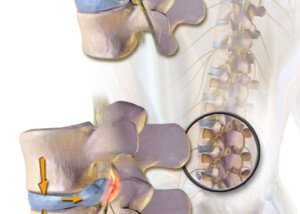
DVT and Chronic Subdural Hematoma at the Same Time?

How would a patient with both deep vein thrombosis and chronic subdural hematoma be treated?
Now, I don’t mean someone who develops a chronic subdural hematoma from the Coumadin (Warfarin) they were prescribed to treat a DVT.
Rather, I mean a new-onset deep vein thrombosis which is unrelated to the symptomatic chronic subdural hematoma.
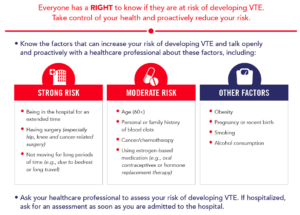
The patient has risk factors for DVT, such as smoking, lack of exercise, pregnancy or being on birth control pills, a recent joint replacement surgery and recent prolonged air travel.
The chronic subdural hematoma developed as a result of slipping on ice several weeks prior and hitting the head against concrete.
“These types of clinical situations require a close discussion between the doctors,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“This patient would likely be a good candidate for an (inferior vena cava) IVC filter. This is a small ‘umbrella’-like device which is placed in the IVC.”
The filter “does not prevent the development or propagation of DVTs, but it prevents them from traveling to the lungs and becoming a PE.”
Think of a fish net trapping fish.The IVC is a large vein that leads into the heart.
“An indication for an IVC filter is a contraindication to anticoagulation (as this patient likely would be), allergy to anticoagulation, or development of a new VTE while on therapeutic anticoagulation.”
A chronic subdural hematoma is slow bleeding in the brain, usually caused by impact to the head that creates small tears in the bridging veins near the skull.
It can take up to 12 weeks before symptoms begin appearing, due to the slow nature of the bleeding.
Anticoagulation (anti-clotting) drugs would thin out the blood, which in turn would amplify the bleeding in the brain.
My mother had a DVT and a chronic subdural hematoma — about two and a half months apart, but they could have been concurrent, simply because there had been no reason why they could not have been concurrent. She was lucky in that respect.
What about pulmonary embolism simultaneous with chronic subdural hematoma?
Simultaneous with a chronic subdural hematoma (not acute) — one that’s generating symptoms such as a “crown of thorns” headache, weakness on one side of the body and changes in cognition.
As for the course of treatment for this kind of situation, Dr. Casey explains: “Again, we would have to have a very close discussion about the best options for this patient.
“However, I think that an IVC filter may also serve this patient best.”
The IVC filter would prevent any additional PEs, but would not dissolve the PE that’s already there.
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Rocketclips, Inc.
One Calf Swollen, Hurts, Red: Possible Causes

A doctor points out many possible causes (some very serious!) of swelling, pain and redness in just one calf.
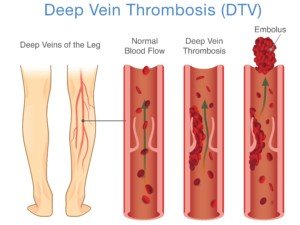
If a calf is swollen, red and painful (hurts, aches, or feels crampy), especially if there’s no explanation such as a traumatic injury or snake bite, this could mean a deep vein thrombosis (DVT).
This is actually the first thing an ER doctor will suspect if someone with these symptoms is seen in the emergency room.
An ultrasound will be ordered to check for a DVT, but there are times when a DVT is missed.
Making things even trickier is that “a large portion of patients with an acute DVT don’t present with unilateral calf swelling, pain and redness,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
Swelling, Pain and Redness in a Calf not the Only Symptoms of DVT
“Clinical manifestations are variable,” says Dr. Casey, “and range from absence of symptoms to massive pitting edema and blanching (a condition called phlegmasia cerulea dolens which is a surgical emergency with a high risk for limb loss).”
Edema is fluid buildup that causes swelling.
Pitting means that if you press on the swollen area with a fingertip or, say, eraser-tip of a pencil, it will leave an obvious indentation that will take longer than five seconds (sometimes up to a few minutes) to vanish.
However, pitting edema doesn’t necessarily mean DVT.
Other DVT Signs
“Signs and symptoms include pain, edema, erythema, tenderness, fever, a Homan’s sign (pain with passive dorsiflexion of the foot), peripheral cyanosis or prominent superficial veins,” says Dr. Casey.
Dorsiflexion is the ankle joint motion of flexing the foot upward.
“Up to 50% of patients with DVT, however, may lack any specific signs or symptoms.”
What else can swelling, pain and redness in one calf mean?
“The differential is broad and includes muscle strain or tear, Achilles tendonitis, soft tissue trauma/injury, superficial thrombophlebitis, symptomatic varicose veins, lymphedema, arthritis, stress fracture, peripheral arterial disease, renal failure, hepatic disease, heart failure,” says Dr. Casey.
You’ll likely have a memory of an extraneous insult for at least a few of these issues, such as muscle strain or tear, and stress fracture.
If you have kidney, liver or heart failure, you’ll very likely have other troubling symptoms of these conditions.
Blood tests can reveal presence of disease in these organs.
Pain, redness and swelling, especially in one calf, warrants immediate evaluation by a doctor!
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Joyseulay
TED Hose for Post-op DVT Prevention: The Truth
A surgeon presents easy-to-understand information about TED hose and post-operative DVT prevention.
My father has had, in total, four joint replacement surgeries — a big risk factor for DVT development.
In his case, the perspective on TED hose for helping prevent a deep vein thrombosis varied from surgeon to surgeon, nurse to nurse.
Gee, I wondered, is TED hose very effective or not?
Why did some medical professionals take this tool very seriously, and others weren’t too attentive to it or didn’t seem to put a lot of stock in it?
I also observed mixed perspectives on TED hose regarding my mother’s illnesses that rendered her to a lot of bed rest.
“Mechanical prophylaxis has not been studied as extensively as chemical prophylaxis in the prevention of DVT,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
Mechanical prophylaxis refers to non-pharmaceutical preventive aides for DVT. Chemical refers to medications.
“However, they may be the only treatment option for those patients in whom chemical prophylaxis is contraindicated,” says Dr. Casey.
“In addition, many of the studies combine both, rather than examine solely, the graduated compression stockings (e.g., TED hose). This may be why there is some confusion on the matter.
“Graduated compression stockings are effective in DVT prevention. The most notable recent study was a meta-analysis of seven randomized controlled trials which showed a cumulative post-operative DVT reduction, from 29% in the control group to 15% in the compression group.”
In addition to the TED hose…
“I am an equally strong advocate of intermittent pneumatic compression while my patients are in the hospital,” Dr. Casey explains.
“These have also been shown to have an extremely successful reduction in the incidence of DVTs in post-operative patients.
“Unlike stockings, they have a decreased risk of skin breakdown and irritation. Of course, they cannot be used at home.”
Warning: Make sure the nurse or nurse assistant turns back on the IPC device after accompanying the patient to the restroom or taking the patient out into the hall for some walking exercise!
More than once, I noticed that the IPC device was NOT on after my father or mother was returned to their bed!
“The DVT risk does extend beyond the post-operative period,” says Dr. Casey.
“Of course, once the patient leaves the hospital, all doctors encourage them to ambulate as much as possible, certainly at least three times per day. Ambulation is very important in the prevention of DVT.”
My father was instructed to wear the TED hose overnight for several weeks after he got home from his first knee replacement surgery.
For the third surgery, he was told he didn’t have to wear them once he got home!
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: hutterstock/Lentpjuve
How Accurate Are Doppler Scans for a DVT?
This article is about the effectiveness of Doppler scans (ultrasounds) in detecting a deep vein thrombosis.
I once read of a woman whose inner left thigh was red, swollen and painful; Doppler (ultrasound) was negative, but 11 days later a CT scan (which emits radiation) showed completely clotted veins!
Can a DVT be missed by a Doppler scan?
“ABSOLUTELY,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“I will start by saying that rarely is a test ever 100% accurate. The great aspect about ultrasound is that it is noninvasive, easily obtainable, reproducible and relatively inexpensive.
“However, the drawbacks to an ultrasound are that it is heavily technician-dependent, can be difficult in patients with a challenging body habitus (namely, obesity).
“Having said that, the sensitivity and specificity of duplex ultrasonography in the diagnosis of acute DVT is around 95% and 98%, respectively.”
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Boyloso
How Long Does It Take DVT to Form from Bed Rest?

Dr. Kevin Casey explains the time lapse for DVT to form from bed rest.
How long might it take for a deep vein thrombosis to develop as a result of excessive bed rest?
“This is a little bit difficult to answer, but I will tell you that it is not long,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“Our bodies are constantly in flux with changing hormones, cytokines and inflammatory markers.
“Under normal conditions the endothelium (vessel lining) provides a vasodilatory fibrinolytic environment.”
Vasodilatory fibrinolytic means suppression of clotting factors via dilation of blood vessels.
Dr. Casey continues, “This prevents coagulation [clotting], platelet adhesion, inflammation and clot formation.
“However, during states of disturbance of the endothelium, a cascade of prothrombotic [pro-clotting] and pro-inflammatory states occur, which can set the stage for amplification of the thrombotic process. Inflammation and thrombosis are interrelated.”
Why don’t we get blood clots in our sleep?
“Depending on the other factors simultaneously occurring in a patient (i.e., major trauma, hypercoagulable state from malignancy, etc.), a DVT can form very quickly.

James Heilman, MD, CreativeCommons
“However, an average person lying in bed for two hours will usually not encounter this problem.”
A healthy person who has not had recent surgery or who does not have other risk factors for DVT such as being a smoker who’s on birth control pills, will not develop a DVT simply from sleeping overnight, seemingly immobilized for many hours.
- The body actually moves during sleep in minute ways.
- Muscles are innervated.
- Subtle shifting occurs.
Air pressure is normal (as opposed to the cabin pressure in an airplane, which some experts believe contributes to increased DVT risk while on long flights).
Normal-length sleep is a required physiological process and thus, does not predispose one to a deep vein thrombosis.
Shutterstock/solar22
If you develop a DVT from excessive bed rest, while still in bed, can getting up and about dissolve the clot?
“Possible, yes; likely, no,” says Dr. Casey. “‘Getting up’ or ambulation doesn’t dissolve the clot. But it will begin to release enzymes which prevent the pro-inflammatory state and propagation of the clot.
“Your body may either slowly dissolve or stabilize the clot after that.”
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
DVT Risk During Long Flights vs. Long Car Rides, Movie Marathons
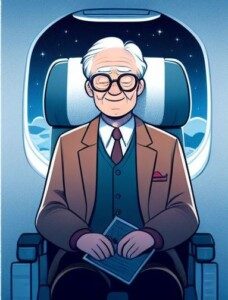
Find out if sitting for prolonged periods on an airplane is worse than sitting for extended periods in a car or on your sofa for DVT risk.
Maybe you keep hearing about how prolonged sitting during air travel is a risk factor for developing a deep vein thrombosis.
In fact, major airlines, on their planes, provide pamphlets that even explain what to do to lower the risk of developing a DVT from a long flight.
But what about sitting virtually immobile in a deep comfy chair or sofa while watching hour after hour of movies or sitcom reruns, not even getting up to use the john?
Or sitting for extended periods, legs with limited space to move, in a motor vehicle?
Developing a DVT from extended air travel is called “economy class syndrome” because the economy seats don’t allow much room for leg movement.
This is a real concern, says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“One study showed that the frequency of a PE [pulmonary embolus] was much greater in patients who traveled greater than 5,000 kms compared to those who traveled less than that,” continues Dr. Casey.
What about DVT from long car rides?
“The increased risk during air travel is probably not more than a similar population traveling in a car,” says Dr. Casey. So why isn’t there a lot of media attention to long car travel or even movie marathons at home?
“It is either less discussed and/or less studied,” Dr. Casey says. “But the same risk does apply during prolonged automobile travel and any other period of prolonged immobility.
“The World Health Organization has stated that such an association is likely to be small and mainly affects passengers with other risk factors for VTE [venous thromboembolism].”

DVT prevention exercises while on a flight or in a long car ride
In addition to prolonged immobility, DVT risks include:
Recent joint replacement, abdominal or heart surgery
Obesity
Lack of regular exercise
Dehydration
Pregnancy
Smoking
Increased age
Previous DVT
Clotting disorder
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can You Get a Blood Clot (DVT) from Lifting Weights?

A vascular surgeon answers the question of can lifting weights cause a blood clot (deep vein thrombosis).
Many bodybuilders and those who lift weights want to know if weightlifting can somehow cause a DVT.
Sometimes, it certainly must feel that way, as the athlete strains with heavy compound lifts, especially if the athlete sees their veins “popping” or “bulging” as they struggle with the load.
Another reason those who strength train or work out with weights may wonder about blood clots is because often, they strive to attain vascularity in their appearance, and this makes them think of veins.
All in all, muscle builders and other kinds of weight lifters will sometimes wonder about deep vein thrombosis, though they may not refer to it as that, and instead call it “blood clot.”
What the Doctor Says
“I suspect what this discussion is focused on is Paget-Schroetter syndrome or subclavian vein effort thrombosis,” says Kevin Casey, MD, FACS, a vascular surgeon with West Coast Vascular.
“This is an acute occlusion [blockage] of the axillo-subclavian vein [runs under the clavicle] and is classically found in an otherwise healthy young male who is an avid weightlifter.
“However, it can also be found in pitchers, volleyball players, tennis players, etc.”
What causes this?
Dr. Casey explains, “It is caused by compression of the vein by the musculoskeletal elements of the thoracic outlet.
“It accounts for approximately 1% of acute venous thromboses.
“The treatment involves chemical thrombolysis [blood thinners] of the vein followed by removal of the ipsilateral first rib and scalene muscles.”
 Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
Dr. Casey specializes in vascular and vein therapy, and has been the lead researcher on publications examining abdominal aortic aneurysms, carotid artery disease and lower extremity critical limb ischemia.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Super Morbidly Obese: Manipulating Their Enablers
Ever wonder what on earth is going on in the heads of the “caretakers” to the super morbidly obese?
These 600 to 1,000 pound men and women are confined to their bed, so it’s impossible for them to get food.
What makes a person keep bringing tons of junk food to a super morbidly obese family member who’s so huge they can’t even get out of bed?
Or if they CAN get out of bed, they’re certainly too fat to get food, let alone prepare and cook it.
So instead they somehow persuade their enabler to continue bringing them thousands of calories worth of unhealthy food by the hour.
What kind of manipulation skills can these super morbidly obese, bedridden men and women, possibly have?
What kind of power do they possess over their enablers?

Or perhaps it’s more of a situation that their enablers (spouse, significant other, parent, grown child, sibling, even non-relative friend) are just very mentally frail.
“As is the case with drug addiction, changes in the chemistry of the brain can cause people struggling with food addiction to manipulate others,” explains David Sack, MD, a psychiatrist specializing in addiction disorders, and CEO of Promises Treatment Centers in Malibu and Los Angeles.
Their drug of choice is food. And tons of it.
What’s mind-blowing is how a physically incapacitated person with little money can exert control over an able-bodied person who has a car.
“If the enabler tries to stop enabling, the food addict may use a number of strategies to elicit compliance,” says Dr. Sack.
“They may use threats, guilt and heartbreaking pleas that are extremely persuasive,” says Dr. Sack, “especially when used against someone who is codependent.”
The TLC program, “My 600 Pound Life,” never shows the super morbidly obese person exhibiting behavior that puts a stranglehold on the enabler. At least not in my opinion.
For instance, maybe some viewers found “Penny” or “James” to be intimidating. But I sure didn’t.
At the most, the 600+ pounder is shown pouting or whining, occasionally raising their voice – but nothing that would – or should – paralyze the enabler with the fear of “I better bring her three Big Macs or else I’m doomed.”
In other words, the hissy fits when food is occasionally delayed or denied amount to little more force than what a toddler can exert.
Yet the enablers eventually give in. Of course, the dynamic usually (not always) changes once the 600 pounder commits to losing weight to qualify for weight loss surgery.
• I’m sure that the more dramatic fits are edited out.
• Nevertheless, why can’t the enablers just ignore them?
• How about leaving the home when they occur?
• Or popping in ear plugs?
• There ARE options.
The enabler is not the one in control.
The enabler, on a superficial level, seems like the one in control. You’d think that anyone who wipes your fanny would have complete control over you. But it’s the bedridden individual who wears the crown.
Can the Enabler Sometimes Be the One in Control?
However, sometimes it is the enabler who IS in control, and thrives on this control – even if it comes with the daily wiping of grime out from in between huge folds of sweaty fat.
“Those who are morbidly obese are also vulnerable to being manipulated by the people around them,” says Dr. Sack, “who may have their own unconscious emotional needs,” such as relishing being so needed.
 Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
Dr. Sack is a sought-after media expert and has appeared on “Dateline NBC,” “Good Morning America,” “The Early Show,” and “The Doctors,” among many other outlets.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
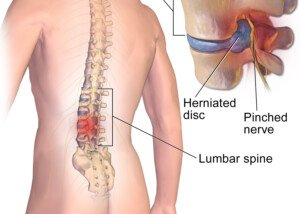
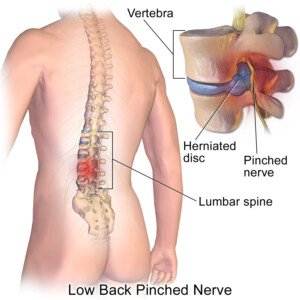
Bulging Disc: How Long to Try Conservative Treatment?
Find out how long you should give conservative treatment a try before having surgery for your bulging (herniated) disc.
If you’ve been diagnosed with a herniated (bulging) disc, you should not rush into the decision to have surgery.
The overwhelming treatment of choice for a herniated disc is conservative — even if the pain is pretty bad.
You may want to get a second opinion if you feel that a recommendation for surgery is coming prematurely.
But the Fair Question Is…
However, how long should you try the conservative approach before it’s fair to conclude that it just won’t solve the problem?
- Cold packs
- Warm packs
- Physical therapy
- Floor stretches
- Yoga
- Acupuncture
- Over the counter pain relievers
“The timing of non-operative care depends on the individual scenario,” says Dr. P. Justin Tortolani, an orthopedic surgeon and spine specialist with University of Maryland St. Joseph Medical Center.
“If someone presents with a weakening in the leg or foot, we might watch cautiously for a few weeks.
“It means that the nerve is compressed by the disc herniation and is being damaged, and generally, means the nerve fibers in each nerve have been compromised so that they’re not transmitting signals to the muscles.
BruceBlaus/CC
“It can be permanent and that’s why we have a lower threshold for considering surgery in a patient who has weakness and is not improving.
“It’s also important to rule out other causes of weakness even with someone with a disc herniation, like Lou Gehrig’s disease or trauma, or syphilis.
“If they present with severe weakness and are showing improvement, they will continue to watch and continue to use non-operative treatment.
“Even with pain, if they are showing signs of strength coming back, we’ll continue to treat without surgery.”
As far as physical therapy, which may be done at home, the patient needs to faithfully stick to the entire exercise regimen in order to give it a fair chance.
Improving symptoms from a herniated or bulging disc through physical therapy can take time.
PT focuses on reducing pain, restoring mobility and strengthening muscles around the spine.
Techniques may include exercises, stretches and manual therapy.
Patience is very important, as it often takes weeks or even months to see significant improvement.
Progress varies based on the severity of the herniation, individual health and adherence to the therapy plan.
Regular follow-ups with the therapist ensure that the treatment is effective and adjusted as needed.
 Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
Dr. Tortolani’s vast experience includes treating all disorders of the spine including herniated discs, spinal stenosis, and adult and adolescent scoliosis.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/TB studio
Can Swollen Anus in Cat Be Caused by Cancer?

How often do you inspect your cat’s anus? Sure, many cat owners don’t like to do this, and in fact, outright avoid it.
However, if your beloved cat has a swollen anus, this can be caused by cancer, says veterinarian Dr. Jules Benson, BVSc, chief veterinary officer with NationwideDVM, a pet insurer company.
Swollen Anus in a Cat: Common Cancers
“Yes – swellings or visible masses around the anus can be caused by cancerous growths,” says Dr. Benson.
The most common abnormal growths in the anal area of a cat are anal gland adenocarcinoma and fibrosarcoma.
“Your vet can help to determine what the cause might be by examining your pet and taking biopsies of any swellings,” says Dr. Benson.
“Unfortunately, adenocarcinoma and fibrosarcoma do not have good prognoses, but evaluation by a veterinarian or even consultation with a veterinary oncologist can result in positive outcomes.”
Treatments Are Expensive
“While these treatments are often expensive, having pet insurance that covers standard cancer treatments can make the difference between being able to pursue the most cutting-edge treatment options, versus palliative care to just keep your pet comfortable,” says Dr. Benson.