A large study suggests that tailoring breast cancer screening to a woman’s individual risk can be safer and more effective than routine annual mammograms for everyone.
By matching screening frequency to personal risk, researchers were able to lower the chance of catching cancer when it was in an advanced stage rather than early, while still giving each woman the screening she needs.
The findings come from the first phase of the WISDOM study, which included 46,000 women across the U.S.
Why Age Alone Isn’t Enough
For years, screening guidelines mostly relied on age, assuming similar risk for all women.
But research shows breast cancer risk varies widely among individuals.
The personalized approach starts with a risk assessment that includes genetics, lifestyle, biology and health history.
This information helps guide better prevention strategies and screening decisions.
How the WISDOM Study Worked
The WISDOM study compared traditional annual mammograms with a strategy based on personal risk.
Researchers used validated models to sort participants into four risk groups based on age, genetics, lifestyle, health history and breast density.
Below is how dense breast tissue appears on a mammogram: a lot of “white” areas.
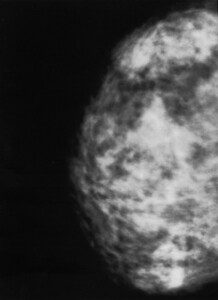
Dense breast tissue, which can obscure a tumor.
Women at lowest risk, about 26%, were advised to delay screening until age 50 or until their risk matched that of a typical 50-year-old.
Those at average risk, 62%, were recommended mammograms every two years.
Women at elevated risk, 8%, were advised to have annual mammograms.
The highest risk group, 2%, was advised to have screening twice a year, alternating between mammography and MRI.
Support for Higher Risk Women
Women in elevated or highest risk groups also got personalized guidance to reduce their breast cancer risk.
This included lifestyle advice, access to online decision tools and consultation with breast health specialists.
Some recommendations covered diet, exercise and medications that can lower risk.
Importantly, risk based screening did not lead to more late stage cancer diagnoses.
Women who chose not to be randomized could join an observational group, and most of them, 89%, still opted for risk based screening.
Expanding Genetic Testing
Since 2016, WISDOM has enrolled over 80,000 women, including those as young as 30, to catch early aggressive cancers.
An important finding was that 30% of women with genetic variants that were linked to higher breast cancer risk had no family history.
Under current guidelines, many of these women would not have been offered genetic testing.
The study also used polygenic risk scores to combine smaller DNA changes, which helped reclassify 12% to 14% of participants into more accurate risk categories.
The Future of Risk Based Screening
Researchers are continuing with the WISDOM 2.0 study to refine risk assessments and improve screening strategies.
The goal is to better identify women at high risk for aggressive cancers and provide prevention and screening tailored to their long-term health needs.










































