Can Anorexic Mom’s Body Prevent Daughter from Eating Disorder?

A girl is more likely to develop anorexia nervosa, relative to her baseline inclination, if her mother has this eating disorder.
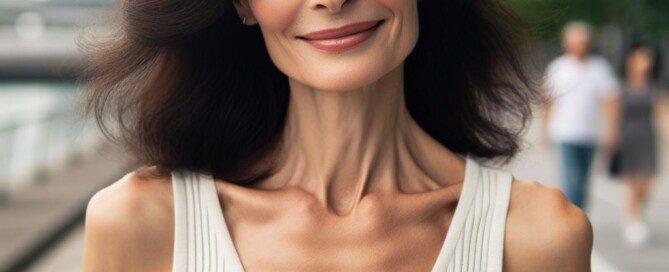
From an intuitive point of view, it seems as though just the sight of an emaciated physique would be enough to deter the daughter from developing the anorexia that she sees her mother battling with daily.
Mayoclinic.com cites that having a first-degree relative with anorexia (which includes the mother) puts a child at a “much higher risk” of developing this condition.
How much is due to genetics and how much is due to learned behavior or dysfunctional family dynamics?
I’ve seen many women over the years who appeared to have anorexia. I’m not talking about “thin” women (or teens). My 15-year-old niece has what’s considered a “skinny” body.
But if she’s walking down the street in tight jeans and a tee shirt, it’s very unlikely that anyone is going to assume that she has an eating disorder.
She eats normal amounts of food and shows no signs of purging. She’s simply in a vertical growth spurt.
However, I’ve seen what truly appears to be significant undernourishment, including a woman at my gym who (according to my personal trainer’s eye) appears to weigh 75 pounds on a 5-4 frame.
So here’s something odd to consider: A daughter of an anorexic woman is at increased risk of developing this eating disorder, even though her mother’s body would surely be quite alarming in appearance.
“In my experience, the mother’s emaciated body is actually a deterring factor for the daughters developing anorexia,” says
Mehri Moore, MD, medical director/founder of THIRA Health in Washington which offers programs for women and girls facing depression and anxiety.
But what about Mayoclinic.com’s statement that anorexia risk is greater in children when a mother has this eating disorder?
Those daughters who never develop anorexia, perhaps, as Dr. Moore explains further, “can more easily recognize that their mother’s anorexia is an illness.”
Another thing to consider when wondering if an anorexic woman’s body can prevent her daughter from developing the illness, is the degree of malnourishment.
Anorexia is on a continuum, just like overeating is. Some functioning anorexics aren’t emaciated, but may look more like my niece.
Dr. Moore explains, “It is much more confusing for daughters when anorexic mothers are thin but not emaciated.”
And when a girl’s anorexic mother seems more fashionably thin than skeletal, she may very well be the recipient of compliments about her thin frame, says Dr. Moore.
If her daughter hears this enough, the daughter may “strive for this thin look,” adds Dr. Moore.
Will the youthfully lean daughters of the 75 pound woman ever aspire to have a body like hers?
I’d think that her three young daughters would rather want a body like Miley Cyrus, Taylor Swift or a Victoria’s Secret model. However, in an effort to achieve that, they may go overboard and actually become anorexic.
A woman with anorexia should not assume that her daughters are at low risk for developing the illness just because she’s skin and bones, or even if her daughters have remarked how frightfully thin she is. The heightened risk can still be there.

In 1991, Dr. Moore founded The Moore Center (now Eating Recovery Center of Washington), which is the longest-established treatment center specializing in eating disorder treatment in the Pacific Northwest.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Source: mayoclinic.com/health/anorexia/DS00606/DSECTION=risk-factors
How Kids Can Motivate Anorexic Mom to Seek Treatment
Here are guidelines for kids to help their mother with anorexia nervosa seek treatment.
If you’re a teenager or even younger, and your mother has anorexia nervosa, it’s presumable that you’d like to help out, but are not sure how to go about doing this beyond, “Mom, I think you need treatment for your eating disorder.”
So what, then, can kids do to help their mother with anorexia realize that she should seek out treatment?
“The most important piece is to not blame yourself and to be honest,” says Tammy Holcomb, MS, EdS, a licensed professional counselor who specializes in eating disorders.
“Let your mom know that you love her and are concerned that she is not taking care of herself.”
What does not work so well is if you’re vague, as in, “Mom, I wish you’d get help for your eating disorder.”
This vagueness is almost akin to your mother telling you, “Clean up the garage,” and leaving it at that.
You then step into the garage: It’s a complete mess. You don’t know where to begin. It’s overwhelming.
However, if your mother had been more specific, as in, “Go into the garage with a big garbage bag and put all the scraps of paper, rags and old magazines you see on the floor into it,” the task would be far less daunting.
This principle applies to helping your mother out who has anorexia nervosa.
Holcomb says to give pinpointed examples whenever you can: “For example, telling your mom that you wish she could sit down and have a meal with you.”
People with anorexia nervosa or other eating disorders often don’t believe they are “sick” or need help, and do not perceive themselves as others around them view them, says Holcomb.
She urges specificity, citing another example: “You looked really pretty when you wore a size 8, but now you are too small at a size 4. I think you have lost too much weight.”
- Don’t be afraid to be upfront and lovingly honest.
- Don’t be critical or admonish.
Imagine you’re struggling with math. You’d be more receptive to your mother if she tenderly offered to help, rather than if she criticized you for being “lazy.”
Holcomb explains further, “Also, don’t hold secrets for a sick mom. Talk to another adult you trust. Either your dad or someone at school.
“Sometimes adults don’t see things until you point it out to them!”
If your mother has anorexia nervosa, do not give up when it comes to getting her to seek treatment.
 Tammy Holcomb founded the Atlanta Eating Disorder Coalition in 2003 and runs a weekly women’s sexual trauma therapy group. She is the former executive director of Carolina House eating disorder programs in NC.
Tammy Holcomb founded the Atlanta Eating Disorder Coalition in 2003 and runs a weekly women’s sexual trauma therapy group. She is the former executive director of Carolina House eating disorder programs in NC.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Is It Wrong for Anorexic Women to Have Children?

Some people believe that a woman with anorexia should not have children — “have” as in raise kids.
In other words, that it’s not ethically right for anorexic women to decide to rear kids, as they’d be subjecting them to the emotional turmoil and extreme anxiety that this eating disorder creates.
“This is a very personal decision and I can only offer some points to consider (as to whether an anorexic woman should or should not start a family),” says Linda Centeno, PhD, clinical psychologist, and assistant director of the Koch Center in NJ that specializes in eating disorder treatment.
First of all, Dr. Centeno says that a child has a greater risk of developing anorexia or another eating disorder if the mother has anorexia.
This increased risk is, in part, genetic, adds Dr. Centeno. However, environment is also a powerful variable.
Dr. Centeno explains, “An anorexic mother is also at risk of modeling disordered eating and body image.
“If a mother is constantly dieting and expressing dislike towards her body, the child receives the message that restrictive eating is normal and a healthy body weight is not.”
What if an anorexic woman truly wants to have children; what should she do?
“One reason why it is important to seek eating disorder treatment before having a child is because many mothers may impart unhealthy eating patterns onto their children,” says Dr. Centeno.
An anorexic who wants to have kids should consider how destructive these patterns can actually be, such as restricting their child’s food intake — when the child very much needs adequate calories for optimal growth.
Or, she may make her kids eat more than necessary. The anorexic mother may express disapproval of her children’s size, even if they aren’t overweight.
She may avoid eating in the presence of family members, even skipping out on important get-togethers to avoid food.
“A mother with anorexia might underfeed her child to make her thin, or, you overfeed her to show nurturing,” says Dr. Centeno.
“Power struggles over food and eating often affect families when a mother has an eating disorder. Mothers need to set a good example for children with respect to weight and eating.”
If a woman with anorexia is wondering if she should or should not have children, she also has to consider another striking element: Kids need and crave their mother’s full attention.
“Individuals with anorexia spend much of their time internally focused on weight, food and body issues,” says Dr. Centeno.
“Even if a mother tries to hide her preoccupation with weight and food, her child will sense that she is not available in the way that the child needs.”
Children can be very perceptive and should not be underestimated, especially as they grow older.
“A child also needs to learn healthy ways of coping,” adds Dr. Centeno.”
Often, the anorexic individual relies chiefly on her eating disorder as a way to cope with life’s major as well as minor challenges, says Dr. Centeno.
Kids need to be shown non-food-related coping tactics for troublesome thoughts and feelings.
In summary, maybe the question shouldn’t be, “Is it wrong for anorexic women to have children,” but rather, “What should anorexic women who want children do to prepare for this new role in their life?”
 Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Five Ways Anorexia in Mother Negatively Affects Children

Though anorexia nervosa is an eating disorder rather than a drug or alcohol addiction, its consequences can have a profoundly negative effect on children of the patient.
Don’t assume “It’s just an eating disorder; how harmful can that be; it’s not like I’m an alcoholic.”
“In my career, I have assessed many individuals who have reported that his/her mother was anorexic or otherwise eating disordered during that individual’s childhood,” says Linda Centeno, PhD, clinical psychologist, and assistant director of the Koch Center in NJ that specializes in eating disorder treatment.
It’s a mistake to assume that this phenomenon can be explained only by a genetic inheritance.
#1. Environment plays a leading role in anorexia being “picked up” by children of the patient.
Dr. Centeno continues, “Many individuals have emphasized this historical fact as having contributed significantly to his/her own eating disorder etiology.”
Though the mother with anorexia may believe there’s no way her children would ever emulate her behavior because they have seen firsthand how she has suffered with the eating disorder, she has to realize that witnessing the negative effects isn’t always an effective deterrent.
This is why children of alcoholics often become alcoholics themselves, even though they grew up witnessing the harmful effects in their parent.
Kids’ minds are very impressionable and they may not have a good grasp on just how harmful eating disorders, especially anorexia, truly are, and may even perceive the situation as simply a benign method to achieving thinness.
#2. “Many individuals report that having been raised with such a mother led them to not know how to ‘eat normally,’” explains Dr. Centeno.

Shutterstock/fizkes
These children learned that food, or the restriction thereof, was the primary means for coping with painful emotions, continues Dr. Centeno.
Kids learn that food is a lot more than just fuel or sustenance; it’s therapy, it’s a reward, it’s punishment.
#3. Dr. Centeno offers this powerful statement: “Some (grown) children have expressed to me feeling ‘detached’ from his/her mother during childhood, ‘knowing’ that the mother’s eating disorder (or anorexia) was paramount in the mother’s life.”
In other words, in these particular cases the children have been made to feel less important than their mother’s obsession with food.
#4. Dr. Centeno says that another potential negative impact that anorexia has on kids is that some kids learn to overeat to make their mother happy.
The anorexic mother can’t have cake or even a bowl of cereal, so she may unconsciously derive satisfaction watching her kids overeat these foods — any foods, for that matter.
Thus, anorexia in the mother may lead to lifelong overeating in the (grown) child.
#5. “Other children report not having any ‘child-friendly’ food in the home growing up, and by having to eat those same foods that the mother ate, later developed anorexia or restrictive eating.”
 Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/VGstockstudio
Advice to Teen Girls with Anorexic Mothers

If you’re a teenaged girl who’s struggling because your mother has anorexia nervosa, know that you are absolutely not to blame for your mother’s eating disorder, says Linda Centeno, PhD, clinical psychologist, and assistant director of the Koch Center in NJ that specializes in eating disorder treatment.
“Despite what happens, most children who have a mother with an eating disorder worry about the parent’s health,” says Dr. Centeno.
If you’re a teen, ask yourself how often you’ve tried to intercept your mother from engaging in eating disorder behavior.
This is normal on the teenager’s part, just as it’s not surprising when a teenager tries to prevent their obese mother from engaging in compulsive overeating of junk food. Caring teens want what’s best for their mothers.
“However, just as teens didn’t cause the eating disorder, they alone cannot stop it,” says Dr. Centeno.
“A teen’s mother has to seek professional treatment,” or, the mother’s partner (assuming they don’t have an eating disorder) should step up and help with this rather than give up or be in denial.
So what can teen girls do, then, if their mother has anorexia?
Certainly they should not stand by idly and cross their fingers. Of course teens want to protect their mother from the anorexia.
If your mother is in denial of her eating disorder, the first step, says Dr. Centeno, is to admit that your mother indeed has an illness.
After all, some teens may attempt to cope with what they subconsciously or deep down inside know to be true, by convincing themselves that there’s actually NO problem.
Dr. Centeno urges teens to confide in a trusted adult who does not have an eating disorder, and this can be your father, any relative, a teacher, coach or school counselor.
What if there’s nobody you feel you can go to? Teens can call the National Eating Disorder Association.
“Ideally, a child or teen with an anorexic mother should work with a psychologist or experienced clinician to address his or her own distress,” says Dr. Centeno.
 Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
Dr. Centeno works with adolescents and adults. In her private practice her specific clinical expertise also includes anxiety and panic disorder, depression, relationship issues and sexual abuse.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Recovering Anorexic Says Eating Disorder Had Bad Impact on Kids

If you have anorexia nervosa, don’t underestimate how damaging the effects of this will be on your children, especially daughters. One woman shares how badly her anorexia nervosa affected her daughter.
I interviewed Kari Adams, who was 42 at the time I spoke with her.
She had received treatment for her anorexia nervosa at The Renfrew Center, which is the U.S.’s biggest network of eating disorder treatment facilities.
At around age 15 was when Adams began developing her eating disorder, and at 41 she sought treatment — but not before she had given birth to a daughter and son.
At the time I interviewed her, Adams was recovered and her daughter was 12.
My first question was how much she felt that her daughter was at risk for developing anorexia or some sort of body image distortion or unhealthy relationship with food.
“My daughter now struggles with body image issues,” says Adams. “She asks me almost daily if she is ‘fat’ and says she needs to go on a diet.
Of course, Adams is working hard with her daughter to build up the girl’s self-esteem.
As for her son, age 10 at the interview time, he gets upset upon hearing Adams negatively talk of her body.
And by the way, boys are not immune to developing anorexia nervosa.
Adams’ daughter was eight when she began noticing that her mother’s relationship with food was not normal.
“My daughter picked up on it when I was in the midst of my eating disorder,” says Adams.
The girl would say, “Mom, you have a problem.”
Adams continues, “After I went to treatment we talked about it; she admitted she didn’t know what an eating disorder was but knew something was wrong.”
“My struggle with food and self-abuse gnawed at me constantly because I had children,” says Adams, “and especially because I knew I was shaping my impressionable daughter who would perhaps one day be faced with similar issues.
The Guilt Factor
Adams explains that as her son was rapidly putting on weight, she was feeling tremendous guilt over this.
She’d been feeding him too much food to prevent him from getting hungry. She worries that her son will develop type 2 diabetes.
Adams’ drive to seek treatment for her anorexia was inspired by the fact that she was a mother.
“I want my daughter to love herself for who she is,” says Adams, “and because I want to be a healthy, happy mother for my children.”
The Renfrew Center has an evidence-based treatment model for eating disorders that emphasizes respect for the unique psychology of women, as well as the importance of a collaborative therapeutic relationship.
The Center encourages patients to actively participate in their growth and recovery.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, maintaining fat loss, muscle building, fitness and improved overall health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, maintaining fat loss, muscle building, fitness and improved overall health.
.
Top image: Freepik
World’s Strongest Toddler, Liam Hoekstra, on TLC: Hype or Hypertrophy
Liam Hoekstra was born in 2005.
The World’s Strongest Toddler aired in 2014 on TLC about 3-year-old Liam Hoekstra, a pint-size boy from Roosevelt Park who has 40 percent more muscle mass than typical 3-year-olds.
Liam Hoekstra, “the world’s strongest toddler,” has a rare condition called myostatin-related muscle hypertrophy. Hypertrophy means increased muscle mass.
But Liam Hoekstra is small for his age. Liam Hoekstra, “the world’s strongest toddler,” does not have big muscles, but he’s rather buff.
The world’s strongest toddler does not have a soft, “baby” look to his body, and has very little body fat.
His mother Dana says he’s always hungry and eats large quantities of food, but oddly, the show did not report how many calories a day he eats.
The World’s Strongest Toddler talked about several feats of strength that Liam Hoekstra has performed in the past. But again, strangely, there were no videos shown.
The World’s Strongest Toddler said Liam Hoekstra was walking at five months. If YOUR baby was walking at five months, you’d take a video. The show provided no video evidence.
The World’s Strongest Toddler said that Liam Hoekstra was moving furniture around before his second birthday.
Again, why weren’t videos of this shown? Seems to me that if a person sees their 19-month-old baby pushing around furniture, they’d immediately grab the video camera.
If they didn’t own a video camera, this would be a pretty good reason to go out and buy one, and then film the feats of strength.
The World’s Strongest Toddler gave the viewer only a photo of a baby Liam Hoekstra being held up by an adult into a standing position by his hands; he appeared to be about six months old.
The greatest feat of strength that the show gave us, was Liam Hoekstra climbing a gym rope.
Barefoot, he was able to slither up the last several feet, though however, at the bottom, he got a little assistance with his feet.
Nevertheless, even just for several pulls without the assistance at the top, that was impressive.
The video conveniently left out the entire climb; we see only the begining, and only the end.
Liam Hoekstra did 17 sit-ups in one minute, though it was not clear if his feet were anchored; only the first sit-up was shown, and his feet were not anchored, and this first sit-up appeared to be a sample sit-up before the actual test.
The other 3-year-old boy, whom Liam was being compared to, could only do one sit-up.
Liam’s grip strength is the equivalent of a 7-year-old. He’s able to do a pull-up, though not from a pure hanging position with straight legs; his legs were bent and flopping around, which makes the pull-up easier.
However, other kids in his preschool class weren’t even able to do even THAT; they had to put their feet against a wall in order to even attempt a pull-up, and most couldn’t even do the pull-up that way.
So, it’s clear that Liam Hoekstra is definitely stronger than most other 3-year-olds and slightly older kids, but at this point, without video evidence, I can’t believe he was walking at 5 months, moving furniture, and I think the show said he was climbing up stairs at 12 months or something like that.
The World’s Strongest Toddler spent too much time showing Liam Hoekstra doing things that I myself have seen other kids about his age doing, including hanging effortlessly on bars (though not doing pull-ups).
The World’s Strongest Toddler showed the boy running just slightly faster than another 3-year-old, but this wasn’t convincing, because in any random pair of preschool boys, usually one runs ahead of the other.
I would have loved to know what Liam Hoekstra’s time for a 30-meter dash would have been, and then compared to that of 10 other 3-year-old boys.
Liam Hoekstra and the other 3-year-old (who only did one sit-up) were instructed to do pushups.
Neither of the boys understood how to do a pushup, but then Liam, while in a sunken pushup position, casually flipped over and supported himself on one hand, in a side-bridge position, to look at his father, sustaining the bridge position. A 3-year-old normally cannot do this.
The World’s Strongest Toddler said that Liam Hoekstra’s adult-height projection was 5-6.
Later in the show, his father told a highschool football coach that it was 5-6 or 5-8.
This creates a problem, because the father dreams that his son will play pro football.
This short stature eliminates a number of sports; it would be useless to prime Liam Hoekstra for Olympic-caliber swimming, though he takes swimming lessons, and his swim instructor says he has the makings of a great swimmer.
Short stature is an impediment in elite-level swimming, but certainly not diving!
The World’s Strongest Toddler noted that should Liam Hoekstra become serious one day about sports competition, his genetic condition might be seen as an unfair advantage.
Well, we can attribute an “unfair advantage” to many Olympic athletes. Take Michael Phelps.
His height, relatively long torso, relatively short legs (less drag in the water), and relatively huge feet (like fins), can be considered genetic anomalies that give him an “unfair advantage” over other swimmers.
An NBA player who stands 7-2 has an unfair advantage, no? Or how about that super thin marathon runner, or that very short gymnast?
Or that giant-slalom skier with the relatively LONG legs that provide a solid base of support while skiing downhill?
One has to wonder how many Olympic or pro athletes might have the same genetic condition that Liam Hoekstra has, and were simply never tested for it.
It was only by chance that Liam Hoekstra was diagnosed. His grandfather was boasting about the boy’s strength to his friends, one of whom was a doctor.
The doctor became intrigued and recalled reading about cows that had abnormal muscle mass due to a genetic anomaly, and he wondered if perhaps Liam Hoekstra might have the same condition. One thing led to another, and soon, Liam Hoekstra was diagnosed.
Now what if Gramps never boasted to the doctor?
Liam Hoekstra could have gone on to be just an ordinary boy who had a very fast metabolism, ate a lot, had unusual muscle definition for his age, and was a little stronger and faster than other kids his age.
And as he got older and excelled in sports, nobody would be accusing him of having an unfair advantage, because nobody would know about his genetic condition, because it wouldn’t have been diagnosed, because Gramps kept his mouth shut.
The reality is that the whole town knows about Liam Hoekstra, and now, after TLC’s airing ot The World’s Strongest Toddler, the whole nation knows.
The World’s Strongest Toddler showed Liam Hoekstra climbing a refrigerator, but — oddly again, the video footage was shown in TWO segments! Dang !
The first segment showed him grabbing the refrigerator’s handles and hoisting himself upward, feet against the appliance. He then reached for the top of the appliance.
Just when I thought I was going to see Liam Hoekstra amazingly hoist himself higher and hang from the top, the footage switched to another angle, showing him ALREADY hanging at the top! A crucial transition element was left out!
The World’s Strongest Toddler made no mention of the possibility that Liam Hoekstra could grow into his strength, or, to put it another way, his biological age could catch up to his biological strength at some point.
Will he always have 40 percent more muscle mass than kids his age and then the average adult?
Or will his muscle development slow down and eventually match pace with his chronological aging?
Ideal sports for Liam Hoekstra, considering his adult-height projection: Sport climbing (big time!), Gymnastics, Power lifting, Sprinting (some elite sprinters are short), Rugby, Soccer, Cycling.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
What Does “Inflammatory Lung Disease” Really Mean?

Have you or someone you know been told they have “inflammatory lung disease”?
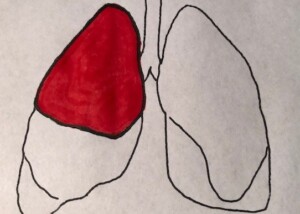
“Inflammatory lung diseases are clinically and histopathologically [under the microscope] a group of acute and chronic conditions,” begins Sashini Seeni, MD, a family medicine practitioner with DoctorOnCall, an online doctor and pharmacy.
“These disorders may affect the pulmonary vasculature, airspaces, pulmonary interstitium or a combination of these three anatomic compartments,” continues Dr. Seeni.
When my mother went to the ER the second time during a bout with pneumonia (she had vomited and complained of faintness and had clammy skin), a CT scan was ordered due to an elevated D-dimer.
The ER doctor said that the CAT scan showed that the pneumonia was gone (though my mother still had a bad cough).
The doctor then informed her, “The scan also shows that you have inflammatory lung disease, and this is not part of the pneumonia, which you no longer have.”
Interestingly, prior to the CT result, my mother had a chest X-ray that the doctor said still showed some pneumonia.
So I asked, “Then what was on the chest X-ray that you said a while ago showed some pneumonia?”
The doctor replied, “That’s scar tissue from the pneumonia. We know now from the CT scan that the pneumonia’s gone.
“Pneumonia tends to show on an image in a lobe of the lung, but the inflammatory lung disease shows as diffuse.
“I recommend a follow-up with your regular doctor or a pulmonologist to have your lung function checked.”
I asked the doctor for a more definitive explanation of this “inflammatory lung disease,” but he said it was difficult to be more descriptive at this point, and that’s why the follow-up was necessary.
I asked if this inflammatory lung disease could be caused by the pneumonia. He said no, pneumonia does not cause inflammatory lung disease.
I left the ER thinking that my mother possibly had some early stage lung disease! What was this inflammatory lung disease?
Inflammatory Lung Disease Could Be MANY Conditions
“Inflammatory lung disease can be divided into two subtypes which are infectious and non-infectious,” says Dr. Seeni.
“Non-infectious inflammatory lung diseases may be idiopathic [no known cause] or may represent a secondary reaction to autoimmune diseases, infections, environmental exposures or drugs.
“Meanwhile, some possible causes of infectious inflammatory lung diseases are tuberculosis, histoplasmosis and blastomycosis.”
COPD
“Chronic obstructive pulmonary disease (COPD), asthma and pulmonary fibrosis are the result of ongoing inflammatory processes,” says Dr. Seeni.
“COPD affects both the airways and lung tissue.
“This can manifest as a combination of emphysema and chronic bronchitis.
“COPD patients are most likely to have a smoking history.”
In addition, “Lung fibrosis is a chronic lung disease where the lung scars and thickens and that can affect oxygen exchange.
“The cause of lung fibrosis is unknown but for some reasons, it is believed to happen due to infection of the lung.”
Ground Glass What?
Next day I contacted my mother’s doctor’s office and spoke to the nurse.
I learned that the preliminary report of the CT scan, sent by the emergency room doctor, stated, “Granulatoma with change and ground glass opacities.”
It took me a while, but I finally recalled that several years ago, a “granuloma” was noted on a chest X-ray of my mother.
A granuloma is a dense collection of scar tissue that indicates previous infection and is harmless.
But what was this “ground glass opacities”?
Pneumonia can cause diffuse-pattern ground glass opacities (GGO) on a CT scan.
GGO can also result from an error in image interpretation, plus unreliable aspects of the imaging technology itself!
GGO can also appear as a result of normal breathing!
In short, GGO is a nonspecific radiologic finding that has a lengthy list of causes.
My mother had the follow-up, and the doctor apparently didn’t even mention the ground glass opacities, and was awaiting the more detailed report from the ER.
A phone appointment with my mother was made for two weeks later to discuss that more detailed report.
Two weeks later my mother’s doctor called and told her everything was normal, and that no further follow-ups were necessary.
The lesson here is: If you’re told you or a family member has “inflammatory lung disease” or “ground glass opacities” as revealed on a CT scan or X-ray, respectively, do not panic or lose sleep.
However, you should be quite discerning and inquisitive about this finding. Do not be reluctant to ask a lot of questions.
 DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
DoctorOnCall is the largest digital healthcare platform for citizens of Malaysia, allowing patients to consult doctors for advice, book appointments and place orders with local pharmacies.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Sources:
erj.ersjournals.com/content/24/3/502.full
ehow.com/about_5489647_inflammatory-lung-disease.html
medicalcenter.osu.edu/patientcare/healthcare_services/lung_diseases/lung/interstitiallung/Pages/index.aspx
mayoclinic.com/health/granuloma/AN00830
appliedradiology.com/Issues/1998/12/Articles/Ground-glass-opacity-on-CT-scanning-of-the-chest–What-does-it-mean-.aspx
How Does Feeling Depressed Cause Constipation?

Depression can cause constipation. However, if your depression has caused constipation, you may not even know it.
“The range of normal bowel movement frequency is from one BM in three days to three BMs in one day,” begins David D. Clarke, MD, President, Psychophysiologic Disorders Association, Clinical Assistant Professor of Gastroenterology Emeritus, Oregon Health & Science University, Faculty Associate, Arizona State University.
Dr. Clarke continues, “Fewer BMs than this is considered constipation. In depression, though definitive studies are lacking, when constipation occurs it is likely that it results from slowing of the muscle contractions of the large intestine (colon).
“The slower contractions cause the feces to move more slowly. In addition, the resulting greater duration of contact of the feces with the colon results in more water being absorbed — causing the stools to harden.”
The information you’re about to read is based on my mother’s constipation, and how her depression led up to it.
A person with major depression typically abandons their usual eating habits and lessen water intake.
My mother one day complained of constipation. But she had had this several times before during her course of depression. We thought it might be related to side effects of painkillers.
- But this time, we couldn’t blame painkillers because she had quit taking them not long prior.
- And this time, the constipation was not resolvable.
We took her to the ER and the doctor said she had a huge bowel movement that couldn’t make an exit, and he’d have to “dig it out.”
Later the doctor said there’d been about two feet worth of bowel movement, and that there was still more BM in there.
How could this be, if my mother had reported a bowel movement that morning, and if she’d been having bowel movements over the past many days?
The doctor said that a person could have bowel movements and simultaneously develop chronic constipation, in that while bowel movements may occur daily, fecal buildup occurs inside the colon over time: a simultaneous process.
He said that my mother’s bowel movement buildup may have taken place over a few weeks’ time, all while she was actually having bowel movements every day or almost every day.
She had compacted fecal material in the colon, and on that fateful day, it caught up with her and resulted in constipation that did not respond to edemas, suppositories or time.
Coinciding with the past few weeks were erratic eating habits, excessive inertia and low water intake.
These three problems were from depression, even though my mother was on an antidepressant.
The problem was that beginning a few weeks prior, the antidepressant lost steam and had to be increased in dosage.
There were a few days there where depression symptoms returned, thus suppressing my mother’s desire for food and fluids.
After we increased the dose, everything was fine, but then she started showing signs of relapse again.
This time we wondered if the increased dose was causing the extreme lethargy, fatigue and desire to sleep all the time. And once again, her appetite and desire for fluids was suppressed.
Even on better days, my mother didn’t eat so well, and she was never one to drink much water.
Erratic eating habits, going long periods without food, and inadequate water intake (all common results of depression) can very much lead to constipation in the form of built-up fecal material.
Depression also causes inertia and the desire to sleep a lot or just sit around not doing anything.
We noticed that my mother, after responding well to the antidepressant, was gradually beginning to want to spend more and more time sleeping or sitting around.
We wondered if the antidepressant was losing its steam again.
At any rate, all that inactivity contributed to the constipation because inertia suppresses voiding.
My mother was eventually diagnosed with hypothyroidism (several days before the major constipation episode), and it’s possible the clinical depression was secondary to the hypothyroidism, which would explain why she began showing signs of relapse despite being on 90 mg of the antidepressant.
The hypothyroidism perhaps began escalating and apparently was fighting against the antidepressant.
But even after she began taking Synthroid for the hypothyroidism, the extreme fatigue continued getting worse. This didn’t make sense…
…Until the ER doctor informed us that she had all that backed-up fecal material in her, stuck inside three feet worth of colon.
We were given instructions on what to do to get the remainder of bowel movement out over the next few days.
As a bunch of bowel movements began coming, once the home treatment started, my mother’s energy returned.
It’s a vicious cycle: Depression causes inertia. Inertia leads to constipation. Backed-up fecal material that’s been sitting in the colon for days and days will weaken the body and drag it down.
If you know someone who has depression and is getting increasingly tired and fatigued, despite being on an antidepressant, consider the possibility that he or she has impacted fecal material inside their colon, weighing them down and making them feel sick.

Since 1983 Dr. Clarke has successfully cared for over 7,000 patients with stress illness.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Excessive Crying in Adults: Causes & Solutions

Are you an adult who cries too much?
Are you an adult who cries excessively?
Just how abnormal is it for an adult to be prone to excessive crying episodes?
There are different kinds of crying, and different reasons for such, in the adult.
Many times, the crying is a normal reaction to an agonizing event.
Sometimes an adult will cry out of happiness.
I’ve witnessed adults crying after winning something on “The Price Is Right.”
The issue, however, is when the adult cries too often, excessively, out of proportion to life circumstances.
I once read a letter to an advice columnist from a woman who said she cried over everything, including the opening of a new K-Mart.
Why are some adults prone to so much tearfulness?
“Most likely the crying is related to a heightened emotional state which is caused by some stress in the person’s life,” explains Peter Swanljung, MD, chief of psychiatry at the Malvern Institute in Willow Grove, PA.
Someone may cry when the K-Mart opens, but they are not really crying about the K-Mart opening; rather, they are releasing emotions related to other issues going on in their lives.”
Some people begin weeping and sniffling while watching sappy movies or TV shows like “Little House on the Prairie.”
When I was in college, a group of us were in the TV lounge watching the 1939 version of “The Wizard of Oz.”
While Judy Garland was singing “Somewhere Over The Rainbow,” one of the female students began quietly weeping.
I don’t recall if I heard her sniffling, but I clearly recall another girl commenting in a sort of teasing way, “She’s crying!”
The weeping girl loved rainbows and had them all over her room.
Some adults will easily weep over very trite but isolated, specific events such as someone singing; whereas other adults will literally cry “over everything.”
Frequent crying episodes are not uncommon in someone with clinical depression, but this article refers to “otherwise normal” adults who just get too emotional.
Sometimes the tears are in reaction to a pleasant event (or seemingly a reaction to), such as the K-Mart opening or Judy Garland singing.
And sometimes the tears result from something negative, such as being chastised by one’s boss.
How many times have we heard of women running to the bathroom and crying after being chewed out by their boss?
Dr. Swanljung explains, “Meeting with a therapist may help a person understand what issues or stressors may be causing this heightened emotional state, and they may then be able to work on resolving or coping with these issues.”
If excessive crying in your adult life is interfering with social interactions or makes you uncomfortable, consider seeking professional help to discover the underlying cause.
Don’t assume this is something that’s just a part of you that can’t be remedied.