Causes, Remedies, to Severe Dizziness While Exercising

Do you know the many causes of severe dizziness during exercise?
“Exercise can trigger dizziness for number of reasons,” says Jacob Teitelbaum, MD, medical director of the Fibromyalgia and Fatigue Centers nationally, and author of “Beat Sugar Addition NOW!”
“These include, most often, dehydration and salt depletion.”
As a personal trainer I’ve had clients report dizziness during exercise.
These were clients who weren’t in the best of condition, though they didn’t have any known diseases. But at some point during the exercise session, they got dizzy. (more…)
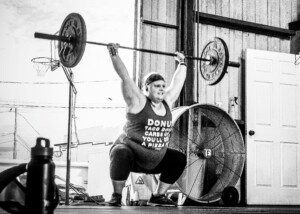
Do Small Women Need to Lift Only Light Weights?

What can a petite woman like 5-2, 105 lbs., gain by strength training with only light weights? (more…)
How Plus Size Women Can Stop a Gym Bully

Contrary to popular advice, the overweight woman who’s “bullied” at the gym SHOULD confront the “bully.” (more…)
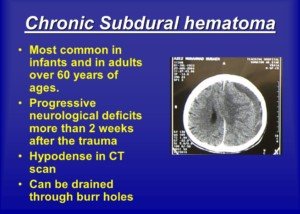
How Common Is Delirium in Elderly Hip Fracture Patients Postop?

Delirium in elderly hip fracture patients after surgery is so common, don’t be surprised if your senior age mother suffers from this after the operation. (more…)
Most Likely Causes of Tingling Head, Feeling Faint

Is that tingling in your head and faint feeling happening to you again?
“There can be many causes,” says Carolyn Dean, MD, ND – Medical Advisory Board Member, Nutritional Magnesium Association at nutritionalmagnesium.org.
According to Dr. Dean, here are the most likely causes of feeling faint and having a tingling sensation in your head: (more…)
Can Excessive Sitting Clog Your Heart’s Arteries?

Uh oh, if you sit a lot…this can actually lead to clogged coronary arteries. (more…)
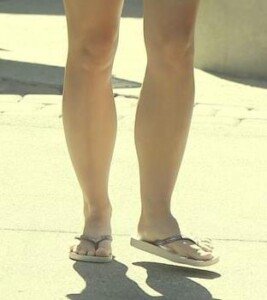
Got Cankles? Where They Come From & How to Get Rid Of
Cankles — is there any hope for those who suffer from these?
In some cases of cankles, there’s actually some hope. The word cankles is a fusion of “calf” and “ankles.” (more…)
Can You Get Ripped Doing ONLY Bodyweight Exercises ?
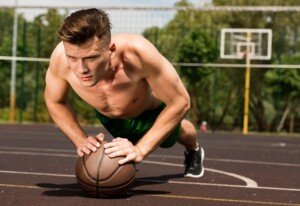
If all you do are bodyweight exercises like pushups, dips, pull-ups, jumping), then YES, you can get a ripped physique.
And I mean really ripped if you apply the very important element of HARD WORK + the right eating habits.
(more…)
Overweight & New to the Gym? Best Exercises for Losing Fat

Overweight, even very fat, people CAN lose a LOT of weight once they start doing specific exercises at the gym that will melt off pounds. (more…)
Which Gym Machine Is Best for Flattening the Stomach ?

One machine stands out for shrinking fat stomach.
All the time people used to ask me when I was a personal trainer at a gym, “What machine will get rid of this?” as they then grabbed ahold of their fat stomach.
I told that there is one machine that beats out all other machines for ridding abdominal fat.
It is the legs! Yes, the legs. Think of your legs as a powerful machine or tool for melting fat.
Your legs are one powerful machine. And this human machine will get rid of stomach fat — when you know which exercises to perform.
So, the truth then is, there is no abdominal gym “machine” that will slash belly fat. But other gym machines will do this: machines that involve your legs!
Leg routines that will knock off stomach fat are: 1) high intensity interval training, and 2) plyometrics.
High intensity interval training (HIIT) may very well be the most effective way to burn fat — according to much research (e.g., Talanian et al).
HIIT involves very brief, but very intense, bursts of all-out-effort pedaling, sprinting, stepping, hill dashing, hill walking, staircase dashing, etc., alternating with just 1-3 minutes of casual pacing, done over a 20 minute (or longer) period, so that ideally, you complete eight “work intervals.”

Shutterstock/Razoomanet
HIIT causes hormonal changes in the body that result in accelerated fat-burning that lasts for many hours after your workout, and this will help get rid of stomach fat.
Plyometrics refers to jumping drills: on an exercise box, leaping, jump lunges, pike jumps, squat jumps, etc.

Jumping explosively for 30 seconds is a form of HIIT, except that it’s more weight-bearing than, for example, running on a track or pedaling super hard on a bike.
There’s a weight training component to plyometrics, in that you are hoisting off the floor your bodyweight.
Leg routines with machines that will rid abdominal fat: 1) squats, 2) deadlifts, 3) leg presses.
Squats can be done with a free barbell, a Smith machine or by holding dumbbells. Squats engage the lower body plus the core, and when done intensely, will burn up a lot of pudge.

I had my clients doing intense squats and I saw their stomachs get smaller. I had them doing isolated abdominal exercises only for five minutes out of an hour training session.
Deadlifts. Anyone who’s ever done intense deadlifts knows that this movement engages the entire body.

Shutterstock/MilanMarkovic78
After completing an exhausting set of deadlifts, many trainees can’t pinpoint which part of their body gets hit the hardest, or what precisely makes them unable to complete another rep, because the entire body gets socked.
Intense deadlifts will burn significant amounts of fat, including abdominal.
Leg presses are best performed on the floor machine, as this more easily allows a deep range of motion.

Shutterstock/Motortion Films
Like squats and deadlifts, the leg press is a multi-joint action. Multi-joint routines burn more calories, and the more fat burned, the smaller that your stomach will get.
In conclusion, there is no abdominal machine that truly “gets rid of” belly fat, though ab equipment is great for strengthening the ab muscles and making them more toned.
But, that layer of fat between the ab muscles and the skin will not budge simply from using an abdominal machine!
The best machine for getting rid of the fat in your stomach is that of your very own body: the legs (and butt), which will be highly engaged through HIIT and multi-joint lower body routines.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.