Breast Cancer Phobia, Obsessive Breast Checking: Solutions

Women who fear breast cancer so much that they “check” constantly & avoid mirrors & wear high collars to resist checking would benefit tremendously from more than just a negative clinical breast exam and a clean mammogram. (more…)
Why Isn’t Ultrasound Standard for Breast Cancer Screening?

If false positive rates of ultrasound screening cause anxiety & unnecessary biopsies, isn’t this worth the breast cancer it’ll catch that a mammogram misses, even if it’s just a handful of patients?
Ultrasound is frequently recommended after a mammogram reveals a suspicious mass.
An ultrasound can give additional information on a concerning mass that shows up on mammography.
Furthermore, women at high risk for breast cancer are sometimes encouraged to supplement the annual mammogram with a screening ultrasound.
So why isn’t it standard for screening?
“Ultrasound is not standard for breast cancer screenings,” says Dennis Citrin, MD, PhD, a board-certified medical oncologist who works with a team of experts to help patients fight breast cancer at City of Hope Chicago.
“Again, screenings are looking for the first signs of disease in a totally asymptomatic woman,” continues Dr. Citrin.
“With a mammogram, you are looking at the entire breast. If an ultrasound is used, it is typically after a woman has felt a lump and the ultrasound is used as a direct exam.
“The technician is looking at the exact spot that the patient and physician felt the lump, or the screening mammogram showed as a problem area.
“Some centers may use ultrasound more frequently, but it is not a screening tool. Additionally, in most hospital systems, a technician performs the ultrasound, not the physician.
“Ultrasounds are not cost effective, as they take up a lot of time and are very much a real time examination.”
If the millions of women every year who undergo a mammogram were to replace that procedure with a screening ultrasound of their breasts – in a parallel world where screening ultrasounds are the standard … there’d very likely be a medically unacceptable rate of false positives.
What initially happens in such cases is that a suspicious area shows up on the US.
This then causes untold anxiety, sleepless nights and possibly leads to an unnecessary biopsy that turns out negative.
This entire process can drag on for weeks, what with scheduling appointments for repeat (targeted) ultrasounds, the wait-and-see-if-it-grows approach and then finally the biopsy.
This scenario would likely play out many times in a world in which ultrasound screenings for breast cancer are the standard.
And those suspicious-looking but ultimately benign masses that are detected by ultrasound, in many cases, would not have been picked up by a mammogram – thus sparing many women prolonged anxiety.
The false positive rate for mammography is statistically significantly lower than it is for US.
The ultrasound can be too sensitive for the patient’s own good, which is why it’s not a standard screening tool for breast cancer.
US Has Its Place
However, it’s invaluable as a diagnostic undertaking following concerning mammogram results, or for women who have a high risk of breast cancer due to dense breasts, says a study (Berg et al) in a 2015 JNCI: Journal of the National Cancer Institute.
Furthermore, in women under 40 who have palpable breast lumps, ultrasound serves as a very effective diagnostic tool, says a study in American Journal of Roentgenology (2012).
“In women under 40, ultrasound is better at evaluating breast lumps compared to mammography,” says Constance Lehman, MD, in the AJR report.
“Mammography is still our best tool for screening women 40 and older, but targeted ultrasound is our tool of choice in evaluating symptomatic women under 40.”
A study in a 2015 Lancet (Ohuchi et al) acknowledges that previous studies have shown an unacceptably high false positive rate with US.
However, the Ohuchi study—which was carried out in Japan—showed only a small false positive rate that the authors believe could be even further reduced when ultrasound and mammogram results are analyzed together.
In America, mammograms remain the standard screening tool for women at average risk for breast cancer because they are more cost effective, have a lower false positive rate than does US, and because there’ve been no large-scale studies showing that ultrasound — as a screening tool for women at average risk of BC — saves more lives when compared to just mammography.
 Dennis Citrin, MD, is board certified in medical oncology with 30+ years’ experience, devotes his practice exclusively to patients with breast cancer and other high-risk breast conditions. He is the author of the book, “Knowledge is Power: What Every Woman Should Know About Breast Cancer.”
Dennis Citrin, MD, is board certified in medical oncology with 30+ years’ experience, devotes his practice exclusively to patients with breast cancer and other high-risk breast conditions. He is the author of the book, “Knowledge is Power: What Every Woman Should Know About Breast Cancer.”
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock, Magnito
Sources
sciencedaily.com/releases/2012/10/121022071723.htm
sciencedaily.com/releases/2015/11/151105010516.htm
sciencedaily.com/releases/2015/12/151228174405.htm
Living with LQTS 2: Cardiac Arrest Caused by Loud Noise
How on earth do people cope with the long QT syndrome type that can cause sudden cardiac death just from hearing a sudden loud sound? (more…)
Why Can’t LQTS Patients Play Sports if They Have an ICD?

Since an ICD shocks a fibrillating heart from long QT syndrome back into normal rhythm, why can’t people with ICDs play sports and work out? (more…)
Can Anxiety During an EKG Prolong the QT Interval?
If your focus of health anxiety is long QT syndrome, you should know that anxiety during an EKG can prolong the QT interval.
“Earlier studies have shown that anxiety states can cause prolongation of QT interval,” says Andrea Natale, MD, cardiac electrophysiologist and executive medical director of the Texas Cardiac Arrhythmia Institute at St. David’s Medical Center.
Medical tests that show an instant result — right there in the office — can leave a person who suffers from health anxiety literally trembling during the test.
Tests noted for an instant result include:
• EKG (of course! How long does it take for the nurse to hand the strip over to the doctor in the next room?)
• Clinical exam of moles
• Digital rectal exam
• Internal pelvic exam
• Clinical breast exam
Anxiety and QT Prolongation
As you already know, a state of anxiety will drive up the heart rate, and in some people, frequently cause “palpitations” or the sensation of delayed or skipped heartbeats.
So it really shouldn’t be a surprise that the QTc can be thrown off while the patient is lying on the exam table with 12 leads stuck onto their skin, knowing that all sorts of information about their heart will be collected in the next eight seconds.
A study that appears in Psychiatry and Clinical Neurosciences (2008) by Takimoto et al looked at the phenomenon of QT interval prolongation and people with eating disorders.
You may already know that anorexia nervosa and bulimia are often cited as risk factors for acquired long QT syndrome.
This is commonly believed to be due to electrolyte imbalances caused by the eating disorder.
However, abnormal QT intervals are also found in eating disorder patients who have normal electrolyte levels.
So obviously, something else is going on here. Takimoto et al discovered a correlation between the anxiety levels of these patients and their QT intervals.
The paper states, “In the present study, anxiety was also shown to be associated with QT interval and QT dispersion in BN patients.”
QT dispersion refers to maximum QT interval minus minimum QT interval, and BN refers to bulimia nervosa.
The paper continues, “It has been reported that anxiety can change autonomic control, and that anxiety influences the QT dispersion in hypertensive patients and normotensive subjects.”
This study result really needs to be taken with a grain of salt, because it triggers some compelling data:
• Anxiety over the actual EKG test is not the same as the more persistent anxiety that those with serious eating disorders experience.
• Not all of the patients in this study had abnormal QT intervals.
• In those with anorexia nervosa, shrunken heart tissue from malnutrition plays a bigger role in QT prolongation than does mood disturbance.
The study had limitations including the possibility that some of the participants were on medications even though the study called for patients not on any drugs; prescription drugs can prolong the QT interval.
Other variables that can influence QT interval such as magnesium and blood sugar levels were not measured.
So what to do?
Try to relax as much as possible during your next EKG. This is a hefty request for a person suffering from cardiac-related health anxiety.
But maybe you’ll feel more at ease if you consider some factors:
• If your doctor relies on the Bazett formula for computing QTc, know that this formula tends to overestimate the QTc the higher the heart rate during the EKG – and anxiety increases heart rate.
• The older you are, the less likely you have congenital long QT syndrome – assuming you’ve made it this far in life without any fainting episodes, let alone cardiac arrests.
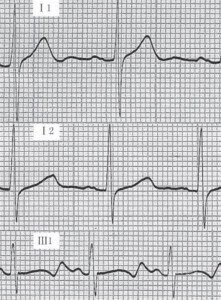
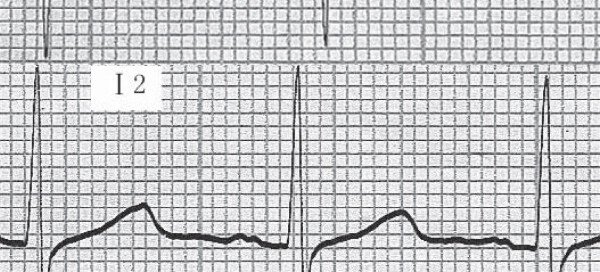
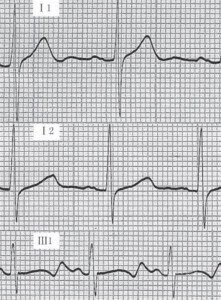
LQTS. Credit: Zhang et al.
• Remind yourself that things are looking good if no family or extended family members have ever suffered fainting episodes, cardiac arrests, sudden unexpected deaths or unexplained drownings – as these events are indicators of a familial congenital LQTS.
• Remind yourself that you are especially at exceptionally low risk for having congenital long QT syndrome if you’ve been exercising intensely for years without incident.
• The likelihood that you have acquired long QT syndrome is ridiculously low if you’re not on medications, don’t have anorexia or bulimia nervosa, don’t have low thyroid, heart disease or heart failure.
This all begs the question:
Can anxiety – either free-floating (ongoing for no apparent reason) or situational (due to intrusive thoughts or specific circumstances such as driving to work or having an EKG done) – actually cause acquired long QT syndrome?
Dr. Natale says that “brief anxiety during EKG is not a known risk factor for QT prolongation. QTc >500 ms is a known risk factor for LQTS.”
Dr. Natale’s greatest reward is restoring his patients to a life free of cardiac arrhythmia. He pioneered a circumferential ultrasound vein-ablation system to correct atrial fibrillation and performed the procedure on the world’s first five patients.
greatest reward is restoring his patients to a life free of cardiac arrhythmia. He pioneered a circumferential ultrasound vein-ablation system to correct atrial fibrillation and performed the procedure on the world’s first five patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Brian A Jackson
Source: on.linelibrary.wiley.com/doi/10.1111/j.1440-1819.2008.01753.x/pdf
How Fast Does Ovarian Cancer Grow from Stage 1 to 4?

Women whose medical plan mean delayed treatment for suspected stage 1 ovarian cancer fear that it’ll grow to stage 4 by the time surgery is performed.
Ovarian cancer is uncommonly discovered at stage 1. But there are cases when incidentally a concerning mass is detected when the patient is being imaged for an unrelated reason.
There is the case of a woman whose doctor suspected she might have an early ovarian cancer.
However, due to the patient’s slow-moving medical plan, the steps leading up to surgery—if further investigation pointed towards a malignancy—would take several months.
She was terrified that during all that time the confined tumor—if that’s indeed what she had—would spread to her organs.
How Long to Go from Stage 1 Ovarian Cancer to Stage 4?
“Ovarian cancer grows or spreads very quickly,” says Julian Schink, MD, Chief of Gynecologic Oncology, Cancer Treatment Centers of America; Medical Director of Gynecologic and Medical Oncology, Midwestern Regional Medical Center.
“In many cases it grows bigger and faster in the omentum [fatty layer that supports intestines and organs] than it does in the ovary or fallopian tube,” continues Dr. Schink.
“In my opinion some cases are stage 3 from the beginning because we sometimes see the pre-invasive (STIC) serous cells in a fallopian tube and a huge serous cancer in the omentum.”
There is no precise timeline identified for how long it takes stage 1 ovarian cancer to develop into stage 4.
If a woman’s initial diagnosis is stage 4, then nobody knows how far back she would have been diagnosed as stage 1.
If her initial diagnosis is stage 1…then the ovarian cancer is going to be treated, and hence, there’s no way to determine how long it would have taken to grow to a stage 4.
For more information on this disease or other gynecological malignancies, contact Cancer Treatment Centers of America at (844) 632-7188.
With 25+ years of experience, and board certified in gynecologic oncology and OB/GYN, Dr. Schink is dedicated to caring for patients and advancing treatments for gynecologic malignancies. His surgery and chemotherapy treatments include those for ovarian, cervical and uterine cancer.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Chinnapong
How Fast Can CIN 1 and 2 Turn into Cancer?

Even if your CIN 1 has turned to CIN 2, you’re still not near the cancer danger zone sitting at CIN 2.
This is because if we skip a step in the progression, meaning, look at the progression of CIN 3 to cervical cancer, we’re still looking at quite a bit of time. (more…)
Can Uterine Fibroids Turn into Cancer?

Learning that you have uterine fibroids can be quite alarming, because the first thought may be, “Can they turn into cancer?”
A fibroid itself is benign. When they become symptomatic this makes a woman a candidate for a hysterectomy. (more…)
How Do Dense Breasts Compare to Top Risks for Breast Cancer?
“Extremely” dense breasts have been noted in medical literature to be a significant risk for cancer, but what about compared to the biggest risk factors such as family history and BRCA? (more…)
Brief Sharp Stabbing Pain Under Breast: Benign or Cancer?