Muscle Twitching: Why You Should Feel Good About Twitching Muscles

Muscle twitching is quite a popular topic, but not one you’ll hear a lot about at the water cooler.
In cyberspace, twitching muscles are discussed quite prominently, because muscle twitching, though extremely common, is also a symptom of one of the most feared fatal diseases: amyotrophic lateral sclerosis (ALS).
But twitching muscles don’t mean you have ALS, any more than a little gas means you have colon cancer.
Unfortunately, once a person gets into the “I think I might have ALS” groove, the anxiety over this can become chronic — unless the person learns to see muscle twitching for what it really is: just tired muscles working their issues out.
“The delicate balance between nerves, their stimulation and chemistry, and the muscles they feed is often affected by fatigue, stress, caffeine or other quite benign influences,” says Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
He adds: “When the balance is not correct, the muscle can twitch in a seemingly random fashion, not under your control.
“It does not take much; staring at the computer screen too long can start the lower lid dancing.
Freepik.com, jcomp
“The vast majority of such twitching is self-limiting, and resolves with correction of the underlying defect.
“As with many other weird symptoms, if it is not getting better, or if it seems really abnormal, see your health care professional.”
Anyone with a lot of muscle twitching will tell you that movement almost always stops the twitching.
Perhaps this is because when a muscle is forced to work, it’s not relaxed enough to twitch.
And anyone who twitches a lot will tell you that most muscle twitching occurs while in a relaxed state.

This is maybe because a relaxed, at-rest muscle can “feel free” to twitch all it wants.
Dr. Leavey says, “Try this: Stand in a doorway and lift your arms, hard, into each doorpost. Hold that position for about 30 seconds.
“Now step out and let your arms relax by your sides. OMG – MY ARMS ARE COMING UP ALL BY THEMSELVES!
“By stressing one group of muscles, resting them allows the other group, that was opposed by the exercise, to take action.
“Similarly, muscles are always adjusting our balance and status, shifting weight on the chair or feet, and, if you are at rest, you’re going to feel that.
“You’ll feel a twitch or movement that makes no sense. Well, to your body, it does.”
The reason why there is a certain percentage of people out there who obsess about the possibility of having ALS is because they were in the wrong place at the wrong time: They googled those keywords: muscle twitching.
Googling these words will bring up links to ALS, but also multiple sclerosis, a few other neurological disorders and Lyme disease.
One day I put my legs through a punishing weight routine at the gym.
They were sore the next day; delayed onset muscle soreness. But I used my treadmill that next day, running on top of the soreness.
My hamstrings were aching and stiff, and I took to sitting at the computer for an extended time.
Lo and behold, the twitching began in my hamstring muscles. But I must say, it felt GOOD! It was almost like tiny fingers were giving me a nice massage.
It felt like miniature fingers were in there, working their way around in my beat muscles, working out the accumulation of lactic acid and other byproducts of anaerobic exertion (from the weightlifting and also the cardio).
And when the twitching began dissipating, I was disappointed. I wanted this automatic massage to continue.
But I guess the job of the twitching muscles was completed; perhaps the lactic acid had been dispersed.
So next time your muscles twitch, don’t despair; think of it as your body’s built-in massage mechanism for fatigued muscles.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Cookie Studio
Why Does Running Increase the Urge to Urinate?
Is it just imaginary, or does running really increase your need to take a leak?
Have you ever noticed that you seem to have to urinate more when you’re running, whether it’s outdoors or on a treadmill? There are a few explanations for this.
The first one comes from Marc I. Leavey, MD, a primary care physician with 40-plus years of experience.
He explains, “The act of running, itself, can cause pressure or shifting of abdominal or pelvic organs, putting pressure on the bladder, with the results that cause a pause.”
The second explanation is that while exercising, you’re guzzling more water than you think you are, and hence, you eventually have to relieve yourself before the workout is completed.

Freepik.com
A third explanation is that you actually don’t have to relieve yourself any more frequently when you run, but rather, you’re more sensitive to even just a little urine buildup in your bladder when you’re doing any kind of impact activity — of which running is one.
In other words, it’s very important to you to be as comfortable as possible when doing aerobic exercise.
So even a tiny bit of urine in your bladder will get your attention — the same amount that would go ignored if you were sitting at a computer.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Noise vs. Odor Sensitivity: Which Should You Tune Out?

Why are people told to “just tune out” annoying sounds, but these very same critics don’t feel this way when something begins stinking really bad?
How many times have you complained about a noise and were told to “just tune it out”?
Ever wonder if your critic could apply this same advice—tuning it out—should he or she suddenly find themselves sitting next to someone at the movie theatre with underarm odor?
“Oh, just tune it out,” someone once told me when I mentioned that a strange humming had started up in my bedroom wall.
It turned out to be from a water pump a few blocks away, and the water pipes running up the street were conducting the sound.
If I had told this person, “Lately there’s this strange smell coming from my heating vent,” he would have told me to check it out, get it resolved.
Next time you label someone with “noise sensitivity” and/or tell them to “just tune it out,” ask yourself how you’d feel if you were met with this same reaction upon complaining that your coworker, whom you must work close beside with every day, has really bad body odor or foul breath. Yes, just tune it out.
Or how about the reek of sewage? Suppose right outside your house, where you like to sit on the deck, there develops the stench of sewage.
- Could you tune this out?
- If it bothers you, does this mean you have some kind of “sensitivity” to odors?
- Does it mean you have some kind of glitch in your brain or obsessive compulsive thought disorder?
Of course not! So why do people who complain of noise pollution or some kind of intrusive sound get labeled as being “sensitive to noise” or neurotic?
Granted, a foul or burning-type smell should be investigated, as it could indicate a problem that needs prompt mitigation.
If you suddenly smell chemicals, gas, something burning or what seems to be rotting flesh, this should not be ignored.
But there are other bad odors that you know are harmless, such as someone’s armpits and breath.

Shutterstock/Aaron Amat
Yet why not tune these benign odors out? I can go on and on with this, because I just don’t get why people are quick to invalidate noise complaints but not odor complaints.
One time my brother told me to “just ignore it” in reference to some kind of noise I had complained about.
I fired back, “If you think tuning it out is so easy, let’s imagine your neighbor is playing a recording artist whose voice you absolutely cannot stand—volume up—all day long. Could you tune it out?” He had nothing to say about that.
What does a doctor say?
“We have five senses, they say, but the five are not really created equal,” says Marc I. Leavey, MD, a primary care physician with 40+ years of experience.
Smell, it turns out, may well be the first sense of which we are aware. The sense of smell is hardwired to an area at the top of the nasopharynx, called the cribriform plate, and is active essentially at birth.
“The sense of smell helps us find food, recognize the scent of our mother, and other vital needs.
“While we can hear from an early age, the startle of a baby to a loud sound is evidence of that we need to learn what sounds mean, learn language and music.
“These learned sounds need processing by the brain to be understood; and can thus be filtered out. Scents that are primary stimuli to our senses are not so easily ignored.”
Noise Sensitivity vs. Odor Sensitivity
There actually exist disorders relating to the intolerance of sound. One such condition is called phonophobia.
But if you’re complaining that the water pump to your apartment complex’s pool squeaks throughout the night, interfering with your sleep, this is not a sign of phonophobia — or another disorder called hyperacusis, which is intolerance to sound.
Certain sounds are intolerable to some people but embraced by others. A classic example is that of children’s screams during play. You either hate this or delight in this, it seems.
Same with thunder. Some people enjoy hearing the rumbles, while others are put on edge. Some people love opera music while others cringe.
But when it comes to bad odors…the aversive nature is universal. How many people like the stench of garbage?
How many people do you know enjoy inhaling sewage odor or the stench of a public porto-o-potty?
Does anyone like the smell of rotting fish or vomitus? How about hot tar?
And I doubt that anyone hates the aroma of freshly baked bread, brewing coffee and a bouquet of flowers — though something tells me not to bet on that.

Dr. Leavey was formerly with Mercy Medical Center in Baltimore, MD, where his focus was primary care and internal medicine. He has a blog, STRING OF MEDICAL PEARLS.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Tinnitus Freepik.com, katemangostar
Source: hyperacusis.net/hyperacusis/4+types+of+sound+sensitivity/default.asp
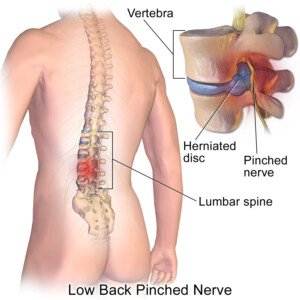
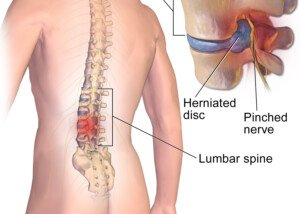
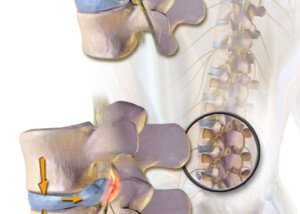
Herniated Disc Symptoms vs. Spinal Tumor: Symptom Comparison

“Both herniated disc and tumors can present with symptoms that are consistent with the nerve compression,” says Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
“However, the pain from herniated disc gets better with rest, but the pain from tumor may get worse at night, laying down,” adds Dr. Park, a neurosurgeon.
Will the pain from a tumor subside, however, with daytime rest, as in resting in a recliner chair?
Dr. Park says, “Usually, pain from tumor does not get better with daytime rest.”
However, he adds that heat, ice, ultrasound and massage will yield temporary relief of pain.
What symptom description might a patient tell a neurosurgeon/spine surgeon that would make the surgeon suspect a tumor vs. a herniated disk?
“The most important is the pain that doesn’t get better with rest at night.” says Dr. Park.
Resting at night in bed relieves the area of the forces of gravity.
When a Doctor Suspects Cancer
When doctors are presented with a patient complaining of pain that seems to be from a herniated disc, the doctor doesn’t automatically suspect cancer unless the patient reports that it does not respond to rest and gets worse at night.
“The spinal tumor is much less frequent than the disc problems,” says Dr. Park.
Tumors in the spine account for about 10-15% of all central nervous system tumors.
Primary spinal cord tumors, which originate in the spine itself, are even rarer, with an estimated incidence of two to 10 cases per 100,000 people annually.
These can occur in the spinal cord, nerve roots or surrounding structures.
Interestingly, most spinal tumors are the result of a primary cancer elsewhere in the body that hahs spread.
However, primary spinal tumors are often benign — but can still cause serious symptoms due to their location.
Because they are rare, diagnosis may be delayed, especially in early stages when symptoms, such as back pain, can mimic more common conditions — such as a herniated disc.
“But when we order MRI for disc problems, the tumor will be visible as well, if present,” says Dr. Park.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
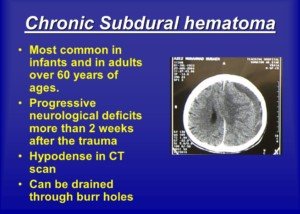
Migraine Headache vs. Chronic Subdural Hematoma

A neurosurgeon says there is one distinguishing feature between a migraine headache and chronic subdural hematoma head pain.
Chances are, if you have a chronic subdural hematoma, you might remember in your recent history getting hit on the head or bumping your head hard on something.
But some patients with cSDH are unable to report the head trauma that caused it.
This is because sometimes, the “trauma” seemed insignificant at the time, such as a run-of-the-mill bonking the head on the car door frame when getting into the car. It’s noticed at the moment, but is quickly forgotten.
Five weeks later when the headache from the chronic subdural hematoma arises, the patient does not link it to the little mishap with the car door frame.
And all it takes is this seemingly minor trauma to induce a cSDH in an elderly person.
But a person over age 60 may also have migraines, and people younger than 60 can get a chronic subdural hematoma.
“One distinguishing feature is that the headache from cSDH is worse in the mornings,” says
Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
He is a neurosurgeon and continues, “Migraine headaches are severe, and associated with light, sound, etc., and usually unilateral.” That means one-sided.
“At night, when we lay flat, there is an increase in venous blood return to the heart and increase in venous pressure. so, the soft structures, such as discs and nerves and brain, get swollen or get larger, which causes a bit more pressure on the brain and this causes worsening headache.”
What about onset of migraine?
Is it always gradual? Or can it be sudden?
“Depends on the type of migraine headaches, but usually the onset of migraine headache is much faster than chronic subdural hematoma, which develops over days,” says Dr. Park.
There are exceptions to the rule of developing over days, however.
My mother was diagnosed with a cSDH six weeks after she fell and hit her head.
She awakened one morning with a horrible headache.
The day prior, going all the way back six weeks, she had not had any headaches.
Even when she got into bed the night prior, she felt perfectly fine.
Sometimes, the brain does not act in ways that we think it should.
Like that old saying goes, “If the human brain were simple enough for us to understand, we’d be too simple to understand it.”
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Prostock-studio
Risk of Chronic Subdural Hematoma in Elderly Who Exercise

A chronic subdural hematoma is a gradual brain bleed that’s common in the elderly.
Can exercise bring this on, being that sometimes exercise involves jarring or erratic movements?
Perhaps you know that a whiplash-type movement of an elderly person’s head can actually cause a very slow bleeding in the brain: the chronic subdural hematoma.
The bleeding does not occur immediately, as would be the case of the far more life-threatening acute subdural hematoma.
A whiplash can result from a fender bender or even a fall in which the person’s head doesn’t even strike anything, but it gets jerked enough to tear a tiny blood vessel in the brain.
Although whiplash is commonly associated with neck pain and stiffness, the impact on the brain can also cause invisible injuries such as a headache, and of course, a gradual bleed in the brain.
So maybe this has you thinking that you’re at risk for a chronic subdural hematoma if your older age is combined with some kind of physical activity that jars the body (and therefore head) around:
- Horseback riding
- Mini-trampolining
- Dancing
- Jumping (rope, jacks, box)
- Running, jogging, skiing
- Step aerobics class
Good News for Aging Exercisers
“I have not seen a chronic subdural hematoma on an elderly patient due to exercise,” says Charles Park, MD, neurosurgeon, and Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore. “It’s usually due to a fall or head bumps.”
Dr. Park says it is okay for people in the senior citizen age bracket to take aerobics classes, do jumping drills and the like.
A person age 60-plus is more likely to suffer a head injury falling off the horse than from the movement of sitting on one.
Senior age men and women should just be aware of the surface they are walking on (at stores, parking lots, slick floors at bowling centers) to prevent a slip/trip-and-fall — which could cause a head injury such as a subdural hematoma.
These surfaces can become hazardous, especially if they are wet, uneven or poorly maintained.
To minimize the risk of falls, seniors should avoid walking on slippery or uneven surfaces whenever possible and use handrails or other supports in potentially hazardous areas.
Meanwhile, they can exercise, jump and run to their heart’s content.
Dr. Park also points out, “Roller coaster with sudden change in direction is not recommended.”
The G forces involved here do not compare to those involved in exercise, including jumping on a mini-trampoline.
That sudden and fast change of direction can simulate a whiplash — leading to a slow brain bleed.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Mladen Zivkovic
Traumatic Chronic Subdural Hematoma in Young Adults
Can young adults get a chronic subdural hematoma from head trauma?
“It’s possible but not likely,” says neurosurgeon Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore. “Chronic subdural hematoma is usually for older people who have a lot of brain atrophy,” he adds.
This article refers strictly to chronic subdural hematoma that results from some kind of trauma, as opposed to a spontaneous bleed – which has actually been documented in medical literature to occur in young people, but it’s rare.
In general, brains shrink with age: age-related atrophy. This means more space between the brain and the skull.
It doesn’t take much trauma to tear the blood vessels in an elderly person’s brain.
If the tear is very small, blood will begin leaking, but at a very slow rate.
The space between the atrophied brain and the skull allows this blood to collect, and it can take two, even three, months for symptoms to begin first appearing.
The space allows the blood (and cerebrospinal fluid) to collect, and the symptoms of this chronic subdural hematoma may be a severe headache, altered mentation, weakness, paralysis and other symptoms that mimic that of a stroke.
In a young person, the same force of trauma to the head, that caused the chronic subdural hematoma in an elderly person, may tear the blood vessels, but due to a bigger brain (no age-related atrophy), there’s very little space, or to put it another way, there’s very tight space, between the brain and the skull.
Any bleeding will not build up and collect; it will just be reabsorbed by the body: no symptoms, no problem.
The same trauma may also not even tear the younger, stronger blood vessels.
Do not confuse chronic subdural hematoma with acute subdural hematoma.
In a young person — even a strong, very fit one — significant head trauma can result in an acute SDH – which is a life-threatening situation due to the rapid bleeding in the brain.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/9nong
Sources: ncbi.nlm.nih.gov/pubmed/19546844; ncbi.nlm.nih.gov/pubmed/16028774
Why Can Young Athletes Get a Herniated Disc?
Even young athletes can suffer from a herniated disc; it’s not just for older couch potatoes.
Charles Park, MD, neurosurgeon, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore, says that the “Disc is composed of two parts: inner soft nucleus pulposus and outer tough annulus.
“Because of the tremendous amount of pressure that young athletes put on their bodies, the pressure may be overwhelming and may tear the outer layer, and some of the inner material can herniate out and put pressure on the nerve.”
Being that most young athletes don’t develop this, what predisposing factors are present that would put the young athlete at higher risk of a herniated disc?
BruceBlaus/CreativeCommons
Dr. Park explains, “A lot depends on genetics, which we can’t do anything about. Some are born with weak annulus, which is more predisposed to rupturing.
“But also, doing a lot of heavy axial-loading kind of activities, such as squatting, will put a lot of pressure on the annulus.”
What kind of exercises can help reduce the risk of a young athlete developing a herniated disc?
Dr. Park says that “core strengthening exercises will lower the risk.”
What are some very effective exercises for strengthening the core?
The core is the group of muscles in the abdominal and lower back regions that act as stabilizers to the spine.
A thousand sit-ups a day is not the path to a strong core. Spending an hour a day on the floor doing leg lifts, leg swings, crunches, etc., is not the answer.
The best core strengthening exercises include but are not limited to:
- pushup
- pushup dumbbell row
- deadlift and back squat
- chin-up
- pull-up
- lat pull-down
- bent-over barbell row
- bent-over dumbbell row.

Planking, too, will strengthen the core. Freepik.com

Pushup dumbbell row
To help protect your spine from developing a herniated disc, young or old, you should do these exercises, and your primary consideration should be perfect form.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Sitting a Lot Every Day Raises Breast Cancer Risk

Breast cancer is linked to prolonged periods of sitting done most days of the week.
For this study, other variables were adjusted for like physical activity and body mass index, and the results still came out as follows:
A higher risk of breast cancer the more a woman spends time sitting.
Alpa Patel, PhD, headed the study that looked at the leisure sitting time in 77,462 women and 69,260 men who did not have cancer. The time spanned 1992 to 2009.
The full report appears in Cancer Epidemiology Biomarkers & Prevention, 2015.
How can a woman reduce her daily sitting time?
ANY sitting time that’s reduced counts towards a lower risk of disease including cancer.
So if a woman sits all day at work, what can she do?
Get a Treadmill Desk

If you spend a good amount of time at home on a computer, a treadmill desk will reduce significant sitting time.
Or, if it’s placed before the TV, you can reduce sitting time while watching your favorite shows.
Even if you spend only small amounts of time at home on a computer or watching TV, walking during that time will go towards reducing your chances of getting the “sitting disease.” It will lower your risk of breast cancer.
You may also want to explore the possibility of using a treadmill desk at your workplace.
I’ve been using a treadmill desk for many years now for home computer use, and believe me, it really does make a difference. You’ll get used to it faster than you think.
No Treadmill Desk?
If that’s not an option, then just simply get up every 45 minutes from the computer and stay on your feet for five minutes.
- Do yoga
- Throw some kicks
- Do mountain climbers or squats
- March in place
- Play with the dog
- Water the plants
- Stand while going through the snail mail
Perhaps you can combine workplace duties with these on-your-feet breaks.
If you can’t get a treadmill desk for home use, then pace as you watch TV: forward and back, side to side, or do some Zumba or standing yoga moves, jumping in place, squats, lunges — whatever goes.
Excessive sitting, for whatever reason, has been associated with breast cancer. That’s enough to get moving more.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/catch-my-eye
Source: sciencedaily.com/releases/2015/07/150713131429.htm
Bench Pressing with a Thoracic Aortic Aneurysm?

The guidelines for bench pressing with a thoracic aortic aneurysm are not encouraging.
If you found this article, you’ve probably been diagnosed, or know someone who has, with a thoracic aortic aneurysm—and know exactly what this is.
And you probably lift weights or were planning on taking this up, including the bench press.
“Once someone is diagnosed with a thoracic aortic aneurysm, a common question is whether or not they can exercise,” begins Jack Wolfson, DO, FACC, a practicing cardiologist in Arizona, author of The Paleo Cardiologist: The Natural Way to Heart Health.
“The concern, of course, is to avoid an event that could cause the affected blood vessel to rupture.
“There are many reports in the literature and small studies which document heavy exertion as a precipitating factor.”
CAN a person with a thoracic aortic aneurysm bench press in a safe manner?
Well, the motion of bench pressing isn’t the issue. It’s the weight of the barbell.
Lifting weights increases blood pressure during the movement (though weightlifting will lower resting blood pressure as the individual becomes more trained).
A person with a thoracic aortic aneurysm must avoid activities that raise blood pressure, because forceful pressure within the bulging portion of the aorta can cause it to dissect.
Dr. Wolfson says, “Activities to be avoided include anything which involves strenuous lifting. I tell most people that 25 pounds is probably the upper limit.”
This is where it gets tricky. A 50-year-old woman who has never trained with weights should be strong enough to bench press 25 pounds for a number of repetitions.
As a fitness expert, I know for a fact that novice women, even middle aged, can often start out with the 45 pound unloaded Olympic bar for the bench press.
As a former personal trainer, I never started my novice female clients at 25 pounds for the bench press—this is way too light.
You can imagine how light this would be to a man—especially if he’s been working out for a while.
So the restriction of lifting no more than 25 pounds, in someone with a thoracic aortic aneurysm, would seemingly more apply to lifts that recruit only a small amount of muscle and involve a non-efficient body position.
For example, hoisting eight, 25 pound sacks into a truck is more strenuous than bench pressing this same amount of weight for eight repetitions.
Suppose a man, who regularly bench presses 225 for reps, learns he has a thoracic aortic aneurysm (e.g., a chest X-ray for suspected pneumonia reveals it).
Does this mean to drop his bench press down to 25 pounds, even though 100 pounds would be a walk in the park for him?
How about a compromise of 50 pounds, since the bench press motion is done while lying down and recruits many more muscle fibers than, say, lifting a 25 pound kettlebell straight out in front of yourself?
No data this refined exists to answer these questions, but on the other hand, because this data does not exist (and maybe one day it will), such an individual should give up bench pressing altogether to avoid the temptation to return to a more strenuous level.
“Check with your doctor to devise an exercise plan that is appropriate for you,” says Dr. Wolfson.
“Make sure to ask questions about specific activities you may be considering.
“Your doctor may want to perform an exercise stress test to determine your blood pressure response to activity.”






























 Wolfson Integrative Cardiology
Wolfson Integrative Cardiology