Cause of Irregular Periods, Weight Gain in Teens

Are you a teen who’s very worried about irregular periods and unexplained weight gain despite no change in diet?
There can be a medical cause to this. It’s called polycystic ovarian syndrome (PCOS).
“PCOS and weight gain are closely related,” says Heather Bartos, MD, a board certified OBGYN, and chief of Obstetrics & Gynecology at Texas Health Presbyterian Hospital in Denton, TX.
“PCOS is a syndrome, as the name says, and part of the constellation of symptoms is obesity, hair growth and hair loss (from the head), acne, type 2 diabetes or metabolic syndrome, infertility and irregular periods.
“In PCOS there is too much androgen, and androgens are produced in three areas — the adrenal glands, ovaries and fat cells.”
Irregular Periods and Weight Gain in Teens Are Not Always Caused by PCOS.
On average, menstruation begins at age 12, and for a few years after that, may be irregular — and this can be normal.
Irregular periods can also result from strenuous aerobic activity or athletic training.
A girl may also gain weight due to benign causes such as quitting sports or lifestyle changes such as more food in the house because Mom has remarried, or a new babysitting job in which there’s a ton of junk food in the house.
However, within about two years after a girl’s period starts, the cycle should no longer be irregular.
In other cases, however, doctors may attribute irregular periods (and weight gain) in teens as normal, due to their young age — when all along, the situation is being caused by PCOS.
When especially older teens have irregular periods, particularly coupled with unexplained weight gain, PCOS should be suspected.
The excess androgens causes imbalances in hormones and interferes with the menstrual cycle.
PCOS needs treatment at the time it’s diagnosed. In women it increases the risk for high blood pressure, high cholesterol and uterine cancer.
How a Teen Can Tell what the Cause of Her Weight Gain and Irregular Periods Are
There may be more than one cause at play. The weight gain may be from both PCOS and a change in lifestyle.
But if you add new-onset irregular periods to the equation, this heightens the possibility for PCOS.
So how can you tell what’s really going on? See a gynecologist for a complete exam. You cannot diagnose PCOS yourself.
“If a person with PCOS can lose weight, they can help reduce some of the circulating androgens — which would have positive effects on their health,” says Dr. Bartos.
What NOT to Do to Lose Weight
- Take up smoking
- Take “fat burning” pills
- Go on a crash or “starvation” diet
- Go on a fad diet like liquid protein or some other NON-sustainable diet.
- Become obsessive with exercise.
Instead, practice portion control, increase intake of fruits and vegetables, take up an aerobic activity and start strength training. Yoga will also help.
 Dr. Bartos served as an assistant clinical professor of OBGYN at the Uniformed Services University of Health Sciences for several years and was a physician in the U.S. Navy for eight years.
Dr. Bartos served as an assistant clinical professor of OBGYN at the Uniformed Services University of Health Sciences for several years and was a physician in the U.S. Navy for eight years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: loyolamedicine.org/newswire/news/irregular-periods-young-women-can-be-cause-concern
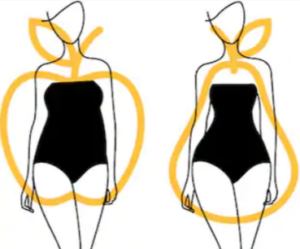
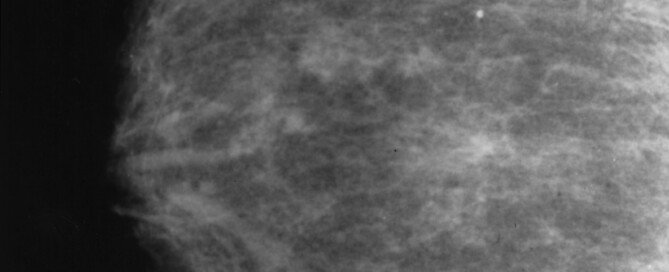
Breast Cancer Risk in Pear vs. Apple Shaped Women

Cancer.gov
Researchers have revealed that the breast cancer risk in postmenopausal women is a function of waist circumference, independent of body mass index (BMI).
And that means that whether or not a woman’s body is in the shape of a pear or has an apple shape makes no difference.
This is because BMI is a numerical value that’s calculated from a person’s height and weight (though some calculations include age and gender).
But as you can see, these features of the calculation have nothing to do with the shape of a woman’s body.
A woman can have a pear shape and a BMI value equal to a woman with an apple shape.
Shutterstock/bus109
When I was a personal trainer I worked with women of all kinds of body shapes: pear, apple, buff, skinny-fat, “average,” you name it.
I found this study quite interesting because historically, studies have shown that the pear shaped person has a lower heart disease risk than the apple body.
The study about breast cancer comes from the American Cancer Society and focused on mostly white women.
The study was not able to verify previous findings that body shape alone is an independent risk for breast cancer.
The report points out that, indeed, many studies have linked abdominal excess weight or obesity to heart disease, type II diabetes and some cancers including breast.
The trend was to conclude that an apple shape (excess fat concentrated in a person’s middle) is more harmful than the pear shape (fat loaded more in the thighs, hips and butt).
Mia Gaudet, PhD, and her team analyzed data from almost 29,000 women.
A strong correlation was unveiled between postmenopausal breast cancer risk and waist size. But the association vanished once BMI was adjusted for.
Thus, regardless of being apple or pear shaped, a high BMI means a higher risk of breast cancer.
The study looked at BOTH the body mass index and waist circumference.
How to Shrink Waist Size

Freepik.com, prostooleh
Women who’d like to shrink their waist size to lower breast cancer risk need to step away from the crunch machine and pick up some heavy barbells.
Heavy barbell work will shear more fat off the entire body than will folding-movements that isolate a tiny muscle group.
How to Do It
Start with LIGHT weights first, and gradually increase over time. Safe heavy barbell work (e.g., deadlift, squat) means that you can do at least eight repetitions but it’s impossible to do more than 12.
Resting in between sets should be for a minute to two minutes, depending on the routine and how you feel, and you should not do jumping jacks or jogging in place in between sets. Rest fully so that you can give the next set your best effort.
Weight workouts fire up the body’s ability to burn fat by adding lean muscle.
As for aerobic exercise, this too, is important for reducing waist and belly size.
The most effective and time-saving way to make aerobics burn up belly fat is to employ interval training:
Do brief bouts of high exertion mixed with a few minutes of casual exertion. High intensity interval training can be applied to ANY mode of cardio exercise.
The full report is in Cancer Causes, and Control (April 2014).
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Source: sciencedaily.com/releases/2014/04/140416090805.htm
Zero Calcium Score Possible with Major Soft Plaque Buildup
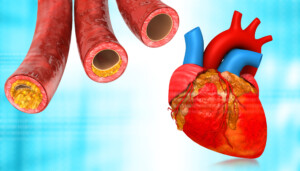
Does a zero calcium score automaticlly mean you’re off the hook for dangerous soft plaque buildup in your arteries?
Though coronary calcium scoring is an accurate indicator of the presence of heart disease (varying degrees correspond to the calcium score number), it’s still possible for a person with a zero calcium score to also have dangerous soft (non-calcified) plaque buildup.
“The CT calcium score measures calcified plaque,” says Nieca Goldberg, MD, medical director of NYU Women’s Heart Program and radio show host of “Beyond the Heart” on Doctor Radio SiriusXM.
“Calcified is stable plaque, less likely to break and start the process for a heart attack. Soft plaque is more fragile and likely to crack and cause a heart attack.
“Studies have shown that higher levels of calcified plaque also indicate that soft plaque is present.
“That is why we treat people with elevated calcium scores with statin therapy to stabilize plaque and lower cholesterol, and aspirin to prevent blood clots.
“A zero calcium score means low risk, not no risk, accounting for the possibility of soft plaque.”
A report in Diagnostic and Interventional Radiology (2013; 19:111–118) details an investigation into the presence of soft plaque.
This doesn’t mean that if you just celebrated learning that your calcium score is zero, that you should now start worrying that your score is meaningless.
Brief Recap
A score of over 100 means you probably have coronary heart disease. I had my calcium score taken and it was zero.
My report said that zero means “no detectable heart disease.” The report said that 400 and over meant a strong likelihood of severe heart disease. I breathed a huge sigh of relief with my zero result.
For the Turkish investigation, 288 adults with a calcium score of zero underwent a CT angiogram.
Calcium scoring is done with a CAT scan without contrast dye. The CT angiogram is also done with computed tomography, but with contrast dye.
The calcium score test detects only the calcified plaques. The CTA detects the soft plaques (as well as the calcified).
Of the 288 subjects, CTA detected soft plaques in 50. Of those 50, the soft plaque buildup caused significant narrowing of a coronary blood vessel in six patients.
What was the difference between those 50 and the remaining 238 subjects?
The prevalence of certain heart disease/attack risk factors was significantly higher in those 50.
For the men, the risk factors were 1) high blood pressure, 2) high total cholesterol, 3) diabetes and 4) family history.
For the women, they were 1) high blood pressure, 2) smoking and 3) diabetes.
The conclusion of the study is that people with a zero calcium score, but who have risk factors for heart disease, need follow-up testing for soft plaques.
The risk factors that stand out in this particular study are high blood pressure (hypertension), smoking and family history. Diabetes was deemed a “borderline” risk factor.
The paper points out results from other studies that name additional risk factors as being correlated to soft plaque deposits in people with a zero calcium score: older age, male gender, high LDL cholesterol and obesity.
 Dr. Goldberg is senior advisor, Women’s Health Strategy, NYU Langone Health; founder and former medical director, Joan H. Tisch Center for Women’s Health; and clinical associate professor, NYU Grossman School of Medicine.
Dr. Goldberg is senior advisor, Women’s Health Strategy, NYU Langone Health; founder and former medical director, Joan H. Tisch Center for Women’s Health; and clinical associate professor, NYU Grossman School of Medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Explode
Sources:
dirjournal.org/text.php3?id=507
webmd.com/heart-disease/cardiac-calcium-scoring?page=3
Why Isn’t a CT Angiogram Commonly Used in ER for Chest Pain?

Why isn’t the CT angiogram used commonly in emergency rooms to evaluate chest pain?
Studies have shown the value of the CT angiogram in distinguishing ER patients with cardiac chest pain from those with non-heart related chest pain.
One such study appeared in the July 26, 2012 New England Journal of Medicine.
The paper states that the use of coronary CTA in an emergency room setting for acute chest pain was very effective at identifying which patients did or did not have a blockage in their coronary arteries.
This allowed clinicians to then focus on the use of resources for patients with clogged arteries.
Despite this compelling finding, however, chances are pretty high that if you walk into an ER complaining of chest pain, you will not undergo the CT angiogram.
These studies show effectiveness, but they don’t focus on something else: the impact of radiation from the CTA.
“The use of CT angiograms (CTAs) of the chest in the ER setting is reserved for the evaluation of specific conditions to prevent patients from receiving unnecessary radiation,” says Brett Mollard, MD, a board certified diagnostic radiologist who specializes in abdominal and chest imaging.
“While ionizing radiation from a single CT scan of the chest has a very low overall risk to a patient, the risk is not zero and can have a cumulative effect in patients who receive multiple CTs over time,” continues Dr. Mollard.
“ER providers therefore limit ordering CTAs unless they have specific concern for disease processes such as pulmonary embolism or aortic injury (dissection or rupture).
“Coronary CTA is also becoming increasingly used in patients with low to intermediate risk of having an acute coronary syndrome (ACS).”
Three Flavors of CT Angiogram
Dr. Mollard explains, “CTAs of the chest come in three flavors: CTA of the pulmonary arteries to evaluate for pulmonary embolism; CTA of the thoracic aorta to look for an acute aortic injury such as a dissection, intramural hematoma or tear; and coronary CTA to assess for the presence of coronary artery disease.
“These differ by timing of imaging following contrast administration and whether or not ECG-gating is performed.
“A CTA of the thoracic aorta frequently also sufficiently evaluates the pulmonary arteries, and special protocols exist that are designed to diagnostically evaluate both the thoracic aorta and pulmonary arteries at the same time with a single scan.”
Thus, for people entering an emergency room complaining of chest pain, they will typically get a chest X-ray, ECG and a blood draw for a heart enzyme – like my mother did on several occasions when her symptoms included the possible differential diagnosis of heart attack.
However, the first time she went in for trouble breathing (which can mean a heart attack or looming heart attack) — had she been given the CT angiogram on that visit, she would have been admitted instead of sent home with a suspected diagnosis of acid reflux, because logically, the CTA would’ve come up with a very troubling finding that the chest X-ray, ECG and enzyme test missed: dangerously blocked arteries.
Several days later she was back and had been admitted due to the enzyme test having a “grey area” result.
A catheter angiogram revealed very severe coronary artery blockage — something that a CT angiogram would have picked up.
Nevertheless, from an overall picture, there’d be a lot of unnecessary radiation exposure if the CTA was a standard test for everyone, including those with cardiac risk factors, who reported chest pain in the emergency room.
 Brett Mollard, MD, completed his residency in diagnostic radiology and nuclear medicine at the University of Michigan where he served as Chief Resident. He subsequently completed a fellowship in abdominal imaging at the University of California, San Francisco (UCSF). He currently works in private practice.
Brett Mollard, MD, completed his residency in diagnostic radiology and nuclear medicine at the University of Michigan where he served as Chief Resident. He subsequently completed a fellowship in abdominal imaging at the University of California, San Francisco (UCSF). He currently works in private practice.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Jamesboy Nuchaikong
Source: sciencedaily.com/releases/2012/07/120725200300.htm
Why Excess Fat Around the Heart Is So Dangerous

Emory University School of Medicine cardiologists note that X-ray via CT scan can measure the size of the fat layer surrounding the heart.
The fat layer around the heart is called epicardial adipose tissue.
Knowing the size of this harmful layer can be used as a gatekeeper, say the Emory researchers.
The imaging result of this threatening layer of tissue can help a cardiologist determine if a nuclear stress test should be the next step for the patient.
A nuclear stress test measures how well the heart uptakes oxygen via blood flow during rest, and also during stress (the stress may be in the form of exercise or chemically induced).
Obesity Endangers Health, no Matter How Body Positive You Are
According to the study, people with a higher volume of fat around the heart tend to have the most dangerous form of coronary plaque buildup: non-calcified plaque.
Calcium, a mineral, tends to accumulate in coronary artery plaques. However, the mere presence of calcium in an individual plaque simply doesn’t always mean impending trouble.
Plaques that are not calcified are indicative of active plaque buildup.
Plaque buildup. Shutterstock/Explode
The adipose tissue surrounding the heart, compared to the fat just beneath the skin, secretes more inflammatory hormones.
When the fat around the heart secretes these inflammatory hormones, this may promote an active plaque buildup process in the coronary arteries.
This is demonstrated by the presence of the non-calcified atherosclerotic plaques.
These conclusions came from examining 214 patients via cardiac CT.
The patients also received calcium scoring, assessment of fat around the heart, and coronary plaque evaluation.
In patients with non-calcified plaques, the volume of fat around the heart was the highest (about 60 percent greater than patients with calcified plaques).
Mechanical Dangers of Excess Fat Around the Heart
“Obesity in itself is a risk factor for heart disease,” says Danielle DonDiego, DO, a family physician and obesity specialist with SteadyMD, an online program where patients can call, text or video chat with their doctor anytime.
The term “heart disease” doesn’t just refer to clogged coronary arteries, but this umbrella term can also refer to chronic heart failure.
“Heart failure is actually caused by a weakening of the heart muscle to pump or fill with blood,” says Dr. DonDiego.
“Excess fat around the heart does make it more difficult to pump, just like wearing a backpack while hiking vs. not wearing one — it’s harder with extra weight on the heart muscle.”
Risk Factors for Heart Disease that You Probably Never Thought Could Be
- chronic sleep of six or less hours per night
- chronic sleep of more than nine hours per night
- overall total sleep per 24 hours exceeding nine hours
- sleep apnea
- insulin resistance or prediabetes
- chronic anxiety
- excess abdominal fat, even if your legs and arms are thin and your weight is “normal” for your height.
Intuitively, you should know that the more fat around your heart, the more likely you will have coronary artery disease.
The fatty tissue around one’s ticker can be trimmed, and future fat can be prevented, with cardiovascular exercise.
The heart is a muscle, and in order for this muscle to be fit and healthy, it must be exercised.
Losing a hundred pounds is not easy, but not impossible.
 Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
Dr. DonDiego, who’s also a certified personal trainer, focuses on weight management, fitness, nutrition, reproductive health, preventive medicine and managing end stage disease. Learn more about SteadyMD.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image credit: Nestorjava
Sources
sciencedaily.com/releases/2010/03/100315104032.htm
sciencedaily.com/releases/2011/07/110711164527.htm
sciencedaily.com/releases/2011/02/110208091426.htm
sciencedaily.com/releases/2010/09/100903072320.htm
sciencedaily.com/releases/2011/07/110721163021.htm
What a Calcium Score Means in Low Heart Disease Risk People
If you’re at low risk for heart disease but have a calcium score above zero, just what does this mean for you?
Though the calcium score has been shown to be a strong predictor of the likelihood of heart disease as well as cardiac events, this has applied to people with multiple risk factors already in place for coronary artery disease, such as high blood pressure, poor cholesterol profile, smoking and diabetes.
But what does the calcium score mean for people who apparently have no or a small risk of heart disease?
Los Angeles Biomedical Research Institute (LA BioMed) researchers wanted to find out.
And they found out that the calcium score test, indeed, was accurate in predicting one’s chances of dying from heart disease, even if that person had a small risk, or even zero, known risk factors.
How was this study on calcium scoring done?
LA BioMed researchers investigated 5,593 adults who had no known heart disease risk or who had a minimal risk.
A healthy coronary artery does not contain calcium. But if calcium builds up, it can block an artery.
I’ve had a calcium scoring (a five minute test), and the result was zero.
This means that there was no measurable plaque buildup.
The paperwork that came with my results showed three categories of score values above zero, corresponding to the risk of mild, moderate and severe heart disease.
Now, in the LA BioMed study, it was found that people with calcium scores of one to 99 were actually 50 percent more likely to succumb to heart disease than were those with a zero score.
Those with a moderate score of 100-399 had an 80 percent more likely chance of dying from CAD when compared to those with a zero result. And a score of 400 or more?
These patients were three times more likely to die of heart disease, when compared to those with zero measurable plaque buildup.
“This long-term study builds on previous research conducted at LA BioMed and other institutions,” begins LA BioMed researcher Matthew J. Budoff, MD, “that have proven the effectiveness of coronary artery calcium screening in predicting heart disease risks.”
Dr. Budoff says that his study results show that calcium scoring “can be an effective tool” for evaluating CAD risks in people with little or no known risk factors so they can adjust their lifestyle habits.

Dr. Budoff is at the forefront of the medical community’s efforts to create early detection methods for coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Syda Productions
Source: sciencedaily.com/releases/2014/04/140415133922.htm
Can the Heart Be Damaged by a Fast Resting Pulse?

Is your resting pulse fast and you’re worried that this will eventually cause harm to your heart?
And can this damage the heart if you’re otherwise healthy?
Can a fast resting pulse, in and of itself, lead to heart damage?
Let’s assume that the patient has other good health practices, such as they never smoke, do not drink alcohol, get plenty of exercise, have a plant based diet, and keep their body at what’s considered an ideal weight. So what’s the answer?
“Yes, fast resting pulse can lead to heart damage, but it would have to be quite fast (>110-120) and for a relatively long period of time (weeks to months) to be chronic, occurring all the time and continuous,” explains Dr. Sameer Sayeed, a cardiologist at ColumbiaDoctors of Somers, NY.
“The fast heart rate leads to weakening of the heart muscle and depressed ejection fraction due to overworking the heart muscle, similar to any other muscle in the body.”
Ejection fraction is the amount of blood that’s pumped out with each heartbeat.
Dr. Sayeed continues: “It is not that common for this to occur from stress but more commonly due to a thyroid disorder, atrial fibrillation or something else that would cause persistent rapid heart rate.”
If you’re under a lot of tension, this doesn’t mean you don’t have a medical condition.
“Certainly removing one from stress might help, but generally one would also have to rule out any underlying condition that might be causing the rapid heart rate, and treating the underlying problem might help,” says Dr. Sayeed.
If the situation is only from stress, Dr. Sayeed says that a beta-blocker drug might be of benefit.
What if you don’t want to take a drug to remedy a fast resting pulse from anxiety or stress?
Exercise is a fabulous way to lower resting pulse.
Exercise not only has a direct effect on pulse, but it has an indirect effect on it (lowering, of course) by diluting the negative effect of stress and anxiety.
A very effective exercise for this is HIIT.

Dr. Sayeed performs echocardiograms and stress tests at the Midtown Manhattan and Westchester offices at Columbia Doctors. He is also trained in cardiac CT imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/jcomp
How Long Should Chest Pain Last Before Going to the ER?
How long should you wait with chest pain before deciding it’s time to visit the ER?
After all, you could be in that 15-30% of patients who end up having a heart attack.
“It’s important to have a pretty low threshold for having chest pain evaluated if it does not have a clear cause, such as injury or unusual exertion,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“Musculoskeletal pain can develop in the chest just like in the rest of the body. For example, the prolonged coughing associated with a cold or the flu can lead to chest pain.”
You have muscles and other soft tissue in your chest. They are not immune from feeling strained or achy after mechanical exertion.
Waiting Time with Chest Pain Before Going to the Emergency Room
“Chest pain in a person with risk factors for cardiovascular disease should be promptly evaluated,” says Hanifin.
“People with a history of high blood pressure, smoking, diabetes, high cholesterol or a family history of heart diseases need to be educated regarding the warning signs of heart attack.
“Another red flag for chest pain is the presence of associated symptoms. The presence of shortness of breath, nausea, sweating or lightheadedness can signal a potentially life-threatening problem and merit prompt evaluation.
“Finally, different types of pathology are frequently characterized by different types of pain.
“Heart attacks and angina are usually associated with a pressure sensation.
“Aortic dissection is associated with a tearing sensation, and inflammation around the heart – pericarditis – is associated with a sharp pain. All of these should be urgently evaluated.”
This means don’t make up some time limit rule. Just get out the door (hopefully someone will be able to drive you to the emergency room).
Study: correlation between how long chest pain lasts and whether or not it’s a heart attack?
Researchers from Henry Ford Hospital decided to investigate. The study notes that about 15 to 30 percent of chest pain cases in the ER turn out to be a heart attack.
The paper points out that an electrocardiogram is “not 100 percent accurate,” though this, and a troponin blood test, are important to ER physicians in evaluating for a possible heart attack.
The study involved 426 patients with chest pain and a 30-day follow-up. Out of that, 38 were diagnosed with a heart attack.
Average duration of chest pain was 120 minutes for them. It was 40 minutes for patients who did not have a heart attack.
For patients who had chest pain for under five minutes, there were no heart attack diagnosis.
Conclusion
The report says that those with chest pain lasting under five minutes “may be evaluated as an outpatient” by a cardiologist.
But if chest pain lasts longer than five minutes and does not have a clear cause (such as diagnosed acid reflux), a person should “seek prompt medical evaluation in an emergency department.”
However, what if only one minute into your chest pain, you also feel nauseous, faint and are breaking into a sweat?
Though these symptoms can be caused by a panic attack (which doesn’t require an emotional trigger), they are far more meaningful within the context of a person at high risk for a heart attack:
- Over age 50
- Obese
- Smoker
- Diabetic
- Sedentary lifestyle
- High sodium diet, among other risk factors
Take things into context. A 60-year-old, nonsmoking, fitness enthusiast of healthy weight and other vitals who regularly runs and lifts weights is more likely having a panic attack than is a 40-year-old, smoking, non-exercising, overweight person whose father had a heart attack at age 42.
This study was small and further investigation is warranted. The full report is in the Sept. 2013 Critical Pathways in Cardiology.
Never think that you’ll be wasting an ER doctor’s time with your chest pain complaint as you try to convince yourself it’s only gas or a strained muscle.
When in doubt, go to the ER, especially if you have risk factors for a heart attack.
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2013/09/130911161006.htm
High Calcium in Arteries Linked to High Heart Attack Risk

The higher the calcium in your arteries (shown by a calcium score test), the likelier you’ll suffer a heart attack.
Maybe it’s time to get your calcium score!
Researchers may be able to predict future severe cardiac events in patients with known, stable coronary artery disease (CAD) using coronary calcium scoring, according to a study published in the online edition of Radiology.
“The amount of calcium in the coronary vessels, as measured by CT, is of high predictive value for subsequent serious or fatal heart attack in these patients,” says Marcus Hacker, MD, “independent of the patient’s age, sex and other coronary risk factors.”
Dr. Hacker is lead study author, and resident physician in the Department of Nuclear Medicine and leader of the research unit for nuclear cardiology at Ludwig Maximilians University in Munich, Germany.
According to the National Heart, Lung and Blood Institute, CAD is the leading cause of death in the U.S. for both men and women, killing more than 500,000 Americans each year.
Single photon emission computed tomography (SPECT) myocardial perfusion imaging is a nuclear medicine diagnostic procedure that provides excellent 3-dimensional images of coronary arteries to assist in diagnosis and treatment of CAD.
Currently, calcium scoring – measuring the amount of calcium in the arteries – is used as a screening exam and in cases of suspected CAD, but not in cases of known CAD.
Dr. Hacker and colleagues set out to determine if calcium scoring would lend additional prognostic value to SPECT findings in patients with known, stable CAD.
For the study, 260 patients with CAD underwent coronary artery calcium scoring in addition to SPECT myocardial perfusion imaging.
Over a median period of 5.4 years, the patients were followed up for severe cardiac events.
Twenty-three of the 260 patients had a fatal or severe heart attack, and 40 additional patients underwent bypass surgery.
The results showed that patients with an initial calcium score greater than 400 were at significantly increased risk for severe cardiac events.
“We found that coronary calcium seems to play an important role in predicting subsequent heart attack or sudden cardiac death,” and this adds prognostic value to SPECT findings, says co-author Christopher Uebleis, MD, member of the research unit for nuclear cardiology at LMU.
Dr. Hacker pointed out that combining calcium scoring and SPECT can help identify patients with known CAD who are at highest risk for serious or fatal heart attacks.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sukiyaki
Source: thefreelibrary.com/High+calcium+level+in+arteries+’signals+heart+attack+risk’.-a0204641880
Women’s Heart Disease: Stress, Stiff Heart, High Blood Pressure
Don’t kid yourself: Women’s heart disease is very different from men’s in more ways than you may be thinking, and that includes the effect that stress has on the heart.
Dr. Gordon A. Ewy, MD, explains how women’s heart disease differs from men in the causation of stress, stiff cardiac muscle and high blood pressure.
Maybe you already know that women’s heart disease is a different animal than is men’s, but perhaps you don’t know that mental stress and high blood pressure play a much bigger role in women’s heart disease than they do in men’s. Also relevant is that of stiff cardiac tissue.
Stress and Heart Disease in Women
“Stress often triggers heart dysfunction in women,” says Gordon A. Ewy, MD, in an article he wrote for the University Sarver Heart Center newsletter (spring, 2010).
Dr. Ewy is the Director Emeritus of the University of Arizona Sarver Heart Center.
“Clinical observations of how some individuals experience severe stress or respond unusually to minor stress, have led to our understanding of a condition now called ‘stress cardiomyopathy,’” continues Dr. Ewy in his article.
He adds that most studies show that more than 90 percent of patients who have stress cardiomyopathy are women.
This condition is associated with high levels of the “fight or flight” hormone adrenalin, plus an irregular or fast heartbeat.
This stress-induced form of cardiac ailment, says Dr. Ewy, is reversible in most cases, though he also says in his article, “Tragically, the condition may result in sudden death in the most extreme cases – ‘She was scared to death.’”
Stiff Cardiac Muscle and Women
Dr. Ewy’s report continues, “Heart failure in women is often due to an abnormally stiff heart muscle.
“The heart contracts as it should, but is too stiff to relax normally and requires a higher amount of pressure to fill the major pumping chamber.
This higher pressure backs up into the lungs, resulting in symptoms such as shortness of breath, especially with exertion.”
Women should engage in structured aerobic exercise to help prevent this stiffness from developing.
High Blood Pressure and Women
“Hypertension (high blood pressure) is more common as one gets older, and if inadequately treated, often leads to heart failure due to an abnormally stiff heart, a syndrome more common in women since they tend to live longer than men,” says Dr. Ewy in the report.
What can women do to prevent heart disease?
The article explains, “First, the classic risk factors of high blood pressure, abnormal lipids, diabetes and others, which are often hereditary, need to be addressed.”
He urges a healthy diet, weight control, exercise and avoiding smoking/secondhand smoke.
























 In the area of research,
In the area of research, 







































