — any TIA — are taken into account.
Dr. Mikolaenko explains, “From my experience I see plenty of elderly patients with many TIAs in the past and no stroke, not even old strokes on MRI imaging.
“I always ask myself: Are these people, with multiple admissions for ‘soft’ stroke symptoms, will they ever have a stroke if they live long enough, or [is it that] secondary prevention medication which they are on keeps them away from developing a full-blown stroke?”
Secondary medication consists of blood thinners, which may include a daily aspirin.
Dr. Mikolaenko says the following are soft symptoms of a transient ischemic attack:
- Hemiparesthesias [one-sided numbness/tingling]
- Dizziness/vertigo/lightheadedness
- Blurry vision
- Short lasting diplopia (double vision)
- Confusion
- Neck pain (cervicalgia)
- Unilateral limb pain/heaviness/discomfort
- Very short lasting memory loss.
NOTE: The pain, heaviness and discomfort here do not refer to weakness, which is a hard symptom.
Dr. Mikolaenko says, “‘Hard’ symptoms of TIAs are: aphasia (expressive or comprehensive, or mixed), hemiparesis ( one-sided weakness) or hemiplegia, monocular painless blindness.” Aphasia refers to speaking difficulties.
If all you’ve experienced are the soft symptoms of TIA, this doesn’t mean brush them aside and assume you’ll never have a stroke.
You are still at increased risk of a stroke; transient ischemic attacks mean that something is seriously wrong with the blood circulation that leads to, or that’s in, your brain.
National Heart Lung and Blood Insitute
Soft TIA symptoms that occur while you’re driving, operating machinery, walking down stairs, etc., can result in a fatal accident.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
TIA Symptom: Body Pulling to One Side?
If your body suddenly feels like it wants to pull or veer to one side, could this mean a transient ischemic attack?
If you’ve recently experienced the sensation that your body was pulling to one side, do not blow off such a symptom.
“Sensation of body ‘wanting to go one side’ can be interpreted as veering to one side while walking, very likely might be a TIA,” says Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
Think of it this way: What else could explain such an oddball sensation?
You may be wondering, what is it about a transient ischemic attack that would cause you to feel as though your body was wanting to pull to one side?
The TIA could be cutting off blood flow to the part of the brain that controls that side of the body, making motor control and sensory perception impaired.
What you might actually be experiencing is a heaviness on one side, and if one side of your body feels or seems heavier than the other, it will seem like it’s being pulled in that direction.
“The manifestation of TIA can be protean [extremely variable], and the symptoms of TIA are as many as there are brain functions,” says Dr. Mikolaenko.
“But typically TIA symptoms will point to a specific brain region or its vascular territory.
“Veering to one side or another might be due to cerebellar dysfunction, and vertebro-basilar TIA should be thought of.”
If you’re suddenly overcome with the feeling that your body is being pulled to one side, or feels heavy or numb on one side — have someone immediately drive you to the ER, especially if you have risk factors for a TIA or stroke:
Over Age 50
Don’t Work Out; Sedentary Lifestyle
Obese
Diet High in Processed Foods
Smoker
Family History of Stroke
Diabetes
Poor Cholesterol Profile
Diagnosis of Atrial Fibrillation
TIA Is a Warning a Stroke May Be Coming
You have to wonder how many people who’ve suffered from a massive stroke — in the few months prior to it — had had a TIA but didn’t inform anyone about it.
Perhaps they didn’t even know they were having a TIA and attributed the odd sensation of being pulled to one side as anxiety related or maybe due to lack of sleep or having had too much to drink the day before.
Or maybe they wanted to mention the symptom, but at the time, nobody was around, and they simply forgot about it.
A TIA is a significant risk factor for a future stroke, and it serves as an alert that the individual’s vascular health needs immediate attention.
Awareness campaigns for stroke (symptoms are the same as a TIA) focus on only a handful of sudden signs: sudden weakness or paralysis on one side; clumsiness; facial drooping; speech difficulty; trouble with vision; mental confusion.
We often don’t hear about the more unusual symptoms such as the feeling that your body is being pulled to one side, feeling that one side of your body is suddenly heavy or difficulty swallowing.
Any sudden changes as described above warrant prompt medical attention.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik
Can a Recent Transient Ischemic Attack Be Detected on Exam?
Is there a special test that can tell if you just had a transient ischemic attack?
A TIA (transient ischemic attack) is a mini stroke — and even though the symptoms may vanish after only 30 seconds, a TIA is a medical emergency because it shows that the patient is at very high risk for a massive stroke.
And in case you don’t already know, stroke is the leading cause of disability in the U.S. And it doesn’t just strike senior citizens.
Smoking and high blood pressure are key risk factors for a mini stroke or TIA. So are obesity and lack of exercise.
Out of these four risk factors for a transient ischemic attack, only one involves body weight. So don’t think you’re in the clear just because you’re thin.
Certainly, there exists a test that can tell if someone had a TIA, right?
Well, unfortunately, no such test exists.
“All of the tests that a patient with suspected transient ischemic attack will have ordered have two main goals: substantiate the diagnosis of brain ischemia and establish the cause of brain ischemia,” says Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
What is ischemia?
Ischemia refers to interrupted oxygen supply due to impaired blood flow.
In the case of a mini stroke (or stroke), the cause would be a blood clot.
The clot may originate in the brain, or it may come from the carotid artery in the neck, which carries blood to the brain.
The clot can also originate in the heart. It travels up the aorta and into the carotid artery and to the brain where it lodges in a tiny vessel, obstructing oxygen to the area of the brain that the vessel feeds.
Clues to a Transient Ischemic Attack
“General chemistry labs might detect metabolic abnormalities leading to stroke imitation,” says Dr. Mikolaenko.
“Abnormal blood count and specific blood antibodies may provide useful clues to blood rheology [pertaining to the flow of blood matter] or increased blood-clot forming.”
In short, it may be many years before a single test can identify a TIA with 100 percent accuracy.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Roman Zaiets
sscpywrt26
Single Symptom TIA vs. Multi-Symptom
If you think a TIA that causes only one symptom isn’t as serious as a multi-symptom transient ischemic attack, you’re in for a shock.
Suppose you have sudden-onset blurry vision but no other symptoms, and you suppose this was a transient ischemic attack, but then you figure, “Oh, can’t be serious; it was only one symptom.”
“Single TIA symptom might be as serious as multi-symptoms,” says Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
“We, vascular neurologists, sometimes rate the clinical picture into ‘hard’ and ‘soft’ symptoms of TIA.
“The hard ones usually are problems with language (aphasia), one-sided weakness (hemiparesis) or loss of vision in one eye (monocular blindness).
“But many patients might have mild headache (cephalgia), dizziness (vertigo or lightheadedness), confusion, blurry vision, which very often will be ignored or pointed as not feeling well.”
These sensations may also be brushed off as side effects of medication.
Dr. Mikolaenko refers to the mild headache, dizziness, confusion and blurry vision as soft signs of a TIA, “and such transient symptoms require careful neurologic evaluation, particularly if they occur in the right context.
“It is believed that TIAs are warning signs of stroke, especially those associated with weakness and speech impairment.
“Patients who experience only isolated sensory symptoms [such as dizziness, slight headache, double vision] that resolve within 10 minutes are at risk of recurrent TIAs but rarely for the full-blown stroke.”
This doesn’t get you off the hook. If you have a “soft” TIA sign while driving, you’ll likely lose control of the car.
A soft symptom even while standing could result in a hard fall to the floor, causing a serious injury such as a brain bleed.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/LightField Studios
sscpywrt26
Can a Doctor Tell if You Had a TIA By Looking into the Eyes?

A transient ischemic attack (mini-stroke) is a scary thing, and a doctor will use a special instrument to peer into the patient’s eyes.
This will help the physician, giving information or clues to see if there are any possible signs of a recent TIA.
How well can a physician spot evidence of a TIA by checking the eyes?
The doctor uses an instrument called an ophthalmoscope.
“So-called funduscopic exam of the deep structures of the eye, particularly the retina and its vessels, might pinpoint towards signs of a TIA, especially if retinal vasculature abnormalities are detected,” explains Ivan Mikolaenko, MD, a board certified neurologist of 20+ years based in New York with subspecialty certification in neurocritical care.
However, if this exam turns up nothing, this does not rule out a TIA!
It’s impossible for a doctor to know that you did NOT have a transient ischemic attack if the view of the deep structures of the eyes turned up normal.
In other words, this exam is very meaningful if something does indeed turn up, but it means nothing if the result is negative. Many transient ischemic attacks will not appear on the funduscopic exam.
What to Do if You suspect a TIA and the Eye Exam Is Normal
Ask your doctor what the next step should be, even if he says everything looks fine.
By definition, a TIA is temporary. So just because you feel normal sitting there in the doctor’s office, and whatever odd symptoms you had are long gone, doesn’t mean that you did not have a blood clot in your brain.
Your doctor should have your complete medical history and use that, along with other tests, to determine your risk factors for a miniature stroke.
Certainly, the index for suspicion of a transient ischemic attack will be a lot higher in a 50-year-old smoker who has borderline hypertension, than in a 25-year-old nonsmoker with low-range blood pressure.
Conditions treated by Dr. Mikolaenko in the intensive care setting include strokes, ruptured aneurysms, trauma-related brain and spinal cord injuries, seizures and brain swelling, infections and tumors.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Miriam Doerr Martin Frommherz
sscpywrt26
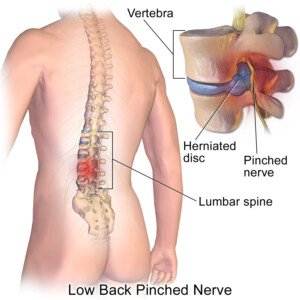
When Is Surgery Needed for a Lumbar Herniated Disc?
What is the point at which it’s time to seriously consider surgery to remedy a herniated disc in the low back?
“Learning to live with the pain” is the mantra heard by many people who have a herniated (bulging) disc.
This is also sometimes referred to as a pinched nerve by laypeople.
But it’s all the same deal, regardless of name: a compression of a nerve at the lumbar spinal column.
The resulting pain may be local or radiate out somewhat, sometimes extending down the leg.
Though the leg is affected in these cases, it’s not because of a muscle problem. It’s because of the nerve in the leg that originates in the spinal cord — where the site of compression is.
For a while patients will try to manage the low back (or leg) pain via conservative means, wondering for how long they can hold off on surgery before the pain becomes impossible to live with.
Source: myupchar. com
When Is Surgery Needed for a Herniated Disc?
“Surgery would be indicated for lumbar herniated disc when a patient is noticing a progressive loss of strength in the leg; we term that partial paralysis,” says Dr. P. Justin Tortolani, an orthopedic surgeon and spine specialist with University of Maryland St. Joseph Medical Center.
“Another indication is when there is pain that is not retractable; when nothing tried is helping,” continues Dr. Tortolani.
This would include a failure of “steroid injection, acupuncture and just the tincture of time.”
A herniated disc can cause shooting, stabbing but brief episodes of pain that can literally stop a person in their tracks.
There may be numbness and tingling. Sitting in the same position for long periods, with pressure on the hamstring (back of the upper leg) can bring on numbness and tingling.
This may often occur as a result of sitting on a toilet seat for an extended period.
 Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can a Bulging Disc Be Untreatable?

Find out from a doctor if a low back herniated (bulging) disc can be untreatable.
A bulging disc puts pressure on nerves that come out of the spinal cord.
A bulging disc occurs when the soft, gel-like center of a spinal disc pushes through its outer layer, potentially compressing nearby nerves.
This pressure on the nerves can cause symptoms such as pain, numbness or weakness in the affected area, often radiating to the arms or legs depending on the location of the disc.
Even a foot can be affected by pain, numbness and/or tingling.
Typically, conservative (nonsurgical) treatments are tried first.
These include physical therapy, hot packs, ice packs, massage and painkilling drugs.
But some people also undergo surgery when all else has failed for their bulging disc.
The very vast majority of herniated disc cases are treatable.
Treatments for a Bulging Disc
This is a condition in which the conservative approach (e.g., physical therapy, back supports for chairs, NSAIDs) wins hands-down over surgery.
Just because you have an issue with your spine, doesn’t mean you automatically need surgery.
Surgery in the case of a bulging disc should always be a last resort, when all else has failed.
When is a herniated disc untreatable?
“Very rarely would it be untreatable unless the patient had some medical factors in which surgery couldn’t be performed like severe heart disease,” says Dr. P. Justin Tortolani, an orthopedic surgeon and spine specialist with University of Maryland St. Joseph Medical Center.
“I’ve never had a patient come in with a herniated disc that couldn’t be treated, but I had one with nerve compression in the lower back, where their heart was so sick their doctors wouldn’t let them go through general anesthesia.”
When a patient feels that they have tried every conservative option yet the pain is still disruptive to their life, they have to ask themselves if they truly, faithfully have given physical therapy a fair chance.
It’s not unheard of for patients to prematurely give up on physical therapy due to either some degree of pain during the movements or assuming ahead of time that PT just won’t work — and hence, not trying it or skipping sessions. They then create a self-fulfilling prophecy.
The person with a herniated or bulging disc needs to give all nonsurgical treatments a fair shake before deciding that the case is hopeless without surgery.
 Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.