What to Expect the Day AFTER Knee Replacement Surgery

The day OF total knee replacement surgery — after the surgery, that is — is not always the same as the day AFTER total knee replacement surgery.
Are you worried about a loved-one who just had total knee replacement surgery, who seemed to be doing well and in high spirits several hours after the surgery, but then next day, seemingly has taken a turn for the worse?
Relax. This is normal. I know so because my father just had total knee replacement surgery.
The surgery for his knee replacement was in the late morning, and in the evening, I visited him.
He was in high spirits, feeling no pain (due to a “nerve pain block” that was still in effect), and his knee had what appeared to be several pounds of bandages wrapped around it, above it and below it.
Emotionally, he was doing great; total knee replacement surgery is very traumatic to the lower body, even though advertisements for total knee replacement surgery make the ordeal seem like smooth sailing.
The next day, I saw a completely different man. He complained of burning skin and a burning forehead, yet a chilled lower body; grueling pain in the knee despite having been medicated all day long with painkillers, and was depressed, downtrodden, dismal, and kept complaining that there had been no progress with the rehab.
His startling words were, “I have a gut feeling something is wrong.” He said he felt that the knee just wasn’t working at all during the rehab.
The morning after total knee replacement surgery, a patient is started on rehab.
In the surgery, the knee is literally replaced; the patella bone is removed and a titanium plate is put in, and in between the knee are metal parts that substitute for the cartilage that was originally there.
Despite such extensive surgery, the patient is given rehab the following morning.
He or she is held by rehab staff while trying to walk using a walker. Additionally, rehab involves various exercises.
My father kept saying how poor he had performed, and kept comparing this outcome to the morning and day following his first total knee replacement.
A nurse took his temperature to check for fever; his forehead was hot; he felt burning up; also felt chilled; but wanted the room cooler.
His temperature was normal. My father’s dampened spirits were spooky; I’d never seen him like this before.
This wasn’t just about knee pain.
There was the odd burning sensation in his skin and face; he appeared flushed; there were the chills in the lower body; and overall he just felt terrible, hopeless and was convinced that somewhere along the way, there was a mistake made.
He even entertained the idea that the nerve pain block damaged the nerve in his upper leg.
The nurse kept assuring him that the rehab went “perfect” and that he was ahead of schedule.
The nurse showed no worry and kept smiling, insisting that my father would feel “200 percent better” the next morning.
She was not able to say if any of the medications were causing side effects, and despite continually reassuring him and his family, he was convinced he was doomed, and just lie there, projecting hopelessness and having given up.
Next day, two days out from the total knee replacement surgery, there was a complete turnaround.
He’d been given a different painkiller which was working — no pain — and not only that, but the rehab went great; he was in very high spirits. A complete turnaround.
So if your loved-one seems out of character with abnormal dejection and feelings of hopelessness the day after total knee replacement surgery, you must realize that the next day, he or she will likely feel just fine and ready to take on the world.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, peoplecreations
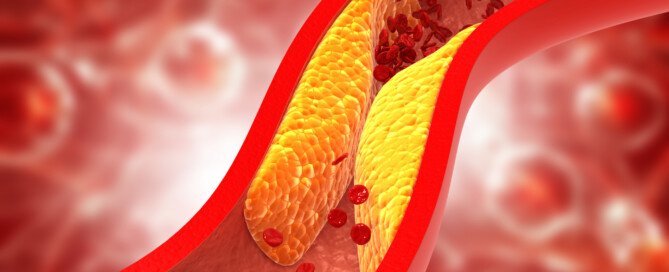
Can Two Supplements Reverse Plaque in Coronary Arteries?
Can these two supplements actually reverse buildup of plaque in coronary arteries (heart disease)?
Yes — according to a very interesting study. But there are things you need to consider about the study.
“This study was performed in 2012 by researchers associated with Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center,” says Carlos González Quesada, MD, FACC, attending cardiologist with Cedars-Sinai Medical Center and a cardiologist with Cardiovascular Medical Group of Southern California.
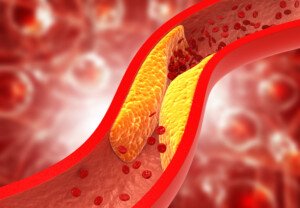
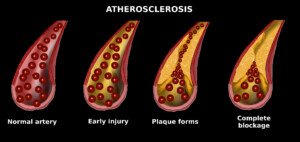
There is controversy over whether or not natural supplements can reverse coronary plaque buildup (a disease called atherosclerosis), which is strongly correlated to heart attack risk.
So the researchers studied a group of people (65 total at the start) who, when compared to the general population, have a two- to four-fold greater risk of heart attack.
This group was firefighters, and for the study, they took daily supplements of coenzyme Q10 (coQ10) and aged garlic extract (AGE).
Another group of firefighters did not take these supplements, so that a comparison could be made.
Nobody in the study was on statins. At the beginning of the study, all subjects had their calcium score taken (a numerical value of measurable plaque buildup).
The supplement group took 120 mg and 1,200 mg a day of coQ10 and AGE, respectively.
The control group took a sugar pill, but nobody knew which group they were in, and neither did the researchers.
The calcium scores of both groups, at the beginning, did not differ that much.
At the end of one year (during which the supplement group took their daily doses), another calcium score test was given.
The supplement group had about half the rate of coronary arterial plaque progression as did the placebo group, and this includes an adjustment for typical risk factors for plaque buildup.
What is the takeaway?
“Over the course of 12 months, 15 patients dropped the study due to loss to follow-up, withdrawal of the consent, or meeting exclusion criteria,” says Dr. Quesada.
“This is a significant number of patients who were not followed-up and may have impacted the result of the study.
“Although there was a small difference in the coronary calcium score and other markers of inflammation, this does not mean that there is a clinical difference.
“In other words, this does not prove that patients on the experimental group are less likely to develop heart attacks, strokes or develop premature death.
“Furthermore, the patients were only followed for 12 months, which is a short period of time.
“Results may have been different if the patient had been followed by several years.
“In my opinion, this clinical trial does not demonstrate a clinically relevant benefit of treating patients with a combination of coenzyme Q and aged garlic extract.
“To demonstrate any benefit, a larger clinical trial with longer follow-up is needed.”
In the meantime, here are very proven ways to prevent dangerous plaque buildup and possibly reduce soft plaque buildup on coronary arteries.
Shutterstock/Cessna152
Exercise. This means sustained aerobic activity at least three times a week for at least 20 minutes — something that gets your heart rate and respiration elevated: brisk walking, hiking, jogging, pedaling, stepping or a fitness class.
Avoid trans fats. This ingredient in processed foods also goes by the names shortening and partially hydrogenated vegetable oil.
Limit processed foods. Eat five to seven servings a day of any combination of fruits and raw vegetables.
If you’re overweight, lose weight. Practice portion control and stick to an exercise regimen.
 Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/ Explode
Source: ncbi.nlm.nih.gov/pmc/articles/PMC3425023/
How Long It Takes Good Diet to Lower Bad Cholesterol
Do you think you’re too old to improve your diet for your cholesterol because it’ll take too long to kick in? Guess what: you’re wrong.
“Any blood work that is obtained on an individual can be viewed as a snapshot in time,” says Richard Kelley, MD, a practicing physician in Texas for 20+ years, and author of “The Fitness Response,” “The Three-Hour Appetite” and the ebook, “The Fitness Response ‘Diet’ for Women.”
He continues, “Consequently, specific lab values, regardless of what they are, can often vary from hour to hour and day to day.
“Though lipid and cholesterol testing is usually done at intervals of several weeks between panels, depending on what a given practitioner is interested in looking at, I have had the opportunity on many occasions to observe repeated studies of LDL and other components of the lipid panel, within days of a patient changing to a cleaner form of diet, and have been able to observe improvement in LDL within a matter of days.”
LDL, the “bad cholesterol,” stands for low density lipoprotein, and you don’t want this number getting above 150.
It’s possible to have a very low triglyceride number (the lower, the better) at the same time that the LDL is on the high side.
Don’t underestimate the power of a better diet in lowering bad cholesterol, regardless of your age.
Dr. Kelley continues, “We know, without a doubt, that in patients who have no predisposition to elevated triglyceride or LDL cholesterol, these values can be elevated or show improvement, sometimes within a matter of two to three days, to varying degree, with simple changes which improve one’s diet.”
As one loses weight from an improved diet, it’s not surprising for medical professionals to observe marked improvements in cholesterol and lipid values, even normalization of these values, adds Dr. Kelley.
If you’re worried about an LDL value that’s increased or is already over 150, the best diet to lower bad cholesterol is one that severely restricts processed foods.
Avoiding buying food in the center of the supermarket right off the bat will go a long way at lowering bad cholesterol; foods that are in the centers of grocery stores tend to be the most processed (with the exception of the bakery department which is typically in the perimeter).
To lower LDL bad cholesterol through diet, avoid the store’s bakery department, increase consumption of raw vegetables, eat more fruit, eliminate beef from grain fed sources (eat only wild game or grass fed beef), eat salmon/tuna/scallops/halibut several times a week, eliminate fast food products, and eat nuts and seeds.
 Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
Richard Kelley, MD, is an author, speaker, fitness expert and transformation coach.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Green Vomit Mean Cancer?
Do you fear that the green in your vomit means cancer?
Perhaps you’ve upchucked lately and couldn’t help notice that the color of your vomit was actually green. Now that can sure be unsettling.
However, this green in your vomit doesn’t mean that anything is seriously wrong with you such as cancer.
In fact, a truly serious sign is when you see red in your vomit — from blood.
But GREEN?
Don’t fret; it’s nothing to worry about. I myself have never seen green in my own throw-up, but I understand that this can frighten people who do happen to notice this odd color.
Gastroenterology is the medical specialty that deals with the gastrointestinal tract (intestines and stomach organ).
“Green color in vomit can occur either because of green food, or more commonly from vomiting bile from the intestine which has a yellow/green appearance,” says Edward Cruz Paredez, MD, a board certified gastroenterologist based in La Jolla, CA.
No cancer.
If you’ve noticed that your vomit is green, ask yourself if you’ve recently eaten broccoli, cucumbers, kale, spinach or other such produce.

Dr. Paredez continues, “Yellow/green bile is made in the liver out of bile salts and pigments/colors.
“These salts aid in digestion and are secreted into the intestine just past the stomach to mix with food contents from the stomach.
“Vomiting green bile can occur in a number of instances and is not specific for ‘how sick’ someone is or what the cause of vomiting is.
“Most people aren’t accustomed at seeing their own vomit and panic when they see the green color, even if they know it is from bile.”
So when you see this hue in the content that you just upchucked, it’s actually the bile that comes from the liver.
“Vomiting green bile often alarms people since they may not have eaten anything green and they do not realize that the body makes bile continuously for us to digest our food,” says Dr. Paredez.
As mentioned before, blood in the vomit warrants a trip to the doctor for evaluation.
However, blood can also manifest as brown, appearing like coffee grounds.
When you throw up, don’t be afraid to take a good look at its contents or color.
If throwing up is accompanied by any other symptoms, see your physician.
So you now know that green vomitus is not a sign of cancer.
However, you should investigate why you’re puking in the first place.

Dr. Paredez has been named a Top Doctor by San Diego Magazine and has also received a 2016 “People Love Us on Yelp” Award.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
What It Costs to Treat Dog Injuries from Exercise

The cost of treating a dog’s injuries–the kind from exercise — is not the least bit cheap.
It’s advised that you have a “dog injury fund” in a second bank account!
When it comes to how much it costs to treat dog injuries, it depends on several factors, says Dr. Jules Benson, BVSc, chief veterinary officer with NationwideDVM, a pet insurer company.
- what diagnostics and treatment your veterinarian considers appropriate for the circumstance
- whether there is any follow-up care, pre- or post-operative rehabilitation or complications
- how large your dog is (larger dogs can cost considerably more for medications and surgical procedures)
- and where you live – veterinary prices vary depending on state/area, and some procedures may only be available if you have a specialty veterinarian in your local area.”
Pet Insurance
Dr. Benson points out that a pet insurance plan will reimburse a percentage of the veterinay bill, “minus a deductible – both of which are selected by the policyholder.”
The costs below reflect an average reimbursement for these conditions as of 2012.
Injuries in Dogs–How Much They Cost
Lameness: $478.80
Cruciate ligament tears: $2,107.31
Luxating patella: $1,262.61
Broken nail: $220.52
Lacerations/cuts: $314.99
Heat stroke: $1,168.43
When your dog is getting exercise, it can be difficult to prevent injuries.
Your dog can be bounding out in a field and step on something that sprains its leg or deeply cuts into a paw. It’s something that just might happen no matter how careful you are.

However, one of the injuries on that list can be prevented: heat stroke.
Unless you and your dog are unexpectedly stranded in a desert, there is no reason for a dog to develop heat stroke.
For any physical activity on a hot day, bring plenty of water, and give it to your dog frequently throughout the activity, especially if it’s strenuous like a hike.
In the event that your dog sustains any of these injuries or some other injury via exercise (or some other origin), you should put aside some money every month for a treatment fund.
Even if it’s just $20, this will cover a broken nail in two years.
 Dr. Benson is regularly consulted by many media outlets including ABC, NBC, FOX, The Wall Street Journal and The New York Times to provide pet health advice to pet parents nationwide.
Dr. Benson is regularly consulted by many media outlets including ABC, NBC, FOX, The Wall Street Journal and The New York Times to provide pet health advice to pet parents nationwide.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Local vs. General Anesthesia for Knee Arthroscopy

Which is better for knee arthroscopy: local anesthesia or general?
We all know that general anesthesia comes with far more risks than local, but there are circumstances that call for general anesthesia over local for a knee arthroscopy.
It’s also understandable if the idea of “going completely under” is frightening.
You probably already know that the level of unconsciousness while under general anesthesia is deep enough that the patient cannot be aroused without drugs.
It’s so deep, in fact, that the patient can’t even breathe on their own; they must be intubated: A tube is placed down their throat and breathes for them.
Local vs. General for Knee Arthroscopy
“Local anesthesia is a reasonable consideration assuming the planned procedure is not expected to be extensive or to last longer than 20 to 30 minutes and does not require the use of a tourniquet,” explains Dr. Mark Galland, orthopedic surgeon, sports medicine specialist and physician at Orthopaedic Specialists of North Carolina.
“The tourniquet itself may cause pain that will not be adequately addressed by the use of a local anesthetic.”
Knee Arthroscopy
This very common procedure allows the doctor to view a knee joint despite making only a small incision.
Arthroscopy allows the surgeon to diagnose the specific condition and then treat it.
Viewing is done via a little camera (arthroscope) that’s inserted into the joint.
It shows images on a video monitor that guide the surgeon in using thin, miniature surgical instruments – that allow for very small incisions.
The patient enjoys a much faster and less painful recovery than what would occur with invasive surgery to the knee, especially if it were done with general anesthesia.
Be sure to ask your surgeon adequate questions to make sure you understand the precise nature of your condition and why your surgeon — if this is the case — has opted for general anesthesia over local to perform your knee arthroscopy.
Dr. Galland has authored many book chapters and papers in sports medicine. His advice and consultation have been sought by world-class athletes in track and field and Major League Baseball.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Africa Studio
Stomach Burning from Exercise Caused by Magnesium Deficiency
Have you experienced a burning sensation in your stomach during or right after exercise?
What can cause a burning feeling in your abdomen when you exercise?
“Sit-ups can aggravate a hiatus hernia and lead to reflux or even vomiting,” says Carolyn Dean, MD, ND – Medical Advisory Board Member of the non-profit Nutritional Magnesium Association at nutritionalmagnesium.org.
Acid reflux can cause a burning or aching feeling in the stomach.
Reflux is when acid in the stomach enters into the esophagus (“food pipe”).
However, the discomfort of reflux can still occur in the stomach, not necessarily only in the chest.
“Also, stomach spasms and vomiting can be aggravated by magnesium deficiency…since magnesium makes muscles work properly, allowing calcium to cause muscle contraction and then pushing calcium out of the muscle cells to allow the relaxation phase,” explains Dr. Dean.
“When there is a lack of magnesium, muscle cells in the bronchial tubes can go into spasm, tighten up and cause wheezing and burning and coughing.”

Dr. Dean, in practice for 35+ years and author of “The Magnesium Miracle,” is also a naturopath, nutritionist, herbalist, acupuncturist, lecturer and consultant.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/KDdesignphoto
Pancake Breakfast or Skipping Breakfast: Which Is Healthier?
Mmmm, a stack of steaming pancakes drenched in maple syrup and butter for breakfast: Is this healthier than SKIPPING breakfast?
Plenty of research shows that a nutritious morning meal is the most important meal of the day (or maybe the second-most important, if you rank the post-workout meal in the top spot for later-day workouts).
The Research on Breakfast for Kids
- Eating it is linked to lower risk of type 2 diabetes in children (Donin et al).
- Eating it is linked to higher IQ’s in kids (Liu et al).
- Skipping breakfast increases kids’ obesity and cardio-metabolic risk (Eloranta).
- Skipping is associated with reduced learning and reduced attention span in kids (Bennett et al).
And what about adults?
- Fuster et al found that skipping breakfast is associated with hardening of the arteries.
- It can lead to poor food choices for the rest of the day (Auestad et al).
- It may lead to high blood pressure and coronary artery disease (Cahill et al).
Note that some of these negative outcomes are associations rather than direct results.
We can venture to say that people who always pass on breakfast are less likely to be health conscious or put in grueling gym workouts.
Therefore, due to poor overall diet and lack of exercise, they’re more likely to develop type 2 diabetes or cardiovascular disease.
But the direct results, such as poor concentration, can’t be dismissed.
If the only breakfast available were pancakes, would it be better for your body to eat all this white flour, sugar and butter fat than to skip it?
“As a clinician, I am always one to promote eating something for breakfast,” says Amanda A. Kostro Miller, RD, LDN, whose specialties are nutrition counseling, weight loss and medical nutrition therapy.
“When we skip breakfast, we may get really hungry by lunch and overeat at lunch.
“While a pancake breakfast is not the best choice, there are small changes we can make to improve upon the nutritional profile of a pancake breakfast.
“Here are some ways to make a pancake breakfast better:
- Add fruit and/or nuts.
- Make your pancakes whole grain.
- Minimize the syrup.
- Control the amount of butter used.
- Instead of large pancakes, make yourself small/mini pancakes (control the number).
“Many people who don’t eat breakfast tend to have several obstacles that prevent them from actually eating breakfast (e.g., lack of time, don’t know what to make, want to sleep in, not hungry in the morning).
“However, if a client is already eating a breakfast (even pancakes), we can work on small changes to their breakfast to make it healthier.
“As a clinician, these small changes, rather than getting someone to prioritize their time to eat breakfast, can be easier.”
Certainly, a breakfast laden with white flour and sugar will satisfy hunger and prevent overeating at lunchtime.
Then again, if a pancake breakfast isn’t consumed with discrimination, it can have far more calories than overeating at lunch after a skipped breakfast.
A well-managed breakfast of pancakes should stave off poor concentration and reduced learning or impaired productivity in children at school and adults at work, respectively.
But remember, as much as the body wants and needs fuel shortly after it awakens from an overnight fast, if you put junk in your body, it will still be junk. Junk food is junk food.
Don’t give up pancakes if you love them. But make an effort to limit intake and make most of your breakfasts healthier options such as eggs with fruit and yogurt, or a fruit smoothie with a whole grain English muffin topped with a little butter.
 Amanda Kostro Miller has worked with U.S. veterans, people with eating disorders and those with various acute and chronic diseases.
Amanda Kostro Miller has worked with U.S. veterans, people with eating disorders and those with various acute and chronic diseases.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Surgical Hair Restoration: Can You Run Out of Donor Sites?

Ever see those surgical hair restoration infomercials and wonder if the donor follicles can keep up with the hair loss follicles?
In surgical hair restoration, follicles that are not genetically programmed to eventually stop producing are “grafted” onto the sites that have become bald.
If you’ve seen any hair loss infomercials involving surgical solutions, perhaps you’ve wondered what I’ve wondered.
In male pattern baldness, the first areas to “go bald” are the top and top/back of the head.
When this pattern of baldness progresses enough, the man is left with a horseshoe pattern of hair.
In extreme cases, this remaining hair is a thin band encircling the lower portion of his head, just above his ears, revealing significant amount of scalp.
The infomercials show the donor site as the section of hair that’s below the balding area. But won’t this area eventually thin out too?
As follicles from this area are grafted onto the top portion of the patient’s head, seems that if this is done enough, this donor area will thin out.
And because this donor area will thin out if it’s harvested enough, and as the male pattern baldness progresses over many years, won’t the patient be left with hair pretty much only on the top of his head?
“Realistic short and long term results should be discussed, as the balding process is progressive and final results can be unpredictable,” says Allen Gabriel, MD, board certified plastic surgeon with PeaceHealth Medical Group Plastic Surgery in Vancouver, WA.
“Over time the transplanted area may become ‘isolated’ and therefore multiple procedures may be necessary over one’s lifetime to achieve natural results.”
Dr. Gabriel continues that “small areas of donor sites can be taken for hair transplant without any loss of noticeable hair with newer techniques.”
The back of the head is a common donor site (since male pattern baldness begins more towards the top of the head).
Taking follicles from this site will not result in noticeable hair loss, says Dr. Gabriel.
“Even if a larger graft is taken and divided into mini-grafts (not the preferred way), the skin and scalp can stretch and expand, and loss of hair will not be noticed as long as the hair is long enough to cover (or drape over) the donor scar.
“With newer techniques and technologies (i.e., follicular unit extraction), the surgeon can retrieve grafts three to five times from the same area,” explains Dr. Gabriel.
“It’s like harvesting blades of grass from the lawn. If we disperse the harvesting, it will not be noticeable.”
Will grafts grow if they are transplanted in an area that never grew hair?
For instance, suppose a person always had a receding hairline, or, to put it another way, prominent temples with an innately, naturally receding hairline.
If the skin here is healthy (non-scarred and no prior history of radiation), and especially if the patient is a nonsmoker, then this recipient site will be “welcoming to the graft,” says Dr. Gabriel.
He emphasizes that medical problems such as diabetes, vascular and thyroid disease will interfere with results and should be controlled prior to the procedure. Smoking cessation is also critical for better results.
“One can graft near the temple or graft on the forehead to lower the hairline, even though hair never grew there.”
 Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
Dr. Gabriel is adept at addressing a wide range of concerns, from breast reconstruction after mastectomy and the treatment of congenital anomalies, to complex facial and breast surgeries performed solely for cosmetic improvement.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/wavebreakmedia
How Many CT Scans Should a Head Trauma Patient Have?
Just how many CT scans are needed if someone has a small brain bleed resulting from a not-so-severe head trauma?
This can be banging their head on the bottom of the bathroom sink after kneeling on the floor and getting up.
Is it possible for a doctor to over-order CT scans in a head trauma patient with a chronic subdural hematoma (slow brain bleed)?
Years ago my mother had seven CT scans in 29 days due to a chronic subdural hematoma.
Certainly, she is not the only person to ever undergo many CT scans of the head in a short period of time.
Concerns of Radiation Exposure of Multiple CT Head Scans over a Short Time Period
What About for Milder Head Trauma?
The January 2013 issue of Neurosurgery has a report that questions the need for repeated CT scans in patients with non-severe brain bleeds.
“The available evidence indicates that it is unnecessary to schedule a repeat CT scan after mild head injury when patients are unchanged or improving neurologically,” says the paper.
In the case of my elderly mother, the diagnosis was chronic subdural hematoma (nowhere near as severe as acute subdural hematoma).
• On 11/28/10 my mother had a CT scan after hitting her head.
• Next day she had another one. Both were normal.
• However, 42 days later (01/09/11) she had another CT scan after awakening with neurological symptoms. That image showed the brain bleed.
• Two days later she had another CT scan following surgical draining of the blood/fluid from her brain.
• About a week later she had another one because she was experiencing new-onset neurological symptoms — that were ultimately attributed to an anti-seizure drug given pre-emptively for the head injury.
On 01/24/11 she had another computerized tomography (scheduled), but this one was based on yet a new set of neurological symptoms (that were soon found to be caused by a recurrence of the brain bleed).
The next day she had yet another CT scan (in the ER) following acute delirium. The ER doctor said the delirium was an adverse reaction to the Medrol Pak (oral steroids) that were prescribed for the injury.
On 01/27/11 she had another imaging following her second surgical draining.
That all seems like a lot of head CT scans, but it’s important to keep ahead of brain bleeds, and to weigh the risk vs. benefits.
It would take many years for radiation exposure to cause adverse effects, if any, and if the patient is already elderly , the concern over radiation becomes smaller.
The standard protocol is to give repeated CT scans after even mild head trauma, since bleeding in the brain can be life threatening or cause permanent neurological damage.
Whether the patient truly needs routine follow-ups based on a timeline, vs. another scan based on symptoms or what the previous scan showed, is up to the treating physician.
The Neurosurgery study authors favor neurological examination as a stronger determinant in treatment changes.
Symptoms, not timelines, should guide the need for CT scans for small slow brain bleeds, says the study.
These findings do not necessarily apply to victims of severe head trauma.