Colon Cancer vs. IBS: Alternating Constipation & Diarrhea
Constipation alternating with diarrhea is a classic symptom of irritable bowel syndrome, but also can be caused by colon cancer.
What if you find that lately, you’re experiencing this troubling symptom?
“Alternating constipation with diarrhea with abdominal pain is very classic of IBS,” says Pankaj Vashi, MD, Lead National Medical Director, National Director, Gastroenterology/Nutrition/Metabolic Support, Cancer Centers Treatment of America.
Dr. Vashi continues, “When it occurs in anyone above the age of 40 with normal bowel habits prior to that, should be evaluated for other conditions like colon cancer.
“Again, in colon cancer these symptoms will be more acute and associated with other concerning symptoms.”
“Acute” means a sudden, notable onset as opposed to a gradual, quieter onset.
However, the “other concerning symptoms” that can be caused by colon cancer can also be caused by IBS.
They include stomach/abdominal discomfort or pain, a feeling of having to void but nothing comes out, fatigue, unexplained weight loss and bloating.
However, a symptom that can be caused by colon cancer, but is never caused by irritable bowel syndrome, is blood in the stools.
This can appear as fresh, red blood, or as a dark or black “tarry” substance in the BMs. Ever see melted tar? This is what “tarry stools” means.

Shutterstock/Ronald Plett
This doesn’t always mean colon cancer (other possible causes of blood in the stools are ulcers and hemorrhoids), but it DOES mean this:
Don’t waste another moment in getting evaluated by a gastroenterologist.
IBS is a diagnosis of exclusion. All other causes of diarrhea alternating with constipation, including colon cancer, should be ruled out before a diagnosis of IBS is made!
 For 20 years Dr. Vashi was instrumental in developing robust gastroenterology, and nutrition and metabolic support programs in all five Cancer Treatment Centers of America centers.
For 20 years Dr. Vashi was instrumental in developing robust gastroenterology, and nutrition and metabolic support programs in all five Cancer Treatment Centers of America centers.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/tonodiaz
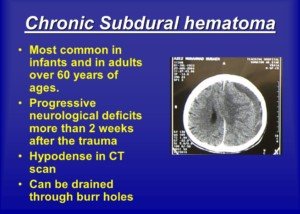
When Chronic Subdural Hematoma Symptoms Begin in Young Adults
Are symptoms of chronic subdural hematoma in people under 65 more likely to occur sooner within 90 days when compared with elderly patients?
Anyone who clicked on this article probably already knows that by definition, the symptoms of a chronic subdural hematoma begin anywhere from three weeks to three months after the initial trauma to the head.
If the symptoms begin presenting themselves a few days to 21 days after, the condition is termed subacute.
If the symptoms begin kicking in sooner than a few days, it’s an acute case.
Some medical schools of thought define subacute as symptoms occurring between a few and only seven days.
When do symptoms of a chronic subdural hematoma begin appearing, usually, in elderly people vs. adults under age 65 within that 90 day grace period?
Would it be more typical for the symptoms in someone under 65 to begin appearing sooner, say, in the first one to two months?
“This is plausible,” begins Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore, and a neurological surgeon.
Dr. Park explains, “As we get older, the brain shrinks and gets smaller. So, the symptoms from the subdural hematoma may not be evident early for the elderly patients because they have more room to ‘accommodate’ the extra mass of the subdural hematoma.
“Younger patients will show symptoms earlier due to the ‘full’ brain.”
Younger Adults Have Bigger Brains
The younger, bigger brain has a tighter fit within the skull, reducing the space between the brain and the dura mater tissue.
With this much less space, if blood begins leaking within it, it will more quickly, within that chronic phase timeline, begin producing symptoms—usually a very bad headache (though other neurological symptoms can also result).
However, the elderly person’s brain is typically smaller (sometimes referred to as age-related brain atrophy).
This makes more room, as Dr. Park says, for a collection of blood and other fluid to fill up.
So it takes longer for this increasing collection or mass to begin putting pressure on the brain, and hence, causing symptoms.
Another thing to consider is that in the elderly, symptoms can be missed, making it seem that the symptoms “began” later than they actually did.
For example, suppose an elderly person (who struck his head a few months before) has been showing signs of a little dementia for the past year.
If the chronic subdural hematoma is now causing impaired cognition, family members might attribute this to the pre-existing dementia getting worse.
Awakening with weakness in a limb might also be passed off as part of old age.
In fact, even a really bad headache might not trigger suspicions in family members of any bleeding in the brain.
When my elderly mother woke up one day with a “crown of thorns” headache, my father was convinced this was due to eye strain the night before at her sewing machine.
And he thought nothing of her leg weakness; he thought it was just another transient setback of “overworking herself,” because the day before she had attended her first Silver Sneakers exercise class.
I pointed out that when she walked, her left foot kind of dragged. My father denied this and said I was imagining it.
So you see how the symptoms of a chronic subdural hematoma can be missed by a spouse?
He wasn’t even concerned that she had upchucked a little bit, thinking it was something she had eaten the day before.
(It’s possible that the nightmare of my mother’s quintuple bypass surgery a few months prior had desensitized my father).
All day long I pressed for the ER visit, and finally my father relented, and soon after she arrived, my mother was diagnosed with a chronic subdural hematoma.
Her symptoms came on suddenly, however, so the delay in diagnosis was only by hours, not days or weeks.
Had my mother been living alone with nobody aware of these symptoms, it’s anybody’s guess how long it would have been before she got medical attention, because she herself had not been worried over these symptoms.
This apathy might have been due to the chronic subdural hematoma.
But when a young person awakens with these symptoms, it’s typically very alarming and they waste no time seeking medical attention.
With that all said, a person under age 65 is more likely than an elderly person to begin experiencing the symptoms of a chronic subdural hematoma one to two months out from the initial trauma, since there is less space in their bigger, tighter-fitting brain to accommodate the increasing collection of blood and cerebral spinal fluid from the damaged veins.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Very Elderly on Coumadin Hits Head but NO Subdural Hematoma?

Can it be possible for an advanced elderly person on a blood thinner to escape a chronic subdural hematoma after a hard hit to the head?
Well, I don’t know what really constitutes a “hard” hit to the head, but when my father at age 89 fell in the middle of the night (nobody witnessed it), the result was a “goose egg” hematoma (collection of blood) on his forehead (a bulging bruise), plus immediate neurological symptoms.
The hit to his head must have been pretty good because he was irrational, then exhibited perseveration (repeatedly asking if he had fallen, despite my mother answering affirmatively every time he asked).
Then the amnesia over the past two weeks was exhibited. The week prior he had had a knee replacement surgery, and he at times thought it had not yet occurred, then was asking if he’d had it.
In addition to advanced age and the neurological symptoms, my elderly father was also on the blood thinner Coumadin at the time.
So we have an ugly recipe for a chronic (and even subacute) subdural hematoma.
I was pretty sure he was going to eventually—weeks down the road — begin exhibiting symptoms of a chronic subdural hematoma, even though the CT scan a few hours later, and 12 hours after that, was normal.
So I was on edge for the next 90 days, and warned my father to limit his driving, in case a neurological symptom suddenly appeared while he was behind the wheel.
But amazingly, 90 days went by without a single neurological symptom.
How is it that an elderly person on a blood thinner who fell and hit his head never developed a chronic subdural hematoma?
I asked this to Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
Dr. Park explains, “It’s always better to be lucky than good. The mechanism of injury is very important.
“If the injury was just local and didn’t involve the sudden acceleration/deceleration, there may not be a breaking of veins and resulting in SDH.”
There is also the possibility that my father does not have a lot of the age related brain shrinkage (atrophy) that many elderly people have, which puts them at risk for a brain bleed.
Two ways to help stave off the so-called age related brain atrophy is to use the brain a lot (which he has always done) and exercise (he’s been doing upper body exercise for years and keeping busy with household projects).
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/pathdoc
How Big must Chronic Subdural Hematoma Be to Cause Symptoms?

How many millimeters–how big–must a chronic subdural hematoma be before it begins producing symptoms?
After all, if a brain bleed beneath the dura mater is small enough, it won’t cause any symptoms.
I posed this question to Charles Park, MD, neurological surgeon, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
Dr. Park explains, “Usual rule of thumb is 10 mm.”
My mother had a chronic subdural hematoma after falling and hitting her head.
The symptoms started up, suddenly, six weeks after the accident. The CT scan revealed two bleeds: One was 15 mm and one was four mm.
Only the 15 mm collection was drained. The neurosurgeon said that the tiny collection would be reabsorbed by her body.
After the surgery, my mother’s symptoms were gone (headache and bilateral leg weakness).
Dr. Park continues, “Also, what is important is whether the [chronic] subdural hematoma will produce a ‘midline’ shift, which means that the brain is shifted to the opposite side.
“This will be a more reliable indicator for the seriousness of the SDH and a determining factor in deciding on surgery.”
On my mother’s CT scan, I clearly saw the midline shift.
Because chronic subdural hematomas that are less than 10 mm, and certainly smaller than five mm, will typically not cause symptoms, we can say that there are people who develop a chronic subdural hematoma and never know it.
These are small collections under 10 mm — and more likely under five mm—that don’t produce any symptoms and are simply reabsorbed into the body.
How are these tiny subdural hematomas even discovered in the first place?
These small collections may be discovered incidentally when the patient undergoes a head CT for another reason that coincides with the timeline of the chronic subdural hematoma.
Or, they may be detected when the CT scan is performed because the patient is exhibiting symptoms from a larger cSDH that accompanies the tiny one.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Chronic Subdural Hematoma Symptoms Come & Go?

If your neurological symptoms like headache come and go, does this rule out a chronic subdural hematoma?
Let’s say you get hit in the head really hard but don’t experience any immediate neurological symptoms such as loss of consciousness, confusion or an immediate headache that worsens.
In fact, you feel fine other than the feeling that you just hit your head really hard.
You may even go to the ER to have a CT scan just in case there’s bleeding in your brain. Everything checks out normal and life goes on.
But you know all about chronic subdural hematoma—enough to worry you that in the next 90 days, there’s a possibility (especially if you’re over 65) that you’ll begin experiencing neurological symptoms due to slow bleeding in the brain over time (chronic) that was set in motion by the strike to your head weeks before.
You get a headache a week later and begin wondering, “Is this it?” But the headache never gets beyond a level 3 on a pain scale of zero to 10, and next day it’s gone.
You figure, If that was a chronic subdural hematoma, it would not have gone away.
Several days later you have another mild headache, and this time it lasts only that day.
A few days later another little headache occurs, and again, it’s temporary. (There are no other symptoms.)
And chances are pretty high that these minor headaches are not from any bleeding in your brain, but from the traumatized nerves outside of your skull, in your scalp, that took a good bang when you hit your head.
But still, you wonder:
Would the symptoms of a chronic subdural hematoma necessarily be ongoing and persistent rather than come and go?
After all, the bleeding doesn’t come and go. There’s either bleeding or there’s not.
If it’s there and causing symptoms…the symptoms will necessarily persist until the blood is surgically drained, right?
I asked Charles Park, MD, a neurological surgeon, if the symptoms of a chronic subdural hematoma can come and go.
He replied: “This is very true.” He is Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
Now realize that this article refers to chronic subdural hematoma, rather than the acute type (which is immediately life-threatening and can cause more dramatic symptoms such as projectile vomiting and stupor within hours, even minutes, of the trauma).
Dr. Park continues, “Once the cSDH develops, it will form a set of fibrous membranes to compartmentalize the cSDH.
“However, these membranes also have blood supply and it can bleed as well, adding to the cSDH already present.
“So, the symptoms can come and go as the size of subdural hematoma is gradually and incrementally increasing.”
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dragana Gordic
Hit Head; Should You Avoid Impact Cardio to Prevent Brain Bleed?

Wondering if after hitting your head you should avoid impact exercise like running or box jumping to prevent a brain bleed?
After all, the jarring and shaking of such activity might induce bleeding in the brain if the tiny veins have already been shaken up by a strike to the head — or so it seems.
Running, jumping and similar impact exercise cause jarring to the body. The head is not excluded from some of this jarring.
If you recently got hit good in the head, you may be fearing the possibility of triggering a slow bleeding in the brain called a chronic subdural hematoma.
If you know anything about chronic subdural hematoma, you know that it’s usually caused by getting hit in the head.
The trauma shears the tiny veins in the brain. It’s understandable if you can’t help but wonder if impact exercise can accelerate leaking of blood from the veins.
“Anything that has a violent acceleration/deceleration could increase the chance of developing subdural hematoma,” says Charles Park, MD, neurological surgeon, and Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
“But in general, just running or jumping, really should not cause the bleeding.”
So if you, for instance, slipped on ice and fell backward, striking your head on the pavement, but got right back up and had no neurological symptoms, you can go running or do your jump rope or stool jumping exercises — as long as you feel perfectly fine.
Certainly, avoid these if you have any kind of neurological symptom, and instead head to the emergency room.
But again, if you feel fine, then you can do your exercises.
But you should make a point to avoid anything that puts you in a potential position of falling and hitting your head a second time — just in case you’re vulnerable to a chronic subdural hematoma.
You really don’t know with absolute certainty if you’ll go on to develop a chronic subdural hematoma or not in the 90 days following getting hit in the head.
However, if you’re younger than 60, chances are pretty small that developing one of these slow brain bleeds will ever happen.
But these brain bleeds can indeed occur in people younger than 60.
Thus, you should not feel invincible regarding a slower brain bleed just because you’re not “old.”
So during that 90 day grace period, it would be wise to avoid activities that could result in head trauma, such as horseback riding, skiing, boxing and ice skating.
But feel free to resume your running, step aerobics and plyometric (jumping) drills, as these will not spur on any subdural bleeding.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vadim Martynenko
Hit Head? Avoid Fish Oil & Garlic to Prevent Brain Bleed?
If you get hit in the head hard, should you avoid natural blood thinners like fish oil and garlic to prevent a chronic subdural hematoma?
I posed this very interesting question to a neurological surgeon, because it made sense to me that someone’s brain could be (for lack of a better phrase), on the fence about eventually suffering a chronic subdural hematoma.
Or maybe they are destined to develop a chronic subdural hematoma—but one so tiny that it never produces symptoms and is naturally reabsorbed by the body’s healing process.
However, what if this individual has been taking natural blood thinners, namely, omega-3 fish oil supplements and garlic?

Might these be variables that would make what could be only a five-millimeter brain bleed turn into a 15 mm collection?
Or perhaps the fish oil and garlic might cause the chronic subdural hematoma where, if this person was NOT taking natural blood thinners, would never develop the bleed.
Let us assume that in this hypothetical scenario, the person who gets hit in the head does not experience any neurological symptoms of concern at the time of injury, such as altered consciousness, loss of consciousness, nausea or visual disturbances.
Specific research on this does not exist, but here is what Charles Park, MD, explains:
“In my opinion, it will be good to avoid anything that might increase the odds of bleeding, such as any chemical blood thinners or natural blood thinners.”
Dr. Park is Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
He adds: “Even though there are no neuro symptoms, there maybe some injury to the brain, which is susceptible to further bleeding.”
So if you get hit in the head really hard, and normally take fish oil supplements or garlic supplements, play it safe by avoiding these.
Since a chronic subdural hematoma can occur up to 90 days following trauma to the head, this is the length of time you should avoid the supplements.
And it goes without saying, avoid aspirin. If you’ve been instructed by your doctor, however, to take a daily aspirin for heart health, make sure the prescribing doctor knows of your head trauma.
Don’t quit the aspirin without being evaluated by your doctor.
Discontinuing it without medical guidance can increase your risk of the conditions it’s been prescribed for, or lead to unintended health consequences.
Your doctor will evaluate your current health status, review your risk factors and determine whether continuing or stopping aspirin is appropriate for you if you’ve recently hit your head hard.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He is skilled in advanced procedures and techniques that utilize innovative computer technology and image guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cyber security topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cyber security topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She is also a former ACE-certified personal trainer.
.
Top image: Shutterstock/G-Stock Studio
Young People, Chronic Subdural Hematoma but No Headache?

In younger adults, how common is it that a chronic subdural hematoma would not cause a headache?
A subdural hematoma is bleeding under the dura mater of the brain. This can begin happening several weeks to a few months after the head trauma — at which point symptoms would begin appearing.
Younger people with a chronic subdural hematoma are much more likely than elderly people to experience a headache from this condition.
This is because the younger brain has not shrunken, and thus, the space between the brain and the dura mater is very tight.
If bleeding begins occurring between this very confined space, it will create a pressure that usually results in a very bad headache.
This space is a lot bigger when the brain is shrunken (atrophied) —which usually occurs with the elderly brain.
Headache and Chronic Subdural Hematoma
“In young people, the chronic subdural hematoma is usually caused by some kind of traumatic injury to the brain,” explains Charles Park, MD, Director of The Minimally Invasive Brain and Spine Center at Mercy Medical Center in Baltimore.
Dr. Park continues, “The extent of the injury can be a mild concussion to severe contusion and bleeding into the brain and outside the brain.
“Headache is the most common symptom, but others, such as nausea/vomiting, cognitive impairment, slurred speech, visual disturbance are expected as well in that order of increasing severity.”
Summary
Headaches most commonly occur in younger people as a symptom of a chronic subdural hematoma. But younger adults can still experience other symptoms.
And likewise, an elderly person with this condition may suffer a searing headache despite more space between the aged brain and the dura mater.
The percentage of people under age 60 who have a headache resulting from a chronic subdural hematoma is estimated to be up to 80 percent.
The key words are “up to.” Data on this percentage is not exact. We cannot say, for instance, that 80 percent have headaches.
Usually, the percentage is a range that starts under 50 percent and goes up to 80.
Dr. Park specializes in minimally invasive surgical techniques for treatment of conditions affecting the brain and spine. He’s skilled in advanced procedures and techniques that utilize innovative computer technology and image-guided surgery systems.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com drobotdean
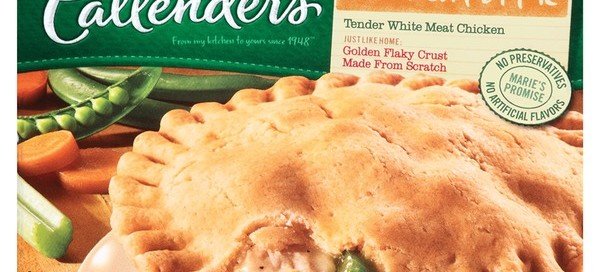
Marie Callender’s Chicken Pot Pie Has TRANS FATS!
What you can’t see CAN hurt you: trans fats.
Do not buy Marie Callender’s chicken pot pies if you don’t want artery-clogging trans fats that are linked to up to 27,000 heart disease deaths every year in the U.S.
It’s BS that Marie Callender’s trans fatty chicken pot pies are made from scratch, as the company’s TV commercial implies by the aproned actress rolling dough with a pin.
These heart disease pies are made one at a time by someone’s granny in a sunny kitchen with just a handful of ingredients. NOT!
Never mind that one whole Marie Callender’s chicken pot pie contains 1,040 calories and 1,600 mg of sodium (the package lists half these values because the indicated “serving size” is HALF the pie).
- If you don’t gain body fat easily you may not care about the calories.
- If your blood pressure is always normal you may not worry about an occasional sodium tsunami.
But if you want to avoid heart disease and heart attacks, then the partially hydrogenated soybean oil in Marie Callender’s chicken pot pie should be the deal breaker.
Any partially hydrogenated fat or oil is a trans fat—and this one element is all you need for the deal breaker.
“Trans fats are man-made fats and they are commonly used in processed foods to improve the texture, flavor and shelf life of the product,” says Prajakta Apte, RDN, owner and founder of Right Nutrition Works who helps people create a healthier lifestyle.
“Many studies have confirmed that trans fats can increase a person’s risk for cardiovascular disease, stroke and systemic inflammation.”
According to the Centers for Disease Control, trans fats increase the “bad” cholesterol and may lower the “good” cholesterol.
Marie Callender’s pot pies are NOT made from scratch.
They are made assembly line style in a factory and with the toxic trans fats—in a way that would have Grandma turning over in her grave.
The Marie Callender’s site says that this product has “HOMEMADE TASTE.”
There is a big difference between homemade taste and homemade ingredients. This “homemade taste” thing is the company’s way of playing tricks on the consumer’s mind.
In the 1940’s Marie Callender began baking her pies — from scratch.
The company has grown massively since. There is NO way that each modern-day pie is carefully made from scratch — unless the company has a few million robots somewhere doing this.
Grandma needs only about a dozen ingredients to make a chicken pot pie from scratch.
Whereas the Marie Callender’s product contains dozens of ingredients including the heart poisonous trans fats and another heart harming substance, interesterified soybean oil. I bet Grandma can’t even pronounce that.
 Prajakta Apte is the author of the eBook “Overcoming Nutrition Roadblocks.” Her personalized approach to nutrition therapies helps treat root causes of conditions such as type 2 diabetes, high cholesterol, GI disorders, hypertension and many more.
Prajakta Apte is the author of the eBook “Overcoming Nutrition Roadblocks.” Her personalized approach to nutrition therapies helps treat root causes of conditions such as type 2 diabetes, high cholesterol, GI disorders, hypertension and many more.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: mariecallenders.com/
Causes of PVC’s after Lying Down at Bedtime
Can lying down to go to sleep actually cause premature ventricular contractions?
“Most people are more aware of their heartbeat after they lie down at night, thus triggering the perception, but not the reality, of an arrhythmia,” explains cardiologist Dr. Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
This phenomenon applies to both men and women. The act of lying down at bedtime — a situation of changing body position from upright — would not disturb the heart and brain’s cardiac rhythm headquarters.
However, something needs to be said about the possibility that the moment some men and women take to their bed, their mind gets flooded with stressful thoughts.
You’re lying there in the dark and quiet, perhaps alone: the perfect opportunity for all sorts of intrusions to barge into your head, such as next-day’s tasks or an unforgivable act committed by a family member.
It can be overwhelming, reflecting upon the anticipated next-day’s struggles or someone’s outrageous behavior.
What’s going on in your life?
The phone calls you must make next day?
The people you must speak to?
The tasks you didn’t get done today that will carry over to next day?
The bills you still didn’t pay?
Anxiety mounts as you lie there in bed, and anxiety can trigger premature ventricular contractions.
In fact, your BED can be a conditioned stimulus for anxiety (because that’s where you do most of your fretful ruminating) and hence — all those PVC’s.
What Should You Do?
- Try to retrain your mind to empty all of the stressful thoughts when your head hits the pillow.
- Put on a white noise machine to help distract you from anxiety-triggering thoughts.
- Limit or eliminate caffeine intake (a trigger for premature ventricular contractions) in the few hours prior to bedtime.

Dr. Marcovitz has 40+ years of experience in helping people improve their heart health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.