How much better is the survival rate of an endovascular repair of an abdominal aortic aneurysm when compared to open surgery?
An endovascular repair of an AAA isn’t as complicated when compared to the more invasive, open surgical treatment.
On the other hand, stented grafts can fail, and this procedure requires lifelong CT scans (radiation) for monitoring.
A Johns Hopkins professor has determined that the four-year survival rate between both repair procedures for abdominal aortic aneurysms is similar.
This means that elderly patients, who might have been considered too frail to undergo the invasive open repair, didn’t fare better with the endovascular version – when four-year survival rate was considered.
This is very compelling information for an elderly person who’s afraid to have the open procedure.
No Survival Rate Advantage
For patients over age 70, this study showed that the minimally invasive endovascular grafting did not result in a higher survival rate.
Study leader Julie A. Freischlag, MD, points out in the paper that it’s questionable that very old patients should have any repair to their abdominal aortic aneurysm.
The repairs did not prolong life because these elderly patients were “dying of the diseases of old age,” states the paper.
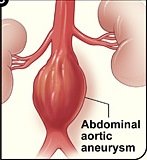
What is an abdominal aortic aneurysm?
An aneurysm is when a portion of a blood vessel wall becomes weak, causing it to swell, dilate or “balloon.”
Think of a balloon filling with air; as it enlarges, its “walls” become thinner and more prone to rupturing.
An AAA can rupture if it gets big enough, causing fatal internal bleeding. They typically cause no symptoms.
People usually learn they have an AAA when it’s accidentally discovered upon imaging for an unrelated concern.
The Johns Hopkins study concluded in 2012, which means that consideration of survival rates for open surgery vs. endovascular repair may be outdated, as advances in repair techniques are always underway.
So as of 2019, I asked Michael Fiocco, MD, about this.
“EVAR has a lower mortality rate than open surgery at 30 days — but the mortality rates converge at three to four years, due to the need for additional procedures, graft migration and potential aneurysm rupture due to migration in the EVAR group,” explains Dr. Fiocco, Chief of Open Heart Surgery at Union Memorial Hospital in Baltimore, Maryland, one of the nation’s top 50 heart hospitals.
This may make you wonder if younger patients, who in general are in better shape than those over 70, might be better candidates for open surgery.
“Younger healthier patients may be better served with open repair, but many factors are involved,” says Dr. Fiocco.
“Youth may not always convey health, and anatomy is just as important. If the aneurysm extends above the renal arteries, or down into the iliac arteries, this can be very challenging to overcome with EVAR, although techniques and equipment continue to improve.”
For endovascular repair the patient must have the appropriate anatomy to “land” the graft.
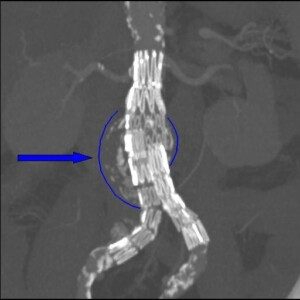
Stent graft on an abdominal aortic aneurysm. Dr Haudebourg, Public domain, via Wikimedia Commons
As mentioned previously, EVAR requires lifelong CT monitoring — every six months — to check for graft shifting (migration).
An intriguing detail in the Johns Hopkins study, which involved 881 patients with an average age of 70, is that the only post-repair aneurysm ruptures occurred in the endovascular group who did not get their regular CT scan follow-ups.