
Have You Banged or Hit Your Head Really Hard Lately and Are Wondering If You Should Visit the ER?
Getting hit hard in the head isn’t pretty, and sometimes an ER visit is warranted.
Sometimes it’s a no-brainer that a visit to the emergency room is in order after one hits or bangs their head, if the ensuing symptoms are beckoning for medical attention.
But what if the symptoms are more subtle and the hit on the head doesn’t seem that bad?
When to Go to the ER
“Head injuries are very common and the vast majority are not serious,” begins Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
“In the majority of people the skull is tough and prevents most trauma from causing brain injury.
“Young children, those on anticoagulants, the elderly and those with osteoporosis are exceptions to this rule.
“Having said that, head injuries are one of the major causes of death in young people. About 0.2% of people attending ER with a head injury die.”
Dr. Beatty provides 12 symptoms to look out for if you get hit in the head.
1) Severe or worsening headache
2) Vomiting
3) Confusion or drowsiness
4) Loss of consciousness
5) Convulsions
6) Visual disturbance such as double vision or loss of some of your visual field
7) Weakness or loss of power in a limb or a drooping on one side of the mouth
8) Clear fluid or bloody discharge from the nose or ears
9) If you take anticoagulants (blood thinners)
10) If there has clearly been a dangerous impact such as a high speed RTA or a fall from a great height
11) Memory loss
12) Any suspicion of non-accident injury
Hard Impact but No Symptoms
What if the impact to the head was really, really hard, but there weren’t notable physical symptoms immediately after?
Some trauma centers have used the criterion of whether or not there was an alteration of consciousness such as asking the same question over and over.
Nevertheless, a person with only one of the aforementioned symptoms may indeed have an intracranial bleed or subdural hematoma.
An ER physician may order a CT scan if the patient has only a headache, especially if it’s getting worse.
What if there’s a big bump or bruise — but no symptoms?
“After any significant bump on the head it’s good practice for the person to stay with a relative or friend for 24 hours after the injury — then if there’s a deterioration, further help can be called,” says Dr. Beatty.
“They should rest, avoid alcohol, avoid sedative drugs, avoid contact sports and avoid driving.
“The size of the bruise gives some measure of the severity of the impact and is certainly taken into account in infants.
“In adults it’s probably less useful as an indicator than the other factors listed above.”
CT Scan of the Head
“Most hospitals will have guidelines/protocols for which patient warrants a CT scan and which doesn’t,” says Dr. Beatty.
“If they are seeing the subdural patient on a good day they may not tick the right boxes to get the test done.
“The guidelines as to when a CT scan is needed will vary from region to region, but most of the above will warrant a CT scan.
“There may be specific guidelines such as more than one vomit or more than five minutes of memory loss.
“The assessment of confusion or drowsiness may involve assessment using a scale such as the Glasgow Coma Scale (GCS).
“This gives scores for eye opening, verbal response and motor response.
“A normal person would score 15 and a totally comatose person would score 0.
“The lower the GCS score the more appropriate it is to do a CT scan.”
Bleeding in the Brain
“After serious head trauma a rapid deterioration in the first few hours is usually caused by a bleed into the substance of the brain: an intra-cerebral hemorrhage,” explains Dr. Beatty.
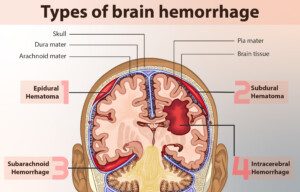
myupchar. comen
“These can bleed profusely, causing pressure and damage within the brain, usually leading to obvious symptoms. It’s easy to spot that things aren’t right.
“Relatively minor trauma can lead to a subdural hematoma when blood collects between the bones of the skull and the substance of the brain.
“The amount of blood may vary from very little to a great deal.
“Small subdurals may not cause many (or any) symptoms. They may cause obvious neurological symptoms with limb weakness.
“They can, however, cause more subtle symptoms which are less likely to be picked up by the doctor or the patient.
“The onset is often more gradual [a “chronic” subdural hematoma] — and the symptoms may fluctuate.”
For example the person may be normal one day but have confusion or memory loss the next.
A chronic subdural hematoma may also present with personality change, speech issues or drowsiness.
“A chronic subdural can grumble on for days or weeks before being diagnosed.
“Those on blood thinners and the elderly are more susceptible.
“If the elderly person doesn’t have normal cognitive function to begin with, it may be very difficult to pick up subtle changes in memory or mental ability caused by a subdural.”
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.


























