Do you know the first three things you should do if someone’s having a stroke?
Even a middle aged person can be stricken by this very common condition. Time is truly of the essence when it comes to a stroke.
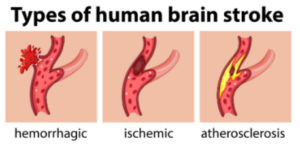
The most common type of stroke is the ischemic type, in which a blood clot in the brain cuts off blood flow – and therefore oxygen – to the area of the brain that the blood vessel feeds.
The less common type is the hemorrhagic, in which a blood vessel ruptures, spilling blood onto brain tissue.
Both are life-threatening situations, and anyone nearby needs to act super-fast.
Time Is Brain
For some, time is money. But for all who have a stroke, time is brain. Fast thinking and fast action are crucial to prevent death and brain damage.
First Three Things to Do when Someone Is Having a Stroke
“The main thing is to immediately contact 9-1-1 and get the patient to the hospital,” says Sendhil Krishnan, MD, a board-certified adult general cardiologist with advanced subspecialty training in interventional cardiology.
“In the interim one should continue to monitor their neurological response and continuously check for a pulse (start CPR if necessary.)”
So that’s 1) call 9-1-1, 2) observe the patient, and 3) continuously check for a pulse.
“Patients should not be given any medications including aspirin,” says Dr. Krishnan.
“The reason for this is the stroke may be due to a bleed (hemorrhagic) or ischemic (due to clot). Giving blood thinners may only worsen the bleed and their brain.”
Source: vecteezy.com
Speaking of blood thinners worsening a bleed – another condition can mimic a stroke for which blood thinners can make worse: a delayed subdural hematoma from recent head trauma that the patient may have forgotten about, such as hitting their head on the door frame of a car when getting out.
This seemingly minor head trauma can cause a delayed brain bleed in a person over 65. The symptoms are nearly identical to that of an ischemic stroke.
Recognizing an Ischemic Stroke
Symptoms are sudden-onset.
• Any trouble with vision
• Paralysis of one side of the face or body/limb
• One side of the face drooping
• Weakness on one side of the body
• Slurred speech or difficulty talking
• Confusion or altered mental status
• Not being able to communicate even though seemingly conscious
• Stroke is even more suspicious if more than one of these symptoms are occurring or if there’s an accompanying bad headache.

Age is a risk factor, but In 2009, 34% of people hospitalized for stroke were younger than 65. Source: cdc.gov/stroke/facts.htm. Freepik.com

“FAST” is the easy-to-remember acronym for stroke.
Signs of a Hemorrhagic Stroke
• Sudden “thunderclap” headache that takes a person’s breath away
• Patient reports they’ve never had a headache so agonizing.
• Nausea, vomiting may precede the headache.
• Vision problems
• One pupil more dilated than the other
“If the patient is diabetic and is profoundly hypoglycemic, they may act and behave as if having a stroke,” says Dr. Krishnan.
“In this case I would recommend giving them something sweet or sugary to raise their blood glucose levels.
“I would recommend things that can be absorbed through their cheeks (i.e., a lollipop or sugar tabs).”
This way the patient won’t have to chew and swallow, which – if they are having a stroke – could lead to choking and aspiration, says Dr. Krishnan.
Diabetes is a risk factor for stroke, so just because a person is diabetic doesn’t mean that you should automatically assume that the sudden-onset symptoms are from low blood sugar.
Even an ER doctor can’t officially confirm diagnosis of a stroke without a brain scan. Thus, the layperson family member or friend absolutely should not try to diagnose the absence of a stroke just because the patient has had similar symptoms in the past from diabetes or is “too young to have a stroke.”
Ischemic and Hemorrhagic Stroke Risk Factors
• Age 65+
• Atrial fibrillation
• Carotid artery disease or peripheral artery disease
• Chronic/congestive heart failure
• Coronary artery disease
• Diabetes
• Diet high in sodium or bad fats (saturated, trans)
• Family history of stroke or cerebral aneurysm
• High blood pressure
• High cholesterol
• Obesity
• Previous diagnosis of a cerebral (brain) aneurysm
• Previous heart attack
• Previous transient ischemic attack (TIA)
• Sedentary lifestyle
• Smoking
Time lost is brain lost when it comes to a stroke. Seconds, not minutes, count.
 Dr. Krishnan is with Pacific Heart & Vascular, where you can view his videos on heart disease and healthy living. He has numerous publications and often speaks at local and regional events.
Dr. Krishnan is with Pacific Heart & Vascular, where you can view his videos on heart disease and healthy living. He has numerous publications and often speaks at local and regional events.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.



























