How to Take Out Thick Ponytail without Pulling out Hair

Here is an ingenious way to take out a big thick ponytail without losing more than a few hairs.
I swear, every time I do this technique, I am very rarely aware of any hairs being pulled out along the way.
But even if one or two are getting by me (though again, I don’t feel the hairs being pulled out), this technique for sure is the best at minimizing hair loss when taking out a ponytail–particularly if it’s big, thick, poofy or bushy.
First, always use a rubber band designed for ponytails, and one that does not have a metal piece holding it together. Ideally, use the ones covered in cloth.
When it’s time to take out your ponytail, bend over so that your ponytail flops over the top of your head. This will clear your work area around the rubber band.
Pull one of the loops of the rubber band just enough to fit the tip of your index finger beneath it, between the underside of this loop and the other loop (or two) that binds the ponytail.
I use two loops of a single rubber band. Almost always, one of the loops lies a little higher than or on top of the other.
This is the one that I lift just enough to insert the tip of my index finger under.
I do this EXTREMELY CAREFULLY because invariably, there will be hair that is tangled with the loop. I do not want to break this hair.
My goal is to “clear” the loop of any hair, so that it’s just my fingertip against it—not a single hair caught in there.
The next step is how you will prevent losing the hair that normally results when you take out a ponytail.
Even if you very carefully remove the rubber band of your ponytail as you’ve always done, it’s almost impossible to avoid yanking some strands out of their roots.
So for this next step, you will need a toenail clipper—the kind with thin pointy ends–NOT the kind in which the ends get wider.
While you’re holding that loop, that you’ve already made sure is clear of any caught strands, you will carefully slip one of the tiny shears of the clipper underneath the band that’s being held out by the tip of your index finger.
Insert the shears under all the way so that when you close the other shear over it, it severs the entire width of the loop that you’re holding with your fingertip.
If you’ve “cleared” any caught strands, the clippers will snip ONLY the rubber band.
I do this entirely by feel. No mirror is necessary.
Snip the rubber band. Very carefully extract the severed rubber band from your hair—so that you don’t snag any strands with it.
DO THIS SLOWLY. If you just yank it out, you’ll pull hairs with it.
This technique means you must have a steady supply of rubber bands–and for thick or bushy hair, you’ll need strong rubber bands.
You will have to keep buying them. But hey…your hair is worth it, right?
For women who have palm calluses from lifting weights, strands of hair can get caught by these.
The solution is to use a fingernail fail to file at the calluses so that they are smoother.
While working with your ponytail, try not to press the callused area of your palms into your hair.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Skin Peeling On Your Hands: Doctor Explains Causes

If you’re suffering from peeling hands, there are many causes of this, says a dermatologist.
“Each and every day your hands are constantly being exposed to various elements that can cause irritation including chemicals, UV rays, weather conditions, irritants and allergens,” says Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology and practices at Westlake Dermatology located in Austin, Texas.
“Repeated irritation of the skin on the hands can lead to excessive peeling, especially if you are genetically predisposed to this.”
Says Dr. Gordon. “Typically this peeling is accompanied by other symptoms like itching, burning or pain, making the situation even worse.
“Unfortunately diagnosing the source of this peeling can be difficult, as there are a number of potential root causes.”
Causes of Skin Peeling on the Hands
(no particular order)
Yes, believe it or not, stress can cause the skin of your hands to peel. “It’s not uncommon for people to experience peeling of the skin (in any area of the body, including the hands) due to periods of high or intense stress,” says Dr. Gordon.
This is because usually, stress exacerbates other conditions (following) that can lead to peeling hands.
Allergies: “Skin peeling may be the result of your skin coming into contact with a substance that you are allergic to,” says Dr. Gordon.
“Potential allergens can be found everywhere, including household items, foods and even skincare products.”
Infections: “Certain staph and fungal infections are known to cause skin peeling. Sometimes these infections occur alongside other symptoms like high fever.
“The infection may be in your skin or may be elsewhere in your body, so if you have any other symptoms, make sure to see your provider quickly.”
Eczema: “Hand eczema is characterized by a peeling of the skin on the hands as well as the fingers.
“This type of eczema is caused by genetics, but is worsened by triggers, with many individuals developing it after being in contact with chemical irritants or allergens.
“Other symptoms can include itchiness, development of fluid-filled blisters, swelling and cracking skin.”
Psoriasis: “Generally occurring due to genetic disposition, psoriasis can result in peeling along the hands.
“Psoriasis occurs with skin cell buildup in a specified area; resulting in irritating red patches, itchiness, peeling and sometimes pustules.”
Exfoliative keratolysis: “While this condition is characterized with peeling of the fingers, peeling of the palms or tops of hands is possible. Exfoliative keratolysis is mostly common in young adults and occurs during the hotter summer months.
“The peeling starts off with the development of a superficial blister which naturally pops and results in peeling skin.”

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/WSW1985
Persistent Red Rash on Cheeks: Doctor Explains

“The development of a rash on the cheeks, indicated by bumps, swelling and redness to the skin, is the result of the body’s natural inflammatory reaction,” says Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology and practices at Westlake Dermatology located in Austin, Texas.
Causes of Red Rash on the Cheeks
“The source of cheek rashes can vary from a mild cause such as exposure to an allergen or the sun, to a more serious cause like a medical disease,” says Dr. Gordon.
“Rashes can occur on individuals of any age and can manifest on a single cheek or both cheeks.”
Often, a person will describe what they see as a “rash” simply if it’s reddish or pinkish and characterized by spots, splotches, patches or bumps.
“The rash itself can greatly vary in appearance depending on the source,” says Dr. Gordon.
“Rashes can vary in color (red, white or purple are common), may be symptomatic (itching, burning, pain) and can have different textures (flat, bumpy, raised or scaly).
“Additionally the rash can be accompanied by scaling or peeling skin.
“The most common causes of cheek rashes include acne, rosacea, allergic reactions, dermatitis and eczema.
“These causes do not result in permanent risks to one’s health, and the rash can be successfully treated by a treatment plan created by your dermatologist.”

Rosacea. Shutterstock/sruilk
Rash on Cheeks Caused by Rosacea
Dr. Gordon explains, “Rosacea is one of the most common culprits for persistent redness on the face. It is very common and occurs primarily on the face of adults.
“Common symptoms of rosacea include redness and rash development along the cheeks, nose, and sometimes the forehead and chin. Often acne-like bumps, sun-sensitivity and flushing can also occur.
“Additionally, rosacea usually causes small blood vessels to be visible on the surface of the skin.
“While there is no cure for rosacea, medicines and laser can help control the rash. And don’t forget your sunscreen!
Serious Causes of “Rash” on the Cheeks
“In rare cases, the development of a rash on the cheeks is an indicator of a more severe medical disease or condition like shingles, severe infections or diseases such as systemic lupus erythematosus,” says Dr. Gordon.
Another cause of what appears to be a “rash” is a condition called actinic keratosis (sun damage).

Actinic keratosis lesion. Shutterstock/Dermatology11
This is actually quite common in people over age 40. It’s characterized by pinkish-reddish patches on the face that feel almost like sandpaper to one’s fingertips rubbing along these lesions.
These lesions are easy to miss until they begin progressing. They are removed via liquid nitrogen sprayed onto them by a dermatologist, or with a prescription ointment.
These lesions absolutely must be removed, because they’re made up of atypical skin cells.
This means they are more likely than surrounding typical cells to eventually morph into a form of skin cancer called squamous cell carcinoma.
It’s estimated that if left untreated, 10 percent of AKs will develop into squamous cell carcinoma.
Because cheeks get a lot of sun exposure, the “rash” of actinic keratoses commonly occurs in this location, though other common locations include the nose, and scalp of bald men. These patches do not itch or produce pain.
“If your rash is unresponsive to treatments and persists, it is very important to see your medical care provider right away,” says Dr. Gordon.

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
Conditions that Mimic Carpal Tunnel Syndrome

There are seven conditions that mimic the symptoms of carpal tunnel syndrome.
First up is pronator teres syndrome. “Whereas carpal tunnel syndrome is compression of the median nerve at the wrist,” begins Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery, “pronator syndrome is median nerve compression at the elbow.”
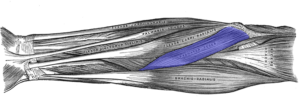
The pronator teres muscle starts at the upper arm bone near the elbow and attaches to both lower arm bones.
PTS is similar to CTS in that it can cause pain, numbness, tingling and burning in one’s thumb, index and middle finger, and half the ring finger, says Dr. Oheb.
But CTS will not cause pain in the forearm. And PTS can cause loss of sensation to your palm, because a branch of the median nerve comes off before the carpal tunnel, says Dr. Oheb.
Carpal tunnel syndrome can be mistaken for PTS. This happened to my mother.
The neurologist who was setting her up for an EMG actually told her he thought she had pronator syndrome.
After he was finished with the EMG study, he said, “It’s carpal tunnel.”
What other conditions can mimic the symptoms of carpal tunnel syndrome?
Dr. Oheb says, “Cervical disc disease or cervical spinal stenosis (associated with concomitant neck pain and often radiating symptoms from the neck).”
When my mother was in the ER (prior to seeing the neurologist for the EMG study), the ER physician was pretty convinced she had a pinched nerve in her neck that was causing her hand pain and finger numbness.
He concluded this based on asking her questions about her symptoms and then viewing an image of her neck that he said showed cervical spinal stenosis (narrowing of the canal through which the spinal cord runs at the neck).
Her symptoms resolved after having carpal tunnel release surgery.
Two more conditions that mimic carpal tunnel symptoms are cubital tunnel syndrome and ulnar tunnel syndrome.
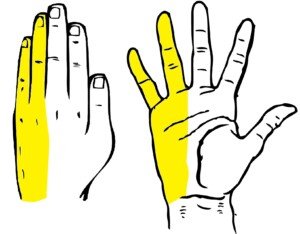
The nerve distribution for cubital and ulnar syndrome.
These cause numbness and paresthesias in the ring and pinky, says Dr. Oheb.
He also names thoracic outlet syndrome and diabetic neuropathy as differentials for CTS.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com, Yanalya
sscpywrt26
Numb Fingers and Hand from Pronator Teres Syndrome

The numbness in your fingers and hand may be caused by pronator teres syndrome.
“Whereas carpal tunnel syndrome is compression of the median nerve at the wrist, pronator syndrome is median nerve compression at the elbow, says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Symptoms similar to carpal tunnel syndrome include numbness, pain, tingling, burning in the thumb, index, middle and half of the ring finger,” continues Dr. Oheb.
Pronator Teres Syndrome vs. Carpal Tunnel
“Differences unique to pronator syndrome include aching pain localized to the forearm, lack of night symptoms (seen in CTS), worsening with repetitive prono-supination, loss of sensation to the palm of the hand (due to a branch of the median nerve that comes off before the carpal tunnel).”
Prono-supination refers to repeatedly rotating your palm back and forth 180 degrees.
“There are varying degrees of pain and paresthesias (tingling, numbness) with pronator syndrome,” says Dr. Oheb.
The pain is “localized over the proximal forearm and paresthesias distally in the thumb, index, middle and half of the ring finger.
“Usually stiffness is not a presentation of pronator syndrome. Late findings of pronator syndrome may lead to weakness in the thenar muscles of the hand which may make certain functions difficult to perform.”
What can you do?
“Resting the forearm muscles, splinting to prevent forearm prono-supination, and nonsteroidal anti-inflammatories are the mainstay of conservative treatment for pronator syndrome.

Shutterstock/Praisaeng
“This is continued for a minimum of three to six months before any surgery is considered.”
Numbness in the fingers and hand can have a variety of causes. This symptom should always be investigated if it persists. Some causes:
• Cervical spine issues – herniated disc or nerve compression in the neck
• Peripheral neuropathy – often from diabetes or vitamin deficiencies
• Poor circulation – reduced blood flow or vascular problems
An overlooked possible cause for a sensation of numbness in the fingers is underactive thyroid.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
How Bad Must Shoulder Pain Be to Take Narcotic Pain Pills?

It’s important to figure out just how bad your shoulder pain must get before it’s time to take narcotic drugs.
“For most conditions involving the shoulder I recommended a course of NSAIDs first before any consideration of stronger pain medication,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Although, I do not generally prescribe narcotics for shoulder pain, I do prescribe them for fractures. There is not a specific time period for shoulder pain that determines when to consider narcotic pain medication.”
My mother several years ago experienced a lot of shoulder pain that we suspected was originating from carpal tunnel syndrome.
Preceding this she had had knee pain from a torn meniscus and had arthroscopic surgery.
This all meant that my mother was taking daily doses of powerful prescription narcotic pain pills.
It wasn’t long before the narcotics began creating side effects. I warned my mother not to take any more pain pills.
These drugs are very potent and can cause a huge host of alarming side effects, including confusion, constipation, vomiting and stomach upset. That’s just the beginning. Narcotics can also cause depression and anxiety.
I told my mother DO NOT TAKE ANY MORE PAIN PILLS. There has got to be a way to get through pain without narcotics or other potent numbing drugs.
After all, people got by before narcotic prescription drugs were even invented. My mother agreed to this plan, which went into effect two days after her carpal tunnel syndrome surgery.
Carpal tunnel syndrome surgery can leave residual pain, and my mother thought this was why her shoulder was hurting.
At one point she asked me how intense the discomfort would have to be before she could take a pill.
This was after she was seated for 30 minutes with an ice pack on her shoulder.
I explained that if she could sit through the hurt for the past 30 minutes, she could sit through it for a few more minutes, to take it a few minutes at a time, to grit her teeth and just let it run its course.
There was no way I was going to give her drugs that resulted in nasty side effects.
To help my mother cope with the hurting shoulder, I reminded her that she was fed (having had breakfast not too long before), and safe, with no danger around.
I pointed out that she was warm (I had just put a blanket on her) and not doing anything that was causing damage to her shoulder.
“The pain will not injure you,” I said.
The development of side effects coincided with when she began taking Norco, a potent narcotic, of which depression is a possible side effect.
The various narcotics my mother had taken never seemed to stamp out the discomfort anyways.
My mother sat through the discomfort until I got her up to do some shoulder exercises to relieve the pain naturally. She got through it, without taking a narcotic pill. Yes, it can be done.
Consider that pain from post-surgical carpal tunnel syndrome can be managed naturally.
Update: The shoulder pain persisted and seemed to get worse. An MRI revealed tears in the rotator cuff region.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Image Point Fr
Source: webmd.com/pain-management/guide/narcotic-pain-medications?page=2#2
Scabs on Scalp: Causes Other than Cancer

Here’s a list of benign, non-cancer causes of scab-like growths on the scalp.
“Scabs on your scalp could be caused by a wide variety of different ailments,” says Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience.
She explains, “Contact dermatitis is an allergic reaction to something you’ve touched, like shampoo, hair dye or jewelry.
“It causes dry patches that can itch or burn. If you scratch them, they may bleed and scab.
“Seborrheic dermatitis (a.k.a. dandruff) can be itchy, flaky and scabby. A dandruff shampoo should be able to help.
“Psoriasis can cause silver-gray scabs all over the scalp. A medicated shampoo may help, but severe cases should be seen by a dermatologist because more extensive treatment may be necessary.
“Lichen planus (or lichen planopilaris, as it’s called on the scalp) usually affects middle-aged people.
“It causes red or purple bumps that can be treated with topical, oral or injectable steroids.
“Ringworm is an itchy fungal infection that causes scaly patches. It is highly contagious and usually is seen in children.
“Lice can also cause scalp scabs if you scratch too much.
“Shingles (a resurgence of the chickenpox) causes small blisters that turn yellow and crust for up to two weeks. It may cause headaches or facial weakness for months.
“Eosinophilic folliculitis causes itchy sores that are filled with pus. It tends to affect people who have HIV/AIDS.”
So as you can see, there are many causes of scabs on the scalp other than cancer.
But this doesn’t mean you don’t have skin cancer.
You may even have one of the benign conditions above along with skin cancer, by coincidence.
This is why if you’ve been diagnosed with a benign condition, you should still get cancer ruled out, because the “scabs” of cancer can resemble the “scabs” of a benign condition.
In another article, Dr. Prystowsky explains skin cancer on the scalp.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Point Fr
Eyebrow Bald Spots: Causes & Solutions

“Hair thinning, bald patches and total hair loss in your eyebrows can be reversible in some circumstances,” explains Dr. Janet Prystowsky, who’s a board certified dermatologist in New York, NY, with 30+ years’ experience.
She continues, “However, it is important to get to the root of the hair loss problem in order to restore hair to the eyebrow.”
Causes of Bald Spots in the Eyebrows
“Potential causes may be over-tweezing, chemotherapy or radiation treatments, hypothyroidism, a skin infection or trichotillomania (compulsively pulling out hair),” says Dr. Prystowsky.
A person may be unaware of how much she is finger-plucking away at her eyebrows when, for instance, entrenched in computer work or a gripping movie.
“It may take weeks or months for hair to grow back once the underlying cause is determined.
“If hair does not grow back, an off-FDA label use of a hair-stimulating product like Latisse (available only by prescription) or minoxidil (over the counter as Rogaine) may help.
“Check with your dermatologist to make sure you are a good candidate.
“Others may prefer using makeup pencils and powders to fill in their eyebrows. Tattoos are also a great option when they are done well.”
Another option, which is more common than you think, is eyebrow transplantation. Ask your dermatologist about this.
What about postmenopausal hormone changes?
Yes, the changing hormonal environment of a woman’s body in the years after menopause can definitely thin out the eyebrows — to even a very noticeable degree.
The thinning, though, would much more likely be uniform or diffuse rather than in just specific areas causing that bald spot appearance.
And of course, these hormonal shifts wouldn’t be the cause in premenopausal women.
Minoxidil
A less pricier version of the drug minoxidil is available at Walmart, and the brand is Equate.
This drug could be used off-label to reverse bald patches in the eyebrows only when other methods have failed to restore the hair.
You must be extremely careful when applying it because if it gets in the eye, the stinging is very painful.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, bearfotos
New Dark Hairs on Breast? Can Mean Weight Gain Disease

The appearance of new dark hairs on your breasts probably mean nothing, but you should see your doctor just to be sure, especially if you have additional new symptoms.
“New dark hairs on breasts should not be an immediate cause for concern,” says Tejas Patel, MD, a board certified dermatologist with Reforma Dermatology in NYC.
Many women do have dark hairs on their breasts.
These pop up usually during times of normal hormonal changes such as during puberty, pregnancy or menopause.
It’s generally a harmless finding by a woman.
Concerning Cause of New Dark Breast Hairs
“These dark hairs could be due to a plethora of reasons, most likely caused by hormonal changes,” says Dr. Patel.
“You should visit your local dermatologist if you notice any other accompanying symptoms, as it might be of importance.
“Examples of accompanying symptoms would include acne, uncontrolled weight gain, excess hair growth, menstrual irregularities and others.”
The condition that causes these symptoms is PCOS: polycystic ovarian syndrome.
Many women with PCOS are mostly concerned about the weight gain aspect.
However, with proper exercise habits and a clean, controlled diet, a healthy body weight can be maintained.
Regular physical activity, including both cardio and strength training, helps regulate insulin levels and support metabolism.
Adding lean muscle to one’s body will raise the resting metabolic rate.
A diet rich in whole foods — low in refined sugars and high in fiber — can reduce inflammation, improve hormone balance , and aid in weight management.
Consistency in these habits can significantly reduce the symptoms of PCOS and promote overall well-being.
PCOS Without Weight Gain Is Still Concerning
But even if you don’t gain much weight, PCOS is certainly nothing to sweep under the rug, either.
That’s because complications can include miscarriage, infertility, type 2 diabetes and abnormal uterine bleeding.
Women with new-onset dark hairs on their breasts should not panic, but should also see a doctor to rule out any concerning cause and hopefully rule in the body’s normal hormonal fluctuations.
 Dr. Patel treats all skin types and welcomes the most challenging skin problems. Dr. Patel specializes in both medical and cosmetic dermatology, and treats patients of all ages.
Dr. Patel treats all skin types and welcomes the most challenging skin problems. Dr. Patel specializes in both medical and cosmetic dermatology, and treats patients of all ages.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Max4e Photo
Black Hairs Growing on Breast: Causes

“If dark hairs suddenly appear on your breast,” begins Dr. Janet Prystowsky, a board certified dermatologist in New York, NY, with over 25 years of experience, “hormones are most likely the culprit.”
When women notice a black hair or two sprouting on their breasts, they want to know what could be the cause of this.
Dr. Prystowsky continues, “Many women experience dark hairs on their breasts, usually during periods of hormonal change like puberty, pregnancy or menopause.
“Generally this growth of dark hair (known as hirsutism) is harmless.
“However, there are some reasons to be concerned. Polycystic ovarian syndrome (PCOS) can cause unwanted hair growth, as it changes your hormonal balance.
“If you have PCOS or another hormone condition, you may also develop acne, problems with menstrual periods, trouble losing weight and diabetes.
“A tumor that releases male hormones could also cause these symptoms.”
“Check with your doctor to make sure that your black hairs are just part of your body’s normal hormonal fluctuations and not attributable to PCOS or another hormonally unbalancing condition.”
Here are the red flags for a tumor related cause:
Rapid onset of new hair growth, especially in adulthood.
Other virilizing signs: deepening of the voice, male pattern baldness, clitoral enlargement.
Irregular or absent menstruation
Abdominal pain

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.