Can Knee Bursitis Cause Pain ONLY when Kneeling?

Is that knee pain you get only when kneeling possibly caused by bursitis in this joint?
“Infrapatellar bursitis can lead to pain while kneeling,” says Devin B. Peck, MD, owner of Austin Interventional Pain in Austin, TX.
Dr. Peck explains, “In fact, superficial infrapatellar bursitis is commonly known as ‘clergyman’s knee’ or ‘plumber’s knee,’ a reference to kneeling.
“Prepatellar bursitis can also lead to pain with kneeling, although it can also result in non-painful swelling over the kneecap. Prepatellar bursitis is sometimes known as housemaid’s knee.’”
Be aware that another condition, unrelated to bursitis, can cause pain in the knee only when kneeling.
It’s called chondromalacia patella or patellofemoral syndrome.
However, this condition usually also causes discomfort when going up stairs, running, jogging and/or sometimes jumping.
The discomfort may be a strong or dull ache and/or a sensation of fullness or tightness under the kneecap.
 Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ThamKC
Wrist Pain While Lifting Weights: Causes, Solutions

A doctor provides causes and solutions to wrist pain while weightlifting.
What are the possible causes of wrist pain that is brought on during a weightlifting set?
“This can often be related to De Quervain’s tenosynovitis,” begins Asim S. Aijaz, MD, a board certified pain management specialist with Advanced Pain Care in Texas.
Dr. Aijaz continues, “This is pain along the radial (thumb) aspect of the wrist. While the exact cause is unknown, repetitive wrist movements can make it worse.
“It is often seen in new mothers who are lifting their babies repetitively. In weightlifting, hammer curls can reproduce this movement and can potentially aggravate the symptoms.”
When your wrists hurt during lifting weights, the tissue that’s involved usually relates to the tendons, as it does with De Quervain’s tenosynovitis, “but it may also be a problem in the joint such as with arthritis, or in the bone if there is a small fracture (more likely with impact exercises such as boxing or punching a heavy bag),” says Dr. Aijaz.
So which exercises should a person with wrist pain avoid doing?
Dr. Aijaz explains, “Hammer curls. Do supinated curls to relieve some of the stress along the radial aspect of the wrists.”

Supinated means palms facing forward when your arms are straight, and as you bring the dumbbells or barbell up, your palms are facing towards you.
Dr. Aijaz adds, “Avoid impact exercises. If doing burpees, make sure you are using proper form with the pushup part of the exercise and that you’re not hitting the ground too aggressively as you are approaching the pushup position of the exercise.
“Listen to your body, if you notice a certain repetitive exercise aggravates the pain, avoid it.”
What exercises can you do?
“If your pain persists you may benefit from having somebody evaluate your form to make sure you are not putting unnecessary stress on your wrists with common exercises such as pushups, bench press, curls,” says Dr. Aijaz.
“Sometimes it’s just a matter of proper hand positioning to reduce the stress: spreading out your fingers to distribute weight through your fingertips during pushups for example.”
If you’ve developed wrist pain in the course of your weightlifting regimen, ask yourself if this pain began after you one day decided to try an E-Z curl bar for biceps curls.
Though these bars are designed to reduce wrist strain, they can actually strain the wrists in someone who’s used to doing curls with a straight bar.
So if this describes you, abandon the E-Z curl bar and go back to the straight bar.
“Generally if the pain is related to a tendon issue or arthritis, one may find it beneficial to reduce the weight and adjust the form or take a break from exercises which stress the wrists,” says Dr. Aijaz.
“During your break from these exercises, you may find relief with ice and anti-inflammatories.
“As you’re getting back into your workout, you may consider wearing a wrist support and see if this helps in preventing the pain from returning.”
Carpal Tunnel Syndrome
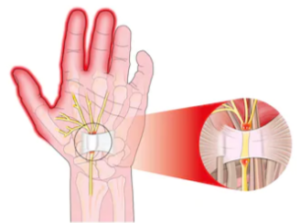
Shutterstock/Alexonline
“Occasionally patients with carpal tunnel syndrome will complain of hand and wrist pain that is exacerbated with weightlifting,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
 Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ruigsantos
sscpywrt26
Stabbing Shooting Pain in Achilles Tendon: Causes, Solutions

A doctor explains why your Achilles tendon has shooting, stabbing pain and what can be done to remedy this situation.
“Pain here is generally the result of tendonitis or inflammation of the Achilles tendon,” says Asim S. Aijaz, MD, a board certified pain management specialist with Advanced Pain Care in Texas.
He continues, “You can also develop tears in the tendon which would also cause tendonitis and pain.”
So how does this situation arise in the first place?
Dr. Aijaz explains, “As with tendonitis in other parts of the body, this is often related to repetitive use or over-exertion, causing tears or degenerative changes in the tendon.
“Bone spurs at the heel can also cause small tears in the fibers, causing Achilles tendon pain.
“Tight calf muscles can also result in increased stress on the Achilles tendon.”
Solutions
“Rest, ice, anti-inflammatories, appropriate stretching (generally the calf muscles) and appropriate shoes,” says Dr. Aijaz.
“If symptoms persist, physical therapy can be very helpful.”
Also keep yourself well-hydrated, as tendons don’t get a lot of water because they are not densely vascular.
In fact, their low level of vascularity is why it takes tendons much longer to heal than do muscles.
 Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Skumer
Red Swollen Feet after Running: Prevention

Here’s what a doctor says you can do to help prevent swollen, red feet after your running session.
“Make sure you have good shoes,” begins Asim S. Aijaz, MD, a board certified pain management specialist with Advanced Pain Care in Texas.
“Just because your shoes look beautiful and new doesn’t mean they’re still doing their job.
“The padding in shoes does wear out, and this padding is very important in helping to absorb the shock to your feet, knees, hips and back.
“A common recommendation to help avoid such overuse injuries is to increase your intensity or distance gradually, some say by roughly 10 percent per week.
“It’s also recommended to take breaks and rest one to two days per week to avoid overuse injuries.”
If after making these changes, you still suffer from swollen and red feet after your running workout, then this might be related to improper running mechanics.
And how can a person run “wrong”? One example is that of holding onto a treadmill.

Larry D. Moore
If you run on a treadmill, do not hold on other than for a momentary balance check or to change the setting.
Otherwise, sustained clinging onto the machine warps natural spinal alignment and messes up the gait pattern, right down to the feet.
If you can’t keep up with the tread without holding on, then use a slower speed.
 Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/zoff
Electric Shock Feeling in Arms from Weightlifting: Causes
Stop wondering; HERE is what a doctor says causes an electric shock feeling in your arms when you lift weights.
“Feelings of electric shocks are often related to nerve irritation,” says Asim S. Aijaz, MD, a board certified pain management specialist with Advanced Pain Care in Texas.
“This could be secondary to the nerves being irritated in the neck where they leave the spine (cervical spine nerve roots) or at some point beyond that as the nerves course through the arms,” continues Dr. Aijaz.
“Other vulnerable areas include the shoulders, elbows and wrists.”
Solutions?
Dr. Aijaz explains, “Make sure you have proper technique when you are exercising. If a particular exercise causes this pain, avoid that exercise.”
You may also want to try a different piece of equipment for the same joint motion.
For example, if you’ve been suffering from electric shock sensations in your arms whenever you do preacher curls, then try standing barbell curls in which your arms and elbows are not pressing into a surface.

Freepik.com, Racool_studio
But if the symptom persists even if you’re not pressing a muscle group or limb into a surface, then avoid that exercise for a while.
Dr. Aijaz adds, “If you believe in the idea of ‘No pain, no gain,’ you should reconsider this philosophy when it comes to pains which feel like electric shocks.
“Nerves are very slow to heal when injured. If this electric shock sensation persists, you should see your doctor.”
 Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Luka Funduk
Ankle Pain with Brisk Walking on Treadmill: Causes, Solutions

“Walking on a treadmill can lead to a sort of repetitive movement related pain” in the ankles, says Asim S. Aijaz, MD, a board certified pain management specialist with Advanced Pain Care in Texas.
“While on a treadmill, you are walking a smooth, unchanging surface, so you are constantly engaging the same muscles over and over again,” continues Dr. Aijaz.
“Compare this to walking on a trail or grass where the surface changes a small amount with each step.
“In this setting you are distributing the work a little more evenly over more muscles.”
Another possible cause of ankle pain while briskly walking on a treadmill is improper footwear. “Always make sure you have great shoes,” says Dr. Aijaz.
“Even if your shoes look beautiful and new, the padding can wear out. Your shoes do more than just make your feet look fresh in the gym; they absorb the shock that would otherwise be hitting your feet, ankles, knees, hips and back.
“Making a trip to a dedicated shoe shop can help in determining what footwear may be best for you.”
Finally, we can’t rule out the possibility that, if you have the habit of holding onto a treadmill while walking, this is responsible for pain in your ankles.
And here is why: Holding on disrupts the natural gait pattern. The faster you walk when holding on, the more unnaturally your foot strikes the tread surface.

I’ve seen people gripping the front bar at fast speeds while walking, and their feet smack down hard with each step.
Holding onto a treadmill while walking, especially briskly, skewers the kinetic chain—the way the body is supposed to move naturally, right down to the feet.
Holding onto the side rails is no better than holding onto the front of the machine.
So instead, release your hands, swing your arms naturally, straighten your spine, and just walk.
Use a slower speed or lower incline if you get dizzy or fear falling off. Your body will quickly adjust.
Holding on has taught you to become quite dependent on assistance while walking.
If you still have pain in the ankles, then re-evaluate your footwear and the fact that when you use a treadmill, the walking surface never changes and is hard.
You may want to consider walking outdoors on an earthen trail.
 Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
Dr. Aijaz has been involved with the Texas Pain Society, Spine Injection Society and the American Society for Interventional Pain Physicians.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/YanLev
Is Lots of Walking Okay Six Months after Hip Replacement?

Just how much walking can you do six months out from a total hip replacement surgery?
“Recovery following uncomplicated hip replacement is generally quite rapid,” says Devin B. Peck, MD, owner of Austin Interventional Pain.
“Important factors include the length of time between onset of hip pain and surgery, severity of pain and disability prior to surgery, and the specific type of hip replacement performed,” explains Dr. Peck.
“In most cases, formal PT should be continued for at least two months after surgery.
“After this, walking can be done as tolerated.
“Speed and duration of walking is limited only by each individual’s tolerance.
“Walking briskly or up or down hills is fine as long as the activity does not cause pain.”
Attention Treadmill Users
You may think that it’s a smart idea to hold onto the treadmill while walking because you had a hip replacement.
However, holding on skewers natural gait. In fact, the faster you walk on a treadmill while holding on in front, the more your hips will over-rotate to compensate for the lack of upper body movement, since holding on locks up the upper body.
Do not fear falling off a treadmill as long as you set the speed slowly and get used to a slow speed—while swinging your arms, moving your body naturally, the way nature designed it to move, with the upper body moving in coordination with the lower body.
Life off the treadmill means you walk all over the place without holding onto anything for support.
Thus, holding onto a treadmill while walking, even after hip replacement surgery, will not make you a more efficient, stronger walker once you step off the machine.
If you feel you’ll fall off if you don’t hold on, then either the speed is too fast and/or the incline is too high.
If your hip hurts while walking on a treadmill, then slow down (hands off) to see if that relieves the pain.
If it doesn’t, get off the machine. Try walking on a track or stable trail outdoors.
In summary, after you’ve completed all of your PT after a hip replacement surgery, you can walk as much as your body feels comfortable — go for it! Just don’t hold onto the treadmill.
 Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos
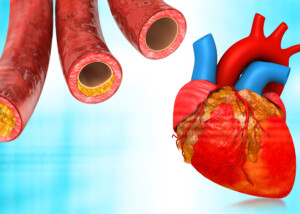
Calcium Score May Show Death Risk Even without Family History of Heart Disease
This study shows that even healthy people with no early family history of heart disease may want to get a calcium score test.
Have you had your coronary calcium score taken? This is a five minute procedure using a CT scanner.
You just lie there while the image is taken: about five minutes.
This procedure yields a numerical value that’s associated with the amount of hard (stable) plaque buildup that’s in your heart’s arteries.
A score of zero means that there is no detectable hard plaque buildup.
Calcium scoring does not show soft (unstable) plaque buildup. The soft plaque is unstable and may spontaneously break off, causing a clot in a coronary artery: a heart attack.
However, enough hard plaque can cause obstructive coronary artery disease, narrowing the interior of the arteries, leading to reduced blood flow in the heart.
Calcium Scoring Indicates Death Risk Even in People without Family History of Heart Disease
Emory University School of Medicine researchers analyzed coronary calcium scores taken from over 9,700 study subjects.
At the time these participants had their scans, none had signs of heart disease.
The calcium scores, say the researchers, were accurate in predicting all-cause mortality up to 15 years out in patients without symptoms.
Higher CAC Score = Higher All-Cause Mortality
“The presence of calcium in the coronary arteries is an early indicator of coronary artery disease,” says Carlos González Quesada, MD, FACC, attending cardiologist with Cedars-Sinai Medical Center and a cardiologist with Cardiovascular Medical Group of Southern California.
“Patients with coronary calcifications are known to be at increased risk of developing heart attacks and strokes.
“Physicians may consider starting low dose aspirin and lowering-cholesterol medications, such as statins, in patients with calcium in the coronary arteries.
“The most recent guidelines of the American College of Cardiology/American Heart Association (ACC/AHA) recommend performing a coronary calcium scan in patients who have a 10-20% risk of developing a cardiac event within the next 10 years.
“To determine the individual 10-year risk of a cardiac event, doctors enter the patient’s information into an online calculator or estimator (tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate).
“The information used by these calculators includes age, gender, race, blood pressure, the cholesterol and presence of risk factors such as diabetes, high blood pressure or smoking.
“Although family history of a cardiac event may not be present, patients may have other risk factors that would put them in the intermediate or high risk.
“If the patient is determined to have an intermediate risk, a coronary calcium scan would identify individuals who may benefit from primary prevention strategies such as aspirin and statins.
“In other words, a family history of heart disease is an important predictor of cardiovascular events — but is not the only one or the strongest one.
“For example, someone may not have family history of heart disease, but he or she may have elevated cholesterol, high blood pressure and history of smoking.
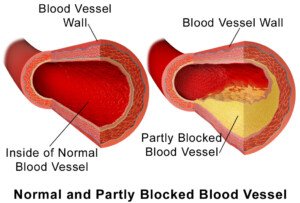
BruceBlaus
“A coronary scan may confirm the presence of early coronary artery disease.
“In the setting, the treating doctor may recommend starting aspirin and statin medication.”
 Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Brian A Jackson
Source: news.emory.edu/stories/2014/04/jjm_coronary_calcium_predicts_death_risk/index.html
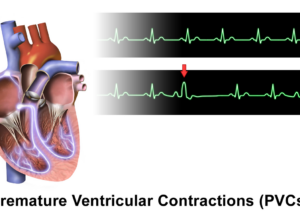
Can PVC’s Cause Early Death?

Just when you’re finally convinced that PVCs are nothing to worry about, a study comes out linking them to early death and heart failure.
UC San Francisco researchers spent over 10 years following over 1,100 participants who were from the national Cardiovascular Health Study.
“We cannot exclude the possibility that PVCs are an ‘epiphenomenon’ or some marker of future heart failure,” points out Gregory Marcus, MD, senior author of the study, which appears in full in the Journal of the American College of Cardiology.
Dr. Marcus goes on to explain that the study participants had no prior history of heart failure, and that the data in this research “would appear to be quite convincing that PVCs represent an important predictor of the disease [heart failure], causal or not.”
The relationship between the frequency of PVCs, incidents of heart failure, and death in the general population is currently not known.
The study subjects were tracked over a decade for new onset death and congestive heart failure.
A higher occurrence of PVCs was associated with decline in left ventricular ejection fraction, an increase in heart failure incidents, and greater mortality.
However, Dr. Marcus says that future studies are needed to identify “the exact types of patients, and likely the particular types of PVCs,” that are most strongly linked to heart failure.
This is all quite striking to me, because my mother has a pacemaker that is able to record abnormal heart rhythms.
At a six-month checkup, the nurse casually commented that it had recorded six-thousand-and-something PVCs (over six months).
She spoke this as though she were commenting on the common cold. She wasn’t concerned.
My mother’s cardiologist wasn’t concerned, either. Her heart rhythm was declared normal.
According to Mayoclinic.com, the following can lead to or increase the risk of CHF: coronary heart disease, high blood pressure, low thyroid (my mother has all three), faulty heart valves, heart muscle damage and diabetes.
The site also lists abnormal heart rhythms, but then states that these “may cause your heart to beat too fast, which creates extra work for your heart.”
In other words, I don’t see a description of a PVC here.
Here are a bunch of articles about PVCs. They are not as dangerous as you think.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Sources: sciencedaily.com/releases/2015/07/150706154852.htm; mayoclinic.org/diseases-conditions/heart-failure/basics/causes/con-20029801
Can You Wash Off Melanoma? Dermatologist Answers

Here’s the final answer to “Can you wash off melanoma?” given by a doctor.
I asked Gary Goldenberg, MD, of Goldenberg Dermatology, if it was possible to wash off any part of a melanoma. Dr. Goldenberg is assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
Here is what he explains: “Absolutely not! Melanoma is a malignant cancer of skin cells that make pigments (melanocytes).
“Depending on when it’s found, melanoma can be in the top layer of the skin called the epidermis (melanoma in situ) or spread down into the deeper levels of the skin (malignant melanoma).
“The deeper the lesion, the higher the chance of spreading to other organs and death from the disease.”
The reason you cannot wash off a melanoma, no matter how hard the water against your skin, no matter how vigorously you rub a sponge on it, scrub with a brush or with a loofah brush, is because the cancer cells are tough and solidly affixed to and into the skin, even if the melanoma is in situ (stage 0) or a very thin layer of cells.
In fact, when’s the last time you were able to wash off a common mole?
If you believe you’ve actually done this … then what you washed off was not a mole, but something that looked like it, most likely a benign skin barnacle (seborrheic keratosis).

Seborrheic keratosis. Shutterstock/Lipowski Milan
It was probably already loose, and you most likely vigorously rubbed over it. These can look like moles. They can also look like melanoma, but are harmless.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.