Epidural Injection for Sciatica Injected Outside the Disc?
Wondering how effective an epidural injection for sciatica would be if the injection were NOT administered directly into the problematic disc?
Well, this is a fair question for the layperson with sciatica, but the answer is very interesting:
“Epidural injections are not injected into the disc — they are injected into the epidural space,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“The purpose of an epidural injection is typically to diminish inflammation around the nerve root that can cause inflammation to recede,” he says.
“Patients who have sciatica can have inflammation of the nerve. The best route for treatment is through the use of a steroid.
“The steroid can be injected to the inflamed area and this can diminish the inflammation and therefore the pain the patient is experiencing. Steroids are not injected in the disc as a form of treatment.”
What Exactly Is Sciatica?
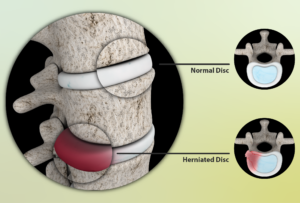
Sciatica is the name for an irritation to the sciatic nerve — an irritation that can have more than one cause.
It results in symptoms of pain, tingling, numbness and/or weakness to the areas that the large sciatic nerve innervates.
These regions of symptoms extend from the buttocks to the foot.
A classic sign of sciatica is that it affects only one side of the body, and the pain can be sudden and “shoot” down the leg.
The sciatic nerve, as mentioned, is irritated — it is compressed, the so-called pinched nerve.
Conservative treatments, in addition to the epidural injection, usually are all that the patient needs to resolve the problem. Surgery is rarely indicated.
Epidural injections are also called steroid injections, but the “steroid” is actually a corticosteroid drug, NOT the type of steroid that bodybuilders and other athletes take.
The objective is to suppress the inflammation that surrounds the irritated root of the sciatic nerve. These injections last about three months.
An irritated disc root doesn’t always involve the sciatic nerve.
The point of compression can be a little above or below. Epidural injections are frequently used for these cases as well.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com pressfoto
Chiropractic Treatment, Spinal Cord Injury in Sciatica Patient
What’s the truth about whether chiropractic manipulation might cause spinal cord injury in a patient with sciatica?
Many people who suffer the pain of a disc herniation or sciatica have considered getting chiropractic treatment, but might fear that the hands-on treatment could harm their spinal cord or column.
Though sciatica can be caused by a herniated (bulging) disc, not all cases of bulging discs affect the sciatic nerve.
But the pain in the back, butt and/or leg feels the same.
Tingling and numbness may also be present.
Chiropractic Treatment of Sciatica
Can injury to the spinal cord result via the manipulation by a chiropractic physician?
“It is possible, but not a common occurrence,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
He adds, “If the patient does have a herniated disc, chiropractors typically take X-rays and MRI scans prior to manipulations to ensure there are no problems occurring on the spine that would be a contraindication for manipulation.”
Chiropractors are trained at interpreting X-rays and MRI scans.
With that said, you should not arrange to have chiropractic treatment for your sciatica if the treating physician has not reviewed images of your condition.
There should be a discussion of the images before any manipulation begins.
Other Treatments for Sciatica
In addition to chiropractic treatment, there are other options for sciatica.
If it has been determined that the irritation is being caused by a tight piriformis muscle imposing upon the sciatic nerve, stretching exercises will be prescribed.
The patient may also opt to take the medications mentioned below.
If it’s nerve root compression, medications are one line of therapy. These include anti-inflammatories, muscle relaxants and tricyclic antidepressants.
Physical therapy is another conservative treatment, as are steroid injections (which last about three months).
Sciatica Stretches for the Piriformis Muscle

Freepik.com/yanalya

Kpa1563, CreativeCommons
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/aijiro
Can a Walker Reduce Inflammation from Sciatica?

If you have inflammation that impairs walking, you might be wondering if using a walker can reduce the so-called inflammatory chemical mediators, such as those present with a herniated disc or sciatica.
The Effect of Using a Walker on Sciatica
“A walker is not prescribed to diminish inflammation,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
He continues, “Walkers are used for patients who need assistance with walking to provide stability and prevent further injury from falling.
“A walker can help alleviate pressure on the spine and help diminish pain; however, other than short term relief, they are not prescribed to assist with inflammation.”
So if you have low back pain from spinal stenosis — which is completely different from sciatica — a walker will help relieve pain by subtracting pressure off your low back.
It’s not a treatment; it’s only a pain reliever by altering the mechanics of your walking.
Using a walker significantly alters body mechanics by shifting weight distribution and changing gait patterns.
For spinal stenosis and other conditions, it provides external support, allowing users to offload weight from the lower limbs, which reduces stress on hips, knees and ankles.
Walkers promote a wider base of support, improving balance and stability but may encourage a forward-leaning posture if not properly adjusted.
This can lead to changes in spinal alignment and reduced natural arm swing.
Additionally, users often rely more on their upper body muscles, particularly the shoulders and arms, which can cause fatigue or strain over time.
Sciatica
But if you’ve been diagnosed with sciatica, you have an entirely different situation on your hands.
You will want to engage in physical therapy and stretching exercises.
These treatment modalities are very effective at resolving sciatica pain in many people by reducing nerve compression, improving flexibility and strengthening the supporting muscles.
These treatments help correct posture, enhance spinal alignment and promote mobility.
But a walker will do zilch for the inflammatory process of sciatic nerve compression and certainly won’t help improve posture.
Dr. Perry continues, “Inflammatory chemical mediators occur when an area of the body is injured and cells release mediations which can cause inflammation to other injured areas of the body.
“Any movement or irritation of an area can increase an inflammatory mediator.”
Though it may initially sound intuitive and reasonable to just grab the walker whenever your sciatica pain acts up, this is NOT something you’ll want to do.
Your doctor will recommend treatment options that will exclude the use of a walker, and include the use of medications such as anti-inflammatories and muscle relaxants, along with possibly epidural steroid injections to reduce the inflammation.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Excessive Bed Rest from a Herniated Disc Cause a DVT ?
You’d better avoid a lot of bed rest, no matter how painful your herniated disc, if you want to avoid a DVT (deep vein thrombosis).
“Yes, bed rest is never indicated for people with back problems,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“Studies have shown bed rest for neck or back problems to be detrimental for the patient.
“Being inactive can cause serious issues to form such as blood clots. If DVT develops, it can cause a pulmonary embolism, which is extremely dangerous.”
Lying around all day in the name of pain stemming from a herniated disc is the last thing you want to do.
Pain doesn’t always mean you should take to lying around or trying to sleep it off.
It’s one thing to sleep off pain from a temporary problem, such as feminine monthly discomfort or a headache.
But a herniated disc isn’t going anywhere too soon.
You need to learn how to live with it should you opt for conservative management.
Source: myupchar. com
This means avoiding excessive bed rest or lounging around. Physical therapy is a highly recommended mode of conservative treatment.
But even if it fails, and even if you’ve decided to pursue surgery, you absolutely should not get in the habit of taking to bed rest, as this can become excessive—a major risk factor for DVT.
Part of the DVT could break off and travel to the lungs where it becomes a pulmonary embolism. The time lapse for this process is immediate.
A pulmonary embolism that’s big enough can take only moments to kill the patient — because it blocks critical blood flow involving the lungs. This can then lead to cardiac arrest.
Warning signs of a major pulmonary embolism can come on quite suddenly, and the patient could be dead before the paramedics arrive.
Key warning signs of a DVT that has embolized are: sudden difficulty breathing, chest pain and fainting.
A herniated disc, no matter how painful, combined with excessive bed rest, never mix well.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Purple Pimple Draws Blood when Popped: Melanoma?
Yes, what appears to be a purple pimple that bleeds just might be melanoma…
The term “pimple” is often used loosely, describing quite an array of bumps or tiny lesions on the skin.
So what may appear to be the type of pimple that many teenagers get may actually be something entirely different.
“Most common cause of a blood filled pimple is an angioma — a type of growth that’s genetic and filled with blood,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“These are more common as we age.” Angiomas do not really look like pimples, but they can bleed if irritated.

Angiomas. Shutterstock/Ocskay Bence
They are a striking reddish magenta color rather than purple.
When viewing these, make sure the light is sufficient so that they don’t seem purple.
Don’t let the name angioma scare you. Not all “oma” suffixes refer to cancer. “Oma” means mass or collection.
So in the case of an angioma, it’s a mass or collection of vascularity (angio refers to blood vessels).
An angioma is sometimes called a hemangioma. The “hem” refers to blood: blood vessel mass.
“A cyst can also look bloody when popped of traumatized,” says Dr. Goldenberg.
What about melanoma?
“Skin cancers, such as basal cell carcinoma, squamous cell carcinoma or melanoma, can also present this way,” says Dr. Goldenberg, referring to what seems to be a purple pimple that’s drawing blood. “Most importantly, see your dermatologist and get checked!”

Nodular melanoma; looks like a pimple.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/antoniodiaz
Itchy Red Bumps on Palm: Causes Other than Insects?

There are several possible causes of red itchy bumps on your palm, and one of these causes is especially serious, says Gary Goldenberg, MD, a dermatologist.
He runs Goldenberg Dermatology, and is assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“Most commonly, especially in adults, this is a manifestation of hand dermatitis, a type of eczema,” says Dr. Goldenberg.
“Allergic contact dermatitis may cause this alone or in combination with eczema.
“Psoriasis can also cause itchy bumps on the hands. Fungal infection of the hands usually presents with scaly patches, but can cause bumps as well. Syphilis can also look like this.”
Syphilis is the serious disorder here. And why is this sexually transmitted disease so serious?
The first symptom is a painless sore usually on the genitals or in the mouth.
The sore will go away but this does not mean you’re out of the woods.
Though the disease can be often cured with just one penicillin injection, it can also kill if left untreated.
After the initial sore heals, a rash may develop and cover the entire body, including the palms. It may not itch, but it also may.
There can be other symptoms too such as hair loss, sore throat and wart-like sores in the mouth.
In people who never get treated for syphilis, about 15 to 30 percent develop the “tertiary” form of the disease.
At this point the infection can damage the brain, eyes, nerves, blood vessels, liver and bones.
These complications may start up many years after the original and untreated infection.
Solutions for Itchy Red Bumps on the Palm
“Treatments vary between steroid creams for psoriasis, eczema or allergic contact dermatitis.
“A blood test is usually needed to diagnose syphilis, and antibiotics are needed for treatment.”
And remember, the fact that a course of antibiotics can resolve syphilis does not mean that this sexually transmitted disease is nothing to worry about.

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/WSW1985
Skin Around Eyes Is Suddenly Itchy, Dry and Flaky?
The skin around your eyes has suddenly become dry and flaky, and itches. What might this be?
Dry, flaky and itching eyes not only feel bad, but they don’t look too good, either.
Has this happened to you lately?
“This is likely allergic contact dermatitis,” says Gary Goldenberg, MD, of Goldenberg Dermatology, and assistant professor of dermatology and pathology at Mount Sinai School of Medicine.
“This condition is more common in women than men around the eyes, continues Dr. Goldenberg.
“The most common causes are nail polish, cosmetic products, hair care products and gold jewelry.
“This condition is likely to come and go unless you find out what’s causing the problem and eliminate its contact with the skin.”
Sources of Contact Dermatitis
The skin around the eyes is particularly sensitive and not immune to reactions from allergic substances.
Allergic reactions in this area can manifest as dryness, itchiness, and flaking, but may also include redness, bumps, and blisters.
Such symptoms can occur if allergens come into contact with the delicate skin around your eyes.
A common way allergens can transfer to this sensitive area is through direct contact with contaminated hands.
For instance, if you apply antibiotic creams or other topical medications and do not wash your hands thoroughly afterward, residues of these substances can linger on your fingertips.
When you then touch your face or rest your cheek in your palm, these allergens are transferred to the skin around your eyes, potentially triggering an allergic reaction.
Similarly, substances like sawdust, which is known to cause contact dermatitis, can also be a culprit if you are exposed to it regularly.
Other potential irritants include various chemicals such as solvents, insect repellents, rubbing alcohol, bleach, and detergents.
Even perfumes and the rubber used in goggles can contribute to contact dermatitis around the eyes.
To prevent these issues, it’s important to practice good hygiene, such as washing your hands after applying topical products and avoiding direct contact with known allergens.
If symptoms persist, consulting a healthcare professional can help identify the specific allergen and provide appropriate treatment or preventive measures.
Solutions
Gloves act as a barrier, preventing direct contact with harmful substances like solvents, detergents and other chemicals that can cause dermatitis or other skin issues.
Using gloves can also help prevent the transfer of these chemicals to your face, particularly if you inadvertently touch your eyes or other sensitive areas.
Dr. Goldenberg explains, “Treatment involves moisturizers, such as aquaphor, topical steroid cream and non-steroidal creams, like elidel and protopic. Most importantly see your dermatologist, find out the cause and avoid it.”

Dr. Goldenberg of Goldenberg Dermatology provides comprehensive care in medical and cosmetic dermatology, including melanoma and other skin cancer, moles, psoriasis, eczema and acne. He is the medical director of the Dermatology Faculty Practice, NY.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Miriam Doerr Martin Frommherz
Memory Loss, Non-Compliance after Hip Replacement Surgery

There could be a most surprising reason for a patient’s non-compliance and memory problems after hip or other surgery…
—and it’s not the anesthesia or painkiller drug side effects.
An elderly person has hip replacement surgery (or any operation for that matter), and after the postoperative delirium wears off, you find that he or she has short term memory issues and is non-compliant with orders from medical staff.
- Could this still be the anesthesia?
- Could it be just an exacerbation “from all the drugs” of the patient’s pre-surgical personality?
Could it be that the patient’s thyroid levels were knocked out of whack from the physical stress of the surgery?
THYROID?
My mother had already been diagnosed with hypothyroidism about six years prior to her total hip replacement surgery.
Back then, the symptoms blew in like a tropical storm immediately following minor knee surgery, and in retrospect, I realized that before that knee surgery, low thyroid symptoms were barely bubbling on the surface but not enough to grab anyone’s attention.
So now she has a hip replacement, and right away, I’m thinking that this assault on her body threw her thyroid out of whack—even though she’s already been taking Synthroid (her daily thyroid pill).
My thinking is that the physical stress of the hip replacement “desensitized” (for lack of a better term) her body to the effects of her usual Synthroid dose.
Well, I’m not a doctor or nurse, but several years ago I interviewed Dr. Ken Holtorf, a thyroidologist, about this very topic: that the stress of surgery could stress the thyroid and cause noticeable symptoms. He explains that yes, indeed, this CAN happen!
Non-Compliance, Short-Term Memory Loss After Hip Replacement
My mother’s non-compliance was alarming. I won’t go into detail, but suffice it to say, it had the family very worried.
The short-term memory loss was aggravating, and there was also impaired judgment.
Nurses and a doctor kept telling me this was the result of the general anesthesia (she suffered postoperative delirium).
We also attributed the issues to age related cognitive decline, and in fact, prior to surgery, this age related decline was already evident — there had been memory lapses and irrational thinking, but she was still functional.
At the rehab center, the memory problems and non-compliance were very obvious, and she was also sleeping too much and popping in and out of a depressed or easily anguished state. At least on one occasion my mother complained of being cold.
None of the nurses suspected her thyroid. This should have jumped out at them because they were giving her the Synthroid every morning.
But very few people, even medical personnel, realize that the stress of surgery could upset thyroid levels even in someone who’s already taking a thyroxin pill.
I was the only person who suspected this. In fact, prior to the hip replacement, I wondered about it, and planned on pushing for a thyroid blood test at some point after the surgery.
I spoke to the rehab center’s doctor about ordering this simple blood test, and he put the order in.
Two days later the results came back: My mother’s result was 10! It should not have been higher than 5.5.
(Low thyroid causes a high score, by the way; that’s just the way the labs do it). So 10 is high, when you consider that the value should not exceed 5.5.
Her Synthroid dose was immediately increased! This should improve her state of mind and reduce the desire to sleep so much.
Memory problems, non-compliance, irrational thinking, impaired judgement—and especially if combined with feeling cold and excessive sleep — these issues following a surgery could be, at least in part, explained by a stressed thyroid.
Push for the blood test! Don’t just attribute all of these problems to age related cognitive decline.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ By pathdoc
Can Underactive Thyroid Symptoms Suddenly Escalate?
Surgery on someone with early low thyroid can kick symptoms into high gear following the operation.
Indeed, symptoms of hypothyroidism (low thyroid) can mosey on along for quite some time, then suddenly escalate out of seemingly nowhere, not just from surgery.
Underactive thyroid symptoms can suddenly blow in like an unexpected storm, escalating for no apparent reason.
The patient may have already been experiencing low thyroid symptoms for a number of months, in a subtle way that really didn’t attract any attention, or maybe a little attention, but certainly not to the point where any alarm bells went off.
And then suddenly, the person with underactive thyroid, who’s been quite functional all this time, rapidly deteriorates over a matter of days.
I asked Dr. Kent Holtorf, MD, if it’s common for the symptoms of hypothyroidism to escalate after a period of existing just below the radar.
“Yes, that is very common,” says Dr. Holtorf, thyroidologist and founder of Holtorf Medical Group in California.
“Often, people have low-level symptoms for years and are told everything is fine and then it escalates. This can be due to a viral infection or significant physiologic stress, which lowers thyroid levels.”
Depression can be caused by hypothyroidism.
For several months, my mother seemed a bit moody, but nobody thought anything of it, especially since it coincided with knee pain resulting from a fall at a bowling center.
Earlier that year she had endured the mental stress of my father’s total knee replacement.
Not long after he was just about independently functioning, my mother slipped at the bowling center.
For the next number of weeks the knee pain came and went. We went on vacation and a few times my mother had panic attacks where she was crying, thought she was dying and reported severe pain throughout her body.
After vacation she kept saying that the mysterious pain throughout her body was “connected” to the knee injury. She began losing her appetite, but was still fully functioning.
Finally, she had an MRI, which had been delayed because her physician kept insisting she didn’t need an MRI. The meniscus was torn and she scheduled arthroscopic knee surgery.
As the days approached she grew increasingly edgy and disgruntled, which was out of character because she had had two shoulder surgeries years prior with no preceding mood changes.
The morning of the knee surgery, all hell broke loose: My mother was sobbing and inconsolable, trembling, could barely walk (due to whole-body weakness.
She had always been able to walk decently with the knee problem), and kept fearing she’d die in surgery.
Immediately following the surgery I knew something was wrong. This wasn’t my mother.
Within 48 hours following the surgery, my mother sunk into a deep, dark hell of clinical depression.
And for the next six weeks, was disabled, exhibiting classic signs of severe depression: wanting to die, complete loss of appetite, multiple crying episodes a day, refusal to leave her bed, irrational thinking, and a “bonus” symptom: multiple panic attacks daily, where instead of wanting to die, she thought she was dying.
Cymbalta resurrected her, but other problems began appearing (such as severe constipation and excessive sleepiness, which we thought might be latent side effects from Cymbalta!), which ultimately led to a blood test that revealed the true culprit: hypothyroidism!
Suddenly, it hit me: In the months preceding the knee surgery, my mother often complained it was cold, even though the house temperature was 74 degrees.
I had noticed her hair loss, but attributed it to older age. Everything now made sense.
Her underactive thyroid had been there all along, but escalated due to the knee arthroscopy.
I asked Dr. Holtorf if this non-invasive surgery was sufficient to escalate a low-lying hypothyroidism. He said, “Yes, it is significant physiologic stress and can trigger.”
In other words, stress to the physical body can cause a pre-existing, and even clinically undetectable, hypothyroidism to escalate like mad.
The escalation with my mother’s hypothyroidism also included memory lapses, confusion and irrational thinking, which can all result from underactive thyroid.
Hypothyroidism isn’t just weight gain and fatigue (my mother lost weight due to loss of appetite from depression).
Hypothyroidism can cause a whole slew of symptoms, and they can lie virtually dormant (subtle, seemingly trite, such as tingling in the fingertips), and then escalate and masquerade as another medical condition, such as major depression.
However, major depression can have physical causes, and low thyroid is definitely one of them.
 Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Depositphotos.com
Can Chest Pain Be the Only Symptom of Arrhythmia?

Chest pain has many causes, and one of them is arrhythmia, which means an abnormal rhythm of the heart.
“Chest pain is rarely the only symptom of an arrhythmia — much more common are palpitations, shortness of breath and lightheadedness,” says Peter R. Kowey, MD, FACC, Professor of Medicine and Clinical Pharmacology, Jefferson Medical College; Chief, Division of Cardiovascular Diseases, Main Line Health System; and author of “Lethal Rhythm,” a medical mystery.
This doesn’t mean that if you’re experiencing chest pain along with some shortness of breath, and maybe also another symptom like what seems like skipped heartbeats . . . that you can safely assume that this is arrhythmia rather than an impending heart attack.
Problem is, the symptoms of an impending heart attack, and that of an arrhythmia, are strikingly similar.
Not only that, but just the two symptoms – chest pain and shortness of breath (or difficulty breathing) – can mean many possible medical conditions, including GERD (gastroesophageal reflux disease) and pulmonary embolism.
You cannot diagnose what chest pain and accompanying symptoms are at home.
If you’re experiencing these symptoms, a trip to the emergency room is warranted for a full evaluation to rule out a pending heart attack. Chest pain and shortness of breath can also mean a problem with a cardiac valve.
Dr. Kowey explains: “Most heart arrhythmias are not life-threatening, but certain arrhythmias can cause life-threatening complications such as stroke.
“The problem is that there are many different types of arrhythmias, some of which need little or no therapy and others more aggressive management, such as with surgery, catheter procedures or drugs. In addition, not all arrhythmias cause symptoms.”
Causes of Arrhythmia
- Emotional distress
- Side effects of medications
- Drug abuse
- Smoking
- Diabetes
- High blood pressure
- Coronary artery disease
- Heart attack
The risk factors for a disturbance in cardiac rhythm overlap the possible causes (such as coronary artery disease), and some of the risk factors lead to the causes, such as obstructive sleep apnea, obesity, and drinking too much alcohol, which can damage cardiac tissue.
Other risk factors include thyroid problems, caffeine and electrolyte imbalance. Amphetamines and cocaine can cause a deadly arrhythmia known as ventricular fibrillation.
Here are the symptoms of a heart arrhythmia: fainting or near-fainting episodes; dizziness; lightheadedness; a slow heartbeat; a fast heartbeat; a sensation of fluttering in the chest; and of course, chest pain and shortness of breath.
The perception of arrhythmia symptoms is not indicative of the severity of the problem.
Neither is the absence of symptoms, i.e., a life-threatening arrhythmia can present with minimal or mild symptoms, while less severe rhythm disturbances can interfere significantly with normal function.
Chest pain and difficulty breathing are two symptoms that should never be passed off as “just stress.”
Dr. Kowey explains, “It’s important to consult with a physician trained in the treatment of cardiac rhythm problems and to undergo a thorough evaluation that could include imaging of your heart and other diagnostic tests including electrophysiologic (catheter) studies.”
 Dr. Kowey’s principal area of interest is cardiac rhythm disturbances, and his group has participated in a large number of pivotal international clinical trials.
Dr. Kowey’s principal area of interest is cardiac rhythm disturbances, and his group has participated in a large number of pivotal international clinical trials.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.