What’s the Death Rate of Abdominal Aortic Aneurysm Repair?
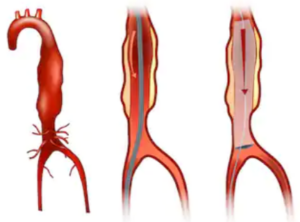
The death rate following the repair of an abdominal aortic aneurysm is something that you’d definitely want to know.
However, if your doctor is already discussing surgical treatment with you, it’s a safe bet that it would be very dangerous to decline surgery.
After all, the aneurysm in your abdominal aorta is at high risk of rupturing, and the internal bleeding from that can be fatal in minutes.
All invasive surgeries do carry risks, and surgeons always weigh the benefits of the surgery against the risks of going without it.
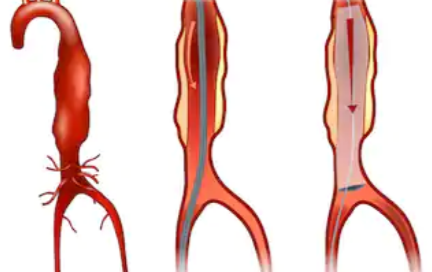
The case of an abdominal aortic aneurysm is no exception to this standard of medical practice. Below is a graphic image of an actual abdominal aortic aneurysm. This particular AAA had not been repaired, as is evident.

Hertzer NR, CC
“Most randomized control trials indicate the 30-day perioperative mortality for elective repair of abdominal aortic aneurysm is about 5%,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“This is major surgery and presence of a AAA is a marker for other significant cardiovascular disease. As a matter of fact, beyond the 30-day, most people die from other cardiovascular causes, such as MI, CVA, etc.”
MI = myocardial infarction (heart attack).
CVA = cerebral vascular accident (stroke).
It is advised that men over the age of 70 be screened for the presence of an abdominal aortic aneurysm.
In addition to male gender and older age, high blood pressure and smoking are risk factors.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Sakurra
How Long Does It Take DVT to Get to Lungs After Breaking?

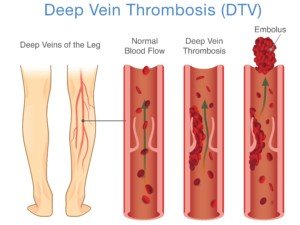
A DVT (blood clot) that’s in your leg has a chance of breaking apart or completely dislodging and then going to your lungs…and how long this takes is not what you may think it is.
I was reading in a health anxiety forum a lengthy thread that was started by a person who’d been at her computer for “three days” googling things relating to health — but not DVT.
She took breaks only to use the bathroom, catnap here and there, maybe eat a little something, but essentially it was a marathon at the computer for three days.
Upon getting up at the end of the computer stint, she felt a pain in her calf and googled this, learning that marathon sitting at a computer can cause a blood clot.
She then freaked out, convinced that there was a DVT in her calf. She kept making posts in the thread over a 45 minute period, corresponding in the then-real-time with a few other caring health anxiety sufferers.
At some point she then said the pain had moved up to her knee and was panicking that the DVT had broken off and was on the way to her lungs.
This post was maybe 10 minutes after the first one.
Then 15 minutes later she made a post that her thigh was hurting, and could the DVT then be in her thigh on the way to her lungs?
Shutterstock/solar22
What a Vascular Surgeon Says
According to the times these posts were made, 15 or so minutes had lapsed between the onset of the knee pain and the thigh pain.
She was convinced that this meant that the DVT was enroute to her lungs.
When a blood clot gets into a lung, it’s called a pulmonary embolism.
Blood Clot in a Leg: Hare or Turtoise?
So if a DVT breaks off or dislodges from its location in the leg, just how long will it take to get to the lungs and become a pulmonary embolism?
“Generally, it is immediate (do not know the exact time period), but by far the majority remain clinically silent since they can be very small,” explains Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
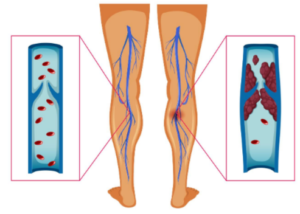
Imagine that you have a DVT anywhere in your leg, and suddenly, a part of it breaks off or dislodges.
This clot material then gets swept up by the venous flow that returns de-oxygenated blood to the lungs.
This is akin to tossing stuff in a river, and the flow of the river carries it downstream.
Of course, veins in the legs pump blood “upstream,” but the principle is the same:
The bits of DVT immediately get carried away with this blood circulation and, like Dr. Gashti says, the time lapse is immediate from when the clot dislodges to when it arrives in the lung (pulmonary artery).
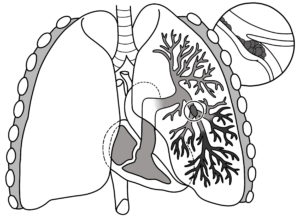
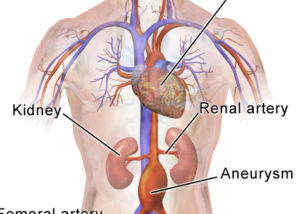
Pulmonary embolism
Think of it this way:
The time it takes for a broken DVT to get to your lungs is the time it takes for the blood in your calf vein, at any given time, to get to your lungs. That’s just seconds.
Though most pulmonary emboli don’t produce symptoms due to being very small, this doesn’t negate the estimated 300,000 U.S. deaths every year to a pulmonary embolism.
A pulmonary embolism is a common event in the U.S. population.
DVT Risks
Recent surgery
Excessive bedrest
Smoking
Obesity
Pregnancy
Extended air travel
Extended vehicular travel
Lack of exercise
Senior age
If you suspect a DVT, and knowing that if it dislodges, the occurrence of a pulmonary embolism will be literally within seconds, don’t delay getting yourself checked out in the nearest emergency room.
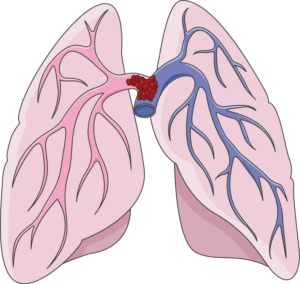
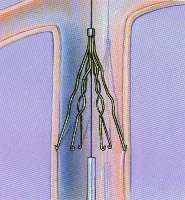
A “saddle” type pulmonary embolism, plugging up the area where the pulmonary artery splits off into each lung. This can cause death in minutes. Laboratoires Servier, CC BY-SA/creativecommons.org/Wikimedia Commons
The time between when a blood clot breaks to when it reaches the lungs is a few SECONDS.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ShotPrime Studio
Can You Get a Pulmonary Embolism without a DVT?

Find out the interesting answer to the question: Can a pulmonary embolism form in the absence of a DVT?
“By definition a PE is an ‘embolus’ that has traveled to the lungs,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
An embolus is a thrombus (blood clot) that is dislodged from one place and ends up in another.
“It can be both venous and arterial. Of course a pulmonary embolus must have a venous source.”
In other words, in order for a blood clot to end up in a pulmonary artery, it has to travel there somehow, and the only way is via veins (venous pertains to veins).
“I assume that one can form a thrombus de novo [originating from] in a pulmonary artery, but that would not be considered a PE.”
Remember, embolus refers to a blood clot that has dislodged. So if the clot originates in the lungs, it’s not a “pulmonary embolus.”
“Not infrequently a patient has a pulmonary embolus, but a source cannot be found,” continues Dr. Gashti.
“In these cases the possibilities include: thrombus completely broke off from the original vein and therefore none can be found now; thrombus was in a vein in the upper extremity which normally is not studied in a patient with a PE unless clinically indicated, or that it came directly from the right heart (after open heart surgery), after having a heart attack, or from a tumor, i.e., myxoma.”
A myxoma is a rare, usually noncancerous tumor made of soft, jelly-like tissue, and it often arises in the heart, which can sometimes cause blockages or heart problems.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
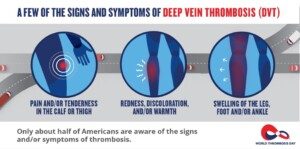
Can a DVT Cause Swelling in the Ankle Only & Nowhere Else?

How likely is it that the swelling in only one ankle, but nowhere else in the leg, is being caused by a deep vein thrombosis?
A DVT typically causes swelling up and down the lower leg and may include the ankle.
But is it possible for this kind of blood clot to swell up ONLY the ankle?
Can a deep vein thrombosis cause swelling only in a person’s ankle?
“That would be unusual, unless the very distal tibial veins are thrombosed, in which case it would not be of great significance, again because these emboli would be very tiny,” explains Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
The distal tibial veins are the veins in the front or anterior of the lower leg where the tibia bone is.
The tibia is the larger of the two lower leg bones. Distal means distant from the center of the body, so in this case, the location would be near the ankle.
Thus, if a DVT forms near the front of the lower leg near the ankle, the clots would be, as Dr. Gashti says, “very tiny,” and thus not potent enough to cause swelling going up the leg, but rather, more likely confining it to only the ankle.

Scientific Animations, Creative Commons/BY-SA
Warning Signs of a DVT Other than Swelling
• One area of the leg is much warmer than the other.
• Area of suspicion is unusually tender to the touch.
• There is pain, even at rest, in the calf or behind the knee. The pain may feel like a strong soreness or a cramp.
• The area is noticeably reddish.
• You very recently had joint replacement or abdominal surgery.
• You’ve recently had excessive bed rest.
• You’ve recently been on a long airplane flight.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from the University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ARZTSAMUI
DVT in Neck after CABG: Shouldn’t Patient Get SVC Filter?
What should be done when a patient gets a DVT in the neck after coronary bypass surgery?
Seems like an SVC filter should be placed?
Following coronary bypass surgery (a.k.a. CABG), it’s possible for a patient to develop a DVT in the neck.
This happened to my mother following her CABG.
“She has a big DVT,” I was told by the nurse after results of the ultrasound came in.
It’s scary to hear that your mother has a “big DVT” in her neck.
DVT stands for deep vein thrombosis. Fragments of, or the entire clot, can break away from where it’s lodged and travel to the lungs. This holds especially true if the clot is in the jugular vein.
In the lungs it could interfere with breathing. Depending on its location, it could cause death very quickly. So of course, knowing all this, I was very worried.
But nothing was done in the case of my mother. They just let it be; no intervention to prevent the clot from traveling to her lungs.
This was extremely worrisome, as her left arm kept getting bigger and bigger from the swelling induced by the DVT.
At the time, I didn’t know about an SVC filter, which is designed to prevent a dislodged portion of a DVT from entering the lungs and becoming a potentially fatal pulmonary embolism.
SVC stands for superior vena cava — a major vein located above the heart.
This vein transports de-oxygenated blood from the upper body to the heart so that it gets re-oxygenated.
After learning about the SVC filter long after my mother had been released from the hospital, I’ve always wondered what the doctors’ responses would have been had I insisted on an SVC filter placement for her.
“Most of these DVTs would be labeled as provoked, most often secondary to central venous catheters,” says Seyed-Mojtaba (Moji) Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“Generally these are focal and limited to the site of the catheter (most often in the internal jugular vein). These can be watched.
“But if the thrombus extends to the subclavian/innominate veins, then most physicians would consider anticoagulation if there are no contraindications.”
Following CABG, a patient can bleed to death from anticoagulant drugs.
“If anticoagulation is contraindicated, then an SVC filter would be indicated,” says Dr. Gashti.
“The SVC is much shorter than the IVC [inferior vena cava], and therefore placement of a filter in the SVC is technically more challenging. You have to make sure the length is adequate.
“Currently there are no filters in the market indicated for SVC, and if you place one, it would be off label.”
This means, for instance, that a filter that’s designed for the inferior vena cava (IVC, below the heart) could be placed in the superior vena cava.
Thus, the procedure is possible, but the mere presence of a DVT in the neck of a CABG patient won’t automatically mean that an IVC filter will be placed in the superior vena cava. The patient’s condition and other factors will need to be weighed.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/DC Studio
Risk of DVT in People Who Use Wheelchairs

Is deep vein thrombosis common in people who use wheelchairs?
Since prolonged “inactivity” is a risk factor for developing a DVT, the logical conclusion would be that this condition is quite common in people whose legs are completely paralyzed and thus are confined to a wheelchair.
Complete paralysis, for the sake of this article, means that the person cannot move, at all, their lower limbs (such as from a severed spinal cord), versus someone who has a neurological disease (such as multiple sclerosis) and can yield minute movements throughout the day while in a wheelchair.
“Immobility is only one of the three factors leading to DVT; the other two being intimal injury to a vein] and a hypercoagulable state,” says Seyed-Mojtaba (Moji) Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“In addition I am not sure if we can make the statement that DVT is not common in wheelchair bound people; symptomatic DVT may be.
“Again, majority of these can remain asymptomatic and/or missed. I am not aware of any studies that have looked at this population.”
I did a little searching on this and came up with one study that looked at DVT prevalence in people with late-stage multiple sclerosis who were confined to a wheelchair.
The report is in the April 2010 Thrombosis Research.
The investigation involved 132 patients. Deep vein thrombosis was present in 58 (43.9 percent).
Furthermore, 32 percent had a history of VTE: venous thromboembolism, the term that pertains to the phenomenon of a deep vein thrombosis dislodging and embolizing in the lungs.
The conclusions include that the rate of DVT in late stage multiple sclerosis may exceed 40 percent, and that doctors should “consider the systematic application of long term preventive measures” for this demographic.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Long After Air Travel Does DVT (Blood Clot) Risk Last?

So you’ve been cramped on that airplane for hours and are finally walking on the ground; how long after will DVT blood clot risk last?
“As far as I know, DVT forms while traveling,” says Seyed-Mojtaba Gashti, MD, a board certified vascular surgeon with Broward Health Medical Center in Florida.
“So once you are no longer in the air and resuming normal activity/oral intake, your risk should be at baseline.”
Do not confuse this with the phenomenon of symptoms of a deep vein thrombosis occurring days after the plane has landed!
Some patients do not make this association, since they believe that a blood clot from air travel would necessarily show symptoms right away.
But this is not necessarily so. Symptoms of a deep vein thrombosis can be delayed enough to seem not connected to the air travel.
DVT Risk Factors
People who have risk factors for a DVT in addition to just having traveled by air for many hours should be on the lookout for suspicious symptoms.
First off, did you stay in your seat nearly the entire time while on the plane? Not good.
How much did you move your legs in that tight cramped space? Did you do lots of ankle, knee and hip movements or pretty much keep everything immobile? Inertia can cause blood to pool in the lower legs.
Did you drink several glasses of water or consume nothing or only alcohol?
Symptoms of Deep Vein Thrombosis
-Swelling in only one leg
-Pain in calve or behind knee; may feel like a cramp
-Redness in calve or at the knee
-Warmth in calve or knee area
-Pain or tenderness upon touching the calve or while walking
Symptoms of Blood Clot Having Traveled to the Lungs: Pulmonary Embolism
Fainting soon after the air flight is suspicious for a blood clot in the lung.
So is sudden chest pain soon after flying.
However, these symptoms may occur days after traveling.

Dr. Gashti specializes in the diagnosis and treatment of vascular disease including abdominal and aortic aneurysm. He received his medical degree from University of New England College of Osteopathic Medicine and has been in practice for more than 20 years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/zusenjka
Diarrhea, Stomach Pain: Crohn’s Disease: PillCam Can Diagnose

Suffer from stomach pain and diarrhea?
This could be Crohn’s disease, which can be diagnosed by swallowing a pill that has a camera.
Crohn’s disease often presents with two key symptoms: diarrhea and stomach or abdominal pain.
The diagnosis can be missed by more common tests, resulting in a misdiagnosis.

For example, 24-year-old Sarah had been suffering from diarrhea and abdominal pain, and underwent many tests, getting no answers.
Finally she was given the PillCam SB, and was diagnosed correctly with Crohn’s disease.
“PillCam is a marvelous innovation and very effective imaging tool to look at the small intestine, which cannot be examined in its entirety with upper endoscopy or colonoscopy,” says Nadeem Baig, MD, a board certified gastroenterologist and hepatologist at Monmouth Gastroenterology, a division of Allied Digestive Health.
“PillCam is used to look for bleeding or tumors in the small intestine. It can also pick up ulcers and inflammatory disorders of the small intestine, like Crohn’s disease for example.”
What is Crohn’s?
It’s a type of Inflammatory bowel disease that can affect any point along the GI tract, and other than abdominal or stomach pain and diarrhea, can also cause blood in the stools, ulcers, appetite suppression, weight loss, fatigue, arthritis, fever, skin disorders, mouth sores and an inflamed liver.
These symptoms, particularly if limited to diarrhea and stomach pain, can also mean many other conditions.
Thus, if you suffer from abdominal pain or cramping, and diarrhea, it’s crucial to get an accurate diagnosis.
There’s no cure for Crohn’s, and in three-quarters of patients, lesions exist in the small bowel.
Historically, it’s been difficult for doctors to visualize via instruments the small bowel.
Yet this area is crucial for ongoing monitoring for Crohn’s patients, even when symptoms are in remission.
In fact, this disorder can progress in the bowel without a symptom presentation.
To assess activity of the Crohn’s condition, doctors typically use a CAT scan, which emits radiation.
Camera in a Pill: PillCam SB
PillCam SB is capsule endoscopy, a non-invasive, non-radiation method of viewing the lining of the lower bowel, yielding a better view than what a CT scan can deliver.
How big is the FDA-approved PillCam SB?
It’s 11 mm x 26 mm and contains an imaging device plus light source. It rapidly transmits images, totaling over 50,000 pictures per procedure duration.
Patients as young as two years can use this device, considered the gold standard for evaluating the small bowel.
For those with Crohn’s disease or any disorder who are concerned about any risks from PillCam SB, those risks include retention or aspiration of the capsule, or skin irritation.
The endoscopic placement of the capsule may also pose some risks.
“The one time PillCam should not be used is If one suspects they have a blockage in the small intestine,” says Dr. Baig. “In such a scenario, it can get stuck and require surgery to remove.”
If you have unexplained stomach pain and/or diarrhea, make an appointment with a gastroenterologist.
 Dr. Baig’s specialties include gastrointestinal cancers and liver disease, plus gallbladder, biliary tract and pancreatic disorders. He is an assistant clinical professor of medicine at the University of Medicine and Dentistry of NJ/Robert Wood Johnson Medical School.
Dr. Baig’s specialties include gastrointestinal cancers and liver disease, plus gallbladder, biliary tract and pancreatic disorders. He is an assistant clinical professor of medicine at the University of Medicine and Dentistry of NJ/Robert Wood Johnson Medical School.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com/ jcomp
Source: givenimaging.com
NOISE INDUCED HEARING LOSS Causes, Prevention, Who’s at Risk

Noise pollution is a very real problem, says the EPA, yet few people take the risks of hearing loss seriously.
We are still in the Dark Ages when it comes to understanding the risks of noise pollution for hearing loss and also its effects on general health.
Humans did not evolve in a loud, noisy environment.
The nerve cells in our ears are fragile and cannot be regenerated once they’re destroyed by the onslaught of loud sounds.
NIHL: Noise Induced Hearing Loss. What Makes You Think You’re Immune?
“The most common causes of NIHL are sudden, loud bursts of sound (like a gunshot or a car accident) and prolonged exposure to loud noise (like loud music or power tools as well as music),” says Rivka Strom, AuD, CCC-A, chief audiologist at Central Hearing LLC in NY.
“NIHL can be caused by a one time exposure to an intense impulse sound or from continuous exposure to loud sounds,” continues Strom.
“Recreational activities and occupational activities can include target shooting, lawn mowing, and listening to very loud music, especially through earbuds.
“In general, listening to any noise at an unsafe level for an extended period of time is damaging.
“The higher the level of noise and the longer individuals are exposed to it, the greater the risk of suffering harm from it.”
*****
Things to Think About
People will wear sunscreen at outdoor sporting events like football and baseball games, and auto racing, but won’t wear hearing protection.
They don’t want sun-induced skin cancer or wrinkles, but what about noise induced hearing loss from the roaring of fans or the sounds of engines?
All people should wear earplugs or noise cancelling headphones at sporting events for as much time as possible.
If you anticipate doing a lot of talking, then earplugs are the better option, as these can easily be loosened and tightened.
Custom made earplugs are virtually invisible. Unfortunately, not a whole lot of people encourage their teenagers to wear earplugs at live concerts. The adults themselves hardly ever do that.
If teens want to preserver their naturally good hearing, they need to use earplugs at concerts.
ALL loud volume can damage hearing, regardless of the nature of the sound — be it drums at a loud concert, aircraft flying low, a chainsaw, a motorcycle or even children screaming during play.

Dr. Strom is a member of the American Speech Language and Hearing Association and has received several awards including Brooklyn College’s Excellence In Audiology Award.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Yeexin Richelle
Can Being Around Screaming Kids Ruin Your Hearing?

An audiologist addresses a fair question: Can hearing be damaged by screaming children?
I was inspired to interview an audiologist for this article because my sister has been diagnosed with bilateral moderate hearing loss.
She has three kids and two are particularly loud, the whoop-and-holler type. A game of Scrabble will get these teen girls quite loudly excited.
They also have a habit of yelling out to their mother when they want her attention.
By the time they were 17 and 15, my sister had been diagnosed with the hearing loss. That’s a lot of years to be exposed to loud kids.
Being that these girls were so loud as teenagers, I can imagine that when younger, they did a lot of screaming when playing or when excited.
After I told the expert source for this article that my sister has always worked in quiet environments, didn’t wear earbuds, blast her music, hang around loud machinery, shoot guns or participate in other loud activities, here is what my expert source stated:
“I suppose it is fair to conclude that repeated exposure to screaming children over a period of many years could have caused her moderate nerve type hearing loss,” says Rachel Raphael, M.A., CCC-A, an audiologist with ENT Baltimore.
“For those who worked in daycare or around loud children, we usually don’t consider that a risk factor for noise induced hearing loss, but I’m sure there are exceptions.
“Once again, not only the loudness/intensity of the sound, but individual susceptibility and length of exposure must be considered.”