Preparing for a Strenuous Hike: Be Ready, Not Hurting

Fearing you won’t last on that upcoming grueling hike?
This smart routine will prepare your body for handling the hills with grace. (more…)
Locking Elbows Out During Bench Press: Pros & Cons

What are the advantages, if any, to locking out the elbows for the bench press?
Can this even cause an injury to the elbow joint?
For best results, you should not completely lock out the elbows for a bench press. (more…)
Can You Get Big Shoulders from Lifting Light Weights ?
For big shoulders, does it really come down to heavy weights with impaired range of motion or light weights with full ROM?
Can you build big shoulder muscles with light weights? It may seem intuitive that using heavy weights is the best way to build big shoulder muscles.
But the problem with heavy weights is that, depending on the routine, they will disrupt range of motion and may encourage cheating, thereby ultimately shortchanging your shoulder muscles – and preventing the growth you seek.
On the other hand, you don’t want to use weight loads that are too light, either.
“In order for hypertrophy (muscle development) to occur in a muscle group, that muscle group must be trained with basic overload principles,” says Juliet Deane, Elitefts staff member, Elitefts-sponsored figure athlete, personal trainer (NSCA) and co-owner of The Training Studio, NJ.
She continues, “The shoulders need to be trained to stimulate muscle growth by stressing the area with mid-volume rep ranges from 8-15 with challenging weights to complete the set.
“Studies show that reps six and below do not significantly increase muscle size, but with reps of 8-15, depending on your supportive nutrition, is the range you can expect to get the greatest results.

Shutterstock/Artem Furman
“Reps above that will elicit a muscular conditioning response, which also does not greatly affect hypertrophy.”
There is something very important to consider here.
If you choose a weight and simply count out reps to between eight and 15, then set the weights down, this doesn’t mean you’re working out in a way that maximizes growing big shoulder muscles.
That rep range of 8-15 must be very difficult to complete.
You can’t just go through the motions with a little elbow grease and expect to build your shoulder muscles.
The entire set must be stressful, and the last rep (be it the eighth, tenth or fifteenth) must take all you have to complete it.
And at the conclusion, your shoulders should be crying.
Deane explains, “The actual weight of the dumbbells is irrelevant, and light is a relative term or even a matter of opinion.
“What counts is if the weight is challenging for you. If the weights feel light, you are not likely going to stimulate the muscles enough in the optimum muscle building rep ranges; in effect, not producing the results of bigger shoulders you are looking for.”
Many other variables are at play when it comes to building big shoulders.
The shoulder muscles consist of three heads: front, middle and back.
All three heads must be worked, and there are many ways to do this.
Some people swear by upright rows, though these are very uncomfortable for some folks as well.
Another favorite is the lateral or side lift with dumbbells.
However, if the weight is too heavy, your form will suffer enough to impede shoulder muscle growth, even though it may seem like you have “completed” your eight or 10 reps.
A classic shoulder building routine is the barbell military press. Pulley systems are also popular.
At the end of your shoulder routine, these muscles should be burning mad, from front to back.
If you can barely lift your arms later on that day, you did a good job.
Make sure you support your workouts with a protein-rich, high-carb meal within 45 minutes after.
 Juliet Deane is also certified as a Russian kettlebell instructor and USAW Olympic lifting coach.
Juliet Deane is also certified as a Russian kettlebell instructor and USAW Olympic lifting coach.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ sozon
How to Make Lunges Count As Cardio
Lunges CAN count as a cardio workout — if you know how to make them do so.
As a former personal trainer, I would tell my clients that the rule of thumb, when determining if an exercise is cardio vs. strength training, is how long the movement can be sustained for. (more…)
Do Halfway Pull-ups and Chin-ups Count As Real?

What is it about the pull-up or chin-up that encourages so many gym-goers to go only halfway? (more…)
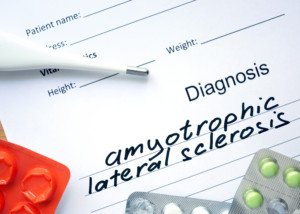
Muscle Twitching: Causes and Solutions

A physician explains what causes fasciculations and how to curb them.
Everyone experiences twitching muscles. Any voluntary muscle is capable of twitching.
This includes the eyelid, right above the lip, behind the ears, and of course, the larger muscles, including those located in the back, abdomen and limbs.
Fingers and toes may twitch from time to time as well. In fact, when digits twitch, it’s common to be able to actually see them in twitching motion.
Often, other muscles that twitch can also be seen twitching, including muscles on the top of the hand. In short, muscles, by nature, twitch.
For exercise enthusiasts, the most common sites of muscle twitching are the calves, arches of the feet, quads, hamstrings and glutes.
However, upper-body muscles also commonly twitch, such as biceps after performing pull-ups or grueling biceps curls; or chest muscles after bench pressing, pushups or some other rigorous chest routine.
Exercise is one of the most, if not the most, common causes of muscle twitching.
However, the twitching normally does not occur during exercise.
Sometimes, it occurs immediately following weight-bearing routines, such as pull-ups.
On the other hand, twitching may not start until the person finally comes to a complete rest at home. Cardio exercise can also induce twitching.

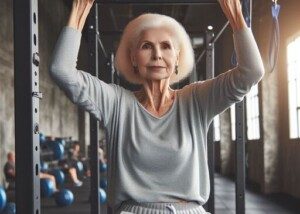
Shutterstock/ G-Stock Studio
The medical term for muscle twitching is fasciculations, or fascics for short.
- Ranking at perhaps No. 2 on the list of causes for fasciculations is anxiety.
Yes, muscles will often jump around a bit when you’re flanked with stress and anxiety.
- Another cause is dehydration, though you may not be particularly thirsty.
- Lastly, inadequate intake of calcium and magnesium is a classic cause of fasciculations.
Muscle twitching, to some people, feels good, kind of like internal massaging.
But to other individuals, fasciculations can be annoying, especially if the twitching rate is coming in at about one fasciculation per minute.
Some people experience several fasciculations per minute, for hours on end, even all day long.
Individuals have described the sensation as “worms crawling under the skin,” or “thumping.” One particular area of the body may twitch a lot: a “hot spot” for fasciculations.
Common hot spots are calves and arches, because calves really do quite a bit of work from day to day, and our feet take a good beating on a regular basis.

Shutterstock/Denis Val
Sometimes, twitches are body-wide. Interestingly, if a person starts worrying about the twitching, he or she will start twitching more.
In fact, many people who first start experiencing fasciculations in one body part, such as the feet, will then report that the twitching “quickly spread” throughout their entire body – only after they began worrying about it or focusing on it with too much wonder.
But are fasciculations something to worry about in the first place?
If fasciculations become annoying, you may become concerned that the twitching signals some kind of medical ailment.
This is akin to automatically concluding that an upset stomach means colon cancer.
However, in the case of a medical condition, the twitching is always accompanied by other symptoms of that condition.
In other words, there is no illness that is characterized by just twitching.
When anxiety about fasciculations accompanies the twitching, other symptoms often appear: muscle cramping, some tingling, and what seems to be weakness. All three of these symptoms are caused by the anxiety.
Yes, muscle weakness in this case is imagined. This is called “perceived weakness.”
But if anxiety is severe enough, muscles really can lose their efficacy. A classic example is when a person is under extreme duress, and can barely walk due to “buckling” legs.
Once the person begins lifting, running or hiking (and we all know how effective vigorous exercise is at eradicating anxiety), the perceived weakness typically disappears into thin air.
Notable muscle twitching is referred to as benign fasciculation syndrome, or BFS.
BFS is a fancy way of saying that someone has twitching muscles, usually accompanied by cramping or tingling.
The cramping often comes from tension in the muscles, sometimes from fasciculations; and tension from stress.
Muscle twitching in and of itself does not cause tingling. But worrying about the twitching can, since stress causes constriction of blood vessels in extremities, thereby reducing blood flow there!
Certainly, all athletes will get fasciculations sooner or later. After a rigorous hike or trail run, for example, a person will eventually settle down and relax, legs immobile.
Soon after, his or her legs begin twitching like mad. Movement ceases the twitching. But once inertia resumes, fasciculations resume.
Just what causes the twitching in the first place?
“Above all, fatigue is the reason for the muscle twitching,” explains Kevin Plancher, MD, a leading sports orthopaedist and sports medicine expert in the New York metropolitan area.
“The muscles are most likely overworked at this point. The nerves that send impulses to the muscles become fatigued as well, which can cause erratic firing of the muscles.”
Long exercise sessions cause lactic acid to build up, resulting in a lack of oxygen. Dr. Plancher says, “This alters the way the muscles contract as well, possibly causing twitching.”
As mentioned earlier, cramping can be brought on by stress. But it can also be caused by an electrolyte imbalance in the athlete. “In order for a muscle to contract, electrolytes play a key role,” says Dr. Plancher.
Cramping and twitching can result from increased amounts of sweating that follow exercise, he says.
Also, cramping – or what the athlete describes as such – can simply be caused by an over-worked or over-stretched muscle.
Fasciculations shouldn’t be a nuisance, once you realize that they are a normal part of muscle physiology. But there are ways to manage fasciculations, for those who don’t like the sensation.
Dr. Plancher says, “Movement is a very good way to minimize the twitching. It helps the body move the excess lactic acid out of the muscles.
Secondly, it allows the electrolyte levels in the muscles to normalize if they are unbalanced due to fatigue of the nervous system. Stretching the involved muscles will help as well.
This relaxes the muscles. Increasing fluid intake can be key to minimizing these episodes, especially if electrolyte imbalances are the culprit.”
Try a banana or an all-natural electrolyte beverage.
Dr. Plancher also suggests gradually working into an exercise session, rather than jumping in with too much, too soon.
“Do not overload in the beginning. You will see less adverse reactions with a progressive program.”
Finally, work on ways to reduce the anxiety in your life. Dr. Plancher explains that the muscles of an anxious person are often tight – as in too much tension.
“The muscles would be in a constant state of contraction that would overwork the muscle and cause fatigue just like in exercising muscles.”
If you’re having a hard time settling down, consider doing muscle-relaxing activities such as yoga and swimming.
Lastly, spend some time in a sauna for its detoxifying and calming effects.
 Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
Dr. Plancher is founder of Plancher Orthopaedics & Sports Medicine, and lectures globally on issues related to orthopedic procedures and sports injury management.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
,
Top image: Shutterstock/Syda Productions
Can Keppra Cause Excessive Weakness & Sleepiness?

Can the drug Keppra cause extreme weakness and sleepiness?
Keppra is an anti-seizure medication. It’s not just given to those with a chronic seizure disorder.
It’s also prescribed for people who are at risk for having a seizure due to head trauma, such as after hitting their head from a fall.
My mother was given Keppra while recuperating in the hospital after undergoing a burr hole procedure for a chronic subdural hematoma (cSDH) which had been caused by hitting her head in a fall.
She was admitted on a Sunday and released the following Thursday, quite feisty, alert and having no problems with her walking.
It’s common protocol to put a patient, having just undergone the burr hole procedure for cSDH, on some kind of anti-seizure drug, such as Keppra.
This is a precaution, since risk of seizures is elevated for about a month after such a procedure.
My mother was initially put on the anticonvulsant Dilantin, but at some point near the end of her stay was switched to Keppra.
The evening of her discharge she seemed well on her way to recovery and was walking about the house without a hitch, was alert and interactive.
The Keppra prescription was for 500 mg morning and evening.
She took the drug that evening — and next morning awakened complaining of dizziness and weakness: unsteady, lethargic, weak-looking gait.
Her presentation definitely looked medication-induced.
She was dizzy and unsteady all day, and this caused her to fall outside.
As the day progressed the symptoms worsened to the point where I began suspecting that the fall shook up the 4 mm cSDH that the neurosurgeon hadn’t drained because of its small size.
The burr hole procedure had been done only on a larger cSDH; he had left the 4 mm alone, believing it would resolve on its own.
But with my mother’s weakness and lethargy worsening, I thought that the fall might have aggravated the 4 mm leak.
I then gave her the night dose of Keppra. The weakness progressed.
I got ahold of the neurosurgeon and asked if this mysterious weakness could be from the Keppra. He doubted it but authorized me to stop giving it to her.
So here I’m thinking it’s the brain bleed aggravated by the fall.
But if the weakness is from the Keppra, my mother should be better next morning.
Next morning she was worse. She couldn’t walk and had to be pushed in a wheelchair.
She wasn’t all there mentally; was not able to address simple questions, and gave conflicting answers to questions about whether or not she had pain. Appetite was nonexistent.
She remained in her robe all day long, and for most of the day, slept, save for about one hour where she was watching TV and eating a little. But then right after, she went back to sleep in a chair.
Her voice was very feeble, requiring effort to speak. She was not conversational and had little interest in speaking to one of her out-of-state kids who called.
She couldn’t even interact with her husband, was very apathetic and seemed to be heading towards a stuporous state.
Could this extreme sleepiness, weakness and brain fog really be side effects of Keppra?
Or was that 4 mm brain bleed now triple in size?
“It’s well-recognized that Keppra can cause drowsiness or weakness,” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
“Some people find that their body gets used to Keppra after a week or two, and the side effects become less.
“If not, they should discuss the problem with their doctor.
“They shouldn’t drive or operate machinery if they don’t feel alert.”
Of course, there’s a huge difference between the typical drowsiness and weakness from a drug, and the more severe symptoms that my mother had been experiencing.
A cSDH can cause relatively sudden global body weakness, which was what my mother’s larger cSDH had caused.
I was witnessing a very similar symptom. A head injury can also cause sleepiness — but the tipoff that it’s more likely from an injury rather than a drug is that the symptom is progressive.
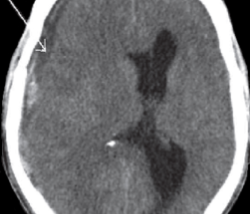
Another Head CAT Scan
I took my mother to the ER for another CAT scan, which turned out to show “improvement” over the one she had had at the hospital following the burr hole procedure, and the 4 mm bleed was gone!
The CAT scan showed no explanation for her severe weakness, lethargy, apathy, sleepiness and earlier-in-the day mental status change.
The ER doctor determined that my mother had sustained an adverse reaction to Keppra, and that it should wear off.
Though drowsiness and a fatigued feeling may be more common side effects, this drug — like so many pharmaceuticals — can uncommonly cause confusion or more severe symptoms in some individuals.
In fact, that evening in the ER, my mother began showing some improvement: better-sounding speech and was conversational. She was kept overnight for observation.
The day after she was much better, and the physical therapist didn’t detect any neurological deficits.
The ER doctor consulted with the neurosurgeon, analyzed the CAT scans and discharged my mother with a diagnosis of weakness caused by Keppra. She had been a complete zombie the day before.
Though some people tolerate Keppra quite well, my mother didn’t.
This doesn’t mean that Keppra can’t work wonders for other people.
But it does indeed mean that if you or someone you know experiences sudden deterioration in mobility, strength, mood, alertness, conversational skills and wakefulness, and that person was recently put on Keppra (or another drug), you should consider that it might be the medication and express this concern to the prescribing doctor.
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
.
Top image: Freepik.com Racool_studio-
How Many Melanomas Can You Get at the Same Time?

Unfortunately you can get a lot of melanomas at the same time, says Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology.
“Sadly there is no limit,” affirms Dr. Gordon. “Once you have had a melanoma, you are at a higher risk of having another.”
It’s been said that melanoma is rarely a singular event. But that typically pertains to the phenomenon of developing another tumor (or one being discovered) a few years or more after the first one was diagnosed.
But what about primary melanomas at the same time?
I once knew a man — the fitness director at a health club — who announced to us one day that he’d been diagnosed with melanoma.
He showed me three spots: two on his arm and one on his face. So he had at least three going on at the same time.
I do not know if they were individual primaries or if, for instance, the one on his face metastasized to the two on his arm.
Multiple melanomas occurring at the same time is not the same as several melanomas being discovered at the same time.
Certainly, if a tumor is discovered during an examination, a rigorous inspection of the patient’s entire body will ensue, where another malignant spot could be discovered…and another.
But that doesn’t mean that the development of these lesions doesn’t have some time in between them; it’s just that they were found and diagnosed at the same time.
It’s not possible to tell if, for instance, there’s only a few weeks vs. 18 months between the development into existence of the melanoma on a person’s arm and the one on his back; or how much time in development there is between the three on his back.
“This is why dermatologists often like to see patients much more often after a melanoma diagnosis,” says Dr. Gordon, who’s with Westlake Dermatology located in Austin, TX.
“Multiple melanomas at the same time often need to be genetically studied to determine if they are separate primary lesions or related (and thus considered metastatic).”
The image below shows many melanomas at the same time — but they are metastatic — having originated from a primary spot.

canceradvice.co.uk/melanoma/treatment/
A primary tumor is one that arises from the pigmented cells in a mole or develops in the absence of a mole.
A secondary tumor is one that develops elsewhere as a result of cancerous cells having migrated from the primary: a metastasis.
The metastasis or spread could occur at a distant site from the primary, such as on the leg, when the primary is on the chest or neck.
Or, the secondary could occur close to the primary, but in either case, it’s not possible to determine what the time passage is between when the primary first came into existence and when the secondary developed.
It’s not common—in fact it’s rare—that a person could be discovered to have dozens of melanomas at the same time.
There are exceptionally rare cases in which a patient was found to have hundreds of melanomas at the same time.

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Nasekomoe
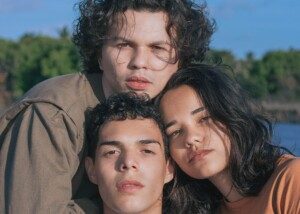
When Your White Daughter Has “Ethnic” or “Black” Hair

I grew up in a time when it wasn’t as acceptable, as it is today, for white girls to have ethnic-looking hair or hair that resembled that of biracial or black individuals.
Even today, unfortunately, some women cringe that their white daughters’ hair has ethnic attributes.
And I’m talking about fully white girls, not biracial or part Latina or Pacific Islander.
I am Caucasian (half Czech, half Lebanese), yet I am the only person in the immediate family and entire extended families on both parents’ sides, who has a very unusual texture of hair.
My Hair; Therefore It’s Natural, Regardless of Race
I have vague memories of my mother putting Brylcreem in my hair when I was a little girl. The stuff stank but she put it in to tame my fluffy and fuzzy hair.
Brylcreem back then was popular with men for slicking back their hair; my father used it.
Instead of relishing my fluffy and fuzzy hair, my mother hid it under Brylcreem.
There’s even a picture of me, at around age six, playing the piano…and you can see the glint of the Brylcreem on my short, smooshed-down hair.
What a travesty. As a young child, I didn’t know better. I didn’t know how to embrace and love my very unusual hair.
- It didn’t hang straight.
- It swelled up if not tied back.
- It flew and whipped all over the place in the slightest wind.
- It was considered “fine,” but there was a ton of it — and I mean a LOT.
If my hair was down and I had on a neon orange shirt, you would not be able to see any of the orange under my hair; my hair thickly fanned from shoulder to shoulder.
My mother also put my hair up in buns.
But voluminous, body-full “ethnic” hair should never be concealed with a bun!
Mothers of white girls with ethnic looking hair, take note:
There is NO shame in ethnic-looking, overly-fluffy, fuzzy and frizzy hair! This is your daughter’s genetic blueprint. It is HER hair.
HER HAIR! It’s her natural hair!
Why would you want to change it to look like everyone else’s? This is the way it’s supposed to be because (can’t say this enough) it’s her natural hair.
Do you not realize that “normal” hair begins looking really lousy once the hormones of perimenopause begin kicking in?
It thins and becomes limp. Come menopause, white women with typical hair have lost so much of it…all because they never had a good, solid foundation or base—or reserve or fund.
I had so much hair in my youth that, despite having experienced the inevitable diffuse hormonal hair loss, I still have a ton of it!
To Mothers Whose White Daughters Have “Ethnic” Hair
• Relish her hair; don’t hide it, don’t spray it down or smoosh it down with gels.
• There is NO such thing as the wrong hair for a white female; if she was born with a particular texture, that is HER hair, her natural texture; no race has a legal hold on any specific texture or look.
• It’s just as much her look as it is any other race’s — simply due to the fact it’s her genetic blueprint.
• Experiment with styles that the texture is especially conducive to, like high ponytails that generously billow out.
• Or just brush out the hair and let it hang, controlled with a few cleverly placed clips or bobby pins. Remember, if she was born with the fuzz and frizz…it’s the way her hair is SUPPOSED to look!
• Learn how to detangle the hair after a washing. I think the reason my mother kept my hair very short when I was very young was because she didn’t want to bother with the arduous task of detangling.
• Learn how to finger detangle. Experiment with different detangler serums. BE PATIENT. Never plan on detangling when you’re rushed.
• Straight, “white” and “normal” hair will not hold up to the hormones of perimenopause and menopause. Doesn’t stand a chance.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Lisa F. Young
Why Being Very Tall Can Help You Find the Perfect Husband