Can Sleep Apnea Be Sporadic Rather than Every Night?

Sleep apnea may not always occur every single night and in fact may be sporadic in some cases.
This can be referred to as intermittent sleep apnea, in which the intermittency is measured in days or weeks rather than hours in a single night. (more…)
Can Diabetes Cause Pain in Calf Muscles when Walking?

Diabetes can lead to dangerous conditions that cause pain in the calves and overall legs when walking.
Those with type 2 diabetes are particularly vulnerable to an arterial condition, though the risk is still increased by type 1 diabetes.
This condition is PAD: peripheral artery disease—also known as peripheral vascular disease. PAD is when there’s plaque buildup in the arteries of the legs.
This is the same plaque or “sludge” that builds up in coronary heart disease, causing the so-called blocked coronary arteries.
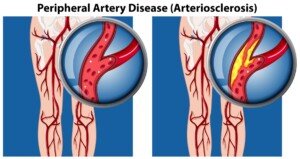
Source: vecteezy.com
There are three other conditions — related to diabetes — that can cause pain, aching or cramping in the calves — but first here is information on peripheral artery disease, which can get bad enough to cripple a person.
Diabetes and PAD
Diabetes is not required to develop PAD, but the presence of diabetes (especially type 2) raises the risk.
The reason diabetes increases the risk of peripheral artery disease, which causes pain when walking, is because diabetes causes a higher level of blood fats and raises blood pressure.
These situations can lead to arterial clogging with fatty deposits. The result is blocked, hardened and narrowed arteries in the legs.
“At rest there is no pain, but with activity, there isn’t enough blood flow to the muscles, so there is pain,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
PAD Causes Pain
The pain can be in the feet and toes, not just the calves and upper leg, and will be worse when walking and especially using a staircase.
However, PAD pain isn’t always constant. Sometimes it’s intermittent and is called intermittent claudication.
The discomfort can be in the form of a cramping type of sensation, or that of heaviness or fatigue.
PAD is no picnic. Peripheral artery disease can disable a person and lead to very slow-healing wounds (cuts, scrapes, etc.). The feet may become cold, too.
Ironically, PAD in some diabetics may not produce pain, mainly because the patient also has diabetic neuropathy, which reduces sensation in the legs and feet.
Peripheral artery disease in the diabetic or non-diabetic can also exist under the radar due to a gradual onset.
This gradual onset, or a subtle onset, can masquerade as “normal aging” to some individuals.
Their compensatory behaviors are to shorten the distances they walk (parking closer to store entrances, always using elevators and escalators, taking more sitting breaks when at the amusement park, etc.).
If the patient is older (e.g., 48 rather than 28), they’re likely to shrug this off as a case of “I’m not as young as I used to be.”
Another compensatory behavior is to walk more slowly. They are unaware they have PAD.
Even if they know they have diabetes, it may not occur to them that what’s happening is due to clogged arteries in the legs and calves.
Diabetic Neuropathy
As mentioned, this can reduce sensation and thus, blunt the pain of PAD. But diabetic neuropathy in and of itself can also cause pain.
You can have pain in your legs (although it usually causes pain in the feet),” says Dr. Besser.
If you have diabetic neuropathy this actually raises the risk of PAD. So it’s not just the diabetes that puts you at higher risk of clogged leg arteries, but the neuropathy, which is caused by chronic excess sugar in the body.
Deep Vein Thrombosis
A blood clot in a vein (DVT) can occur to anyone, but many risk factors abound, including diabetes.
A DVT classically presents with pain in a calf, including at rest. There may be associated swelling, redness and warmth to the area.
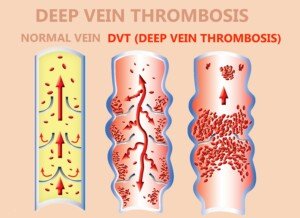
Shutterstock/Solarisys
A pulled calf muscle, however, typically feels fine at rest and is elicited only upon movement such as walking.
Electrolyte Imbalance
“If your diabetes isn’t controlled, your electrolytes (sodium and potassium) will probably not be normal; abnormal electrolytes can cause cramping,” explains Dr. Besser.
“Muscle strain is due to injury to the muscles (sprain/strain). This pain may also occur at rest if the strain is severe enough.
“There may also be tenderness in the affected muscle and it may be swollen.
“Rest, time and ibuprofen (or similar medications) will treat this but won’t help pain from diabetes related issues.”
Those with type 2 diabetes are particularly vulnerable to an arterial condition, though the risk is still increased by type 1 diabetes.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/TANAPAT LEK.JIW
Sources
diabetesselfmanagement.com/managing-diabetes/complications-prevention/diabetic-leg-pain-and-peripheral-arterial-disease/
thediabetescouncil.com/calf-pain-diabetes-connection/
If You Have Sleep Apnea but No Symptoms Do You Need CPAP?

Asymptomatic people with sleep apnea should use a CPAP—and they shouldn’t, too; the answer depends on more specific data as well as the doctor treating the patient. (more…)
How Fast Nodular Melanoma Goes from Flat to Pencil Eraser Height

If you wait for nodular melanoma to go from flat to pencil eraser height before seeing a doctor, you could be dead a short time later.
Nodular melanoma goes from zero to metastasis in zip speed.
But just what IS the time frame for how fast a nodular melanoma can grow from flat to the height of a pencil eraser?
“Nobody knows; they grow quickly,” says Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30-plus years’ experience.
“They can go from non-obvious to obvious in weeks to months.”
The reference to pencil eraser diameter is typically used for the guidelines of examining the skin for signs of melanoma or its risk factors.
Pencil eraser height is a whole new animal, and a killer one at that.
Nodular melanoma is so ruthless that you do NOT want to wait for it to reach the height of a pencil eraser or even one-eighth of that before seeking medical attention.

shutterstock/Leigh Prather
There is no stage zero phase for this kind of skin cancer. It doesn’t sit at an early stage for months on end as does the much more common superficial spreading melanoma.
In the superficial spreading type, it expands in diameter before it starts digging downward.
This can take a few years in some cases. The superficial spreading radial phase gives the patient plenty of time to catch it in a curable stage.
Nodular melanoma can spring out of nowhere and start growing vertically before it spreads laterally, fooling the patient into thinking that the tiny new bump on their skin is “nothing.”
It is commonly pink or red rather than black or dark brown, further tricking the patient into thinking that the new spot is harmless.
But it can also be black or brown, even purple or bluish.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.Source: ncbi.nlm.nih.gov/pmc/articles/PMC2644319/
Can Endometriosis Encroach on Nerves and Which Ones?

“Extragenital endometriosis” refers to endometriosis that affects areas beyond the genitals, such as various nerves.
“Endometriosis is a condition where the tissue that lines the uterine cavity — glandular tissue — is misplaced and studs tissues and organs outside of the uterus,” explains Karen Patrusky, a board certified OBGYN and F.A.C.O.G. in private practice for 20+ years.
“This tissue is hormonally responsive, regardless of its location, and breaks down and bleeds with each monthly cycle. This can result in debilitating cyclic pain.
“The most common organs affected by this condition are the ovary and the Fallopian tube.
“Next is the gastrointestinal system which can result in painful bowel movements and the urinary tract which can cause pain with urination and pelvic pressure symptoms.”
Which nerves can be affected by endometriosis?
“Endometriosis can cause pain by affecting nerves,” says Dr. Patrusky.
“It does this by either creating scar tissue near the nerves which can result in pain, and less commonly, by depositing and damaging the nerves directly.
“The nerves most likely affected by this condition are the nerves of the sacral plexus including the sciatic, obturator, pudendal and the gluteal nerves.
“These are a network of nerves that supply sensation to both the skin and muscles of the pelvis and lower limb.”
Sciatic nerve. Symptoms include shooting or stabbing pain going down the leg, often originating in the butt, and/or numbness and tingling in the butt, leg and/or foot. There may also be weakness in the foot.
The overgrowing uterine tissue can be right over the sciatic nerve region.
In fact, though extremely rare, endometriosis may grow ONLY over the sciatic nerve – a case of so-called isolated endometriosis.
And it’s not easy to diagnose because the symptoms are very much like those of sciatica that are caused by the far more common “pinched” nerve or tight piriformis muscle compressing against the nerve.
Obturator nerve. The pain may travel down the leg or affect the hips and groin.
Pudental nerve. Pain may occur in the anus, labia, perineum, rectum, urethra and vaginal region.
The pain may radiate beyond these locations. The discomfort may be a stabbing, numbness or painful intercourse.
Superior and inferior gluteal nerve. The pain may be in the buttocks and legs.
When the endometriosis is affecting, in addition to a nerve, the pelvic region, there’s usually the classic symptoms such as pelvic pain and intense menstrual pain, along with painful sex.
But when it’s in isolation, coming up with the right diagnosis can be vexing to the physician.
Endometriosis that affects the nerves requires a physician who is very experienced in this highly specialized area, as diagnosis can be quite tricky, and surgery (laparoscopic) will be required if medical management fails to alleviate the symptoms.
The surgical team should consist of three specialists: laparoscopic gynecologist, urologist and colorectal surgeon.
Nevertheless, endometriosis that encroaches on nerves is very rare.
Dr. Patrusky is the developer of Voila Intimate Mood Oil, a 100% organic, non-hormonal lubricant made from coconut oil infused with the purest natural herbal oils. All five formulas are vegan, cruelty-free and U.S. produced. Voilamoodoil.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/tommaso79
Sources:
endometriosisaustralia.org/single-post/2017/04/24/Endometriosis-in-and-around-the-nerves-%E2%80%93-What-can-be-done
nezhat.org/specialties/treatments-procedure/nerve-damage-caused-by-endometriosis.html
Can Women Who Don’t Drink Get Cirrhosis of the Liver?
It’s unsettling: Even a young woman who doesn’t drink can get cirrhosis of the liver.
The risk of non-alcoholic liver cirrhosis does not equally apply to men. (more…)
Can Low Back Pain Radiate to the Groin Area?

Low back pain can definitely radiate or “spread” to the groin, even though the source of the pain is only in the back rather than the groin.
Can Low Back Pain Spread to the Groin?
“Yes, if the injury on the disc is creating herniations on the L1/L2, the second nerve is close to the groin,” says Alfred O. Bonati, MD, owner of The Bonati Institute, a world leader in advanced spine surgery, Hudson, FL.
“To diagnose this issue a patient having these symptoms needs to get an MRI to see if the problem is associated with a bulging or herniated disc at this level,” adds Dr. Bonati.
Even when the back pain originates a little higher up, near the lower ribs, the discomfort can make its way to the groin area.
Though a nerve that comes out of the spinal cord need not be “pinched” to cause the kind of back pain that radiates to the groin, often this is the case.
There are nerves in the back that travel through the area of the groin and hence, can be part of a radiculopathy. Even the upper leg can be affected.
A cause other than a compressed nerve root is a narrowing of the spinal column, called spinal stenosis, which affects the low back.
“Correct diagnosis is the key when it comes to identifying the cause,” says Dr. Tom Carpenter, corrective exercise specialist, certified personal trainer and chiropractor, inventor of Stand Corrected™, a portable harness-like stretching tool that helps alleviate back, neck and shoulder pain.
Low back pain that radiates to the groin area “may be related a problem with the sacroiliac joint(s), referred pain from an inflamed nerve in the lumbar spine, hip problems which may include arthritis, a problem with the leg adductor muscles or a pelvic misalignment, to name a few,” says Dr. Carpenter.
 Dr. Bonati, a board certified orthopedic surgeon, was the first to develop and patent methods and instruments for laser assisted spine surgery – The Bonati Spine Procedures – for cervical, thoracic and lumbar spine problems.
Dr. Bonati, a board certified orthopedic surgeon, was the first to develop and patent methods and instruments for laser assisted spine surgery – The Bonati Spine Procedures – for cervical, thoracic and lumbar spine problems.

Photo credit: Aleesia Forni
Based upon 30+ years of experience, Dr. Carpenter’s practice approach reflects his belief that restoring optimum health and function will enable his patients to enjoy a much greater amount of vitality and wellness. Chiropractic care is true health care, not sick care!
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Doucefleur
Source: webmd.com/men/groin-pain
Can Endometriosis Cause Damage to the Kidneys?

Endometriosis not only can cause damage to the kidneys, but it can cause kidney loss.
The type of endometriosis that damages kidneys is called ureteral endometriosis. (more…)
Can a Pinched Nerve Un-Pinch & Go Away on Its Own?

The so-called pinched nerve, which for many people requires surgery to correct, can actually heal without any surgery and go away on its own.
In fact, there are people who’ve had a minor degree of pinched nerve in their history that went away on its own and they never knew it because they were never diagnosed.
As for a diagnosed pinch nerve that’s causing a lot of discomfort, you don’t want to sit around doing nothing and suffer.
There are nonsurgical treatment options.
Pinched Nerve in Neck
• Can cause shooting pains down the arm.
• Can cause numbness or weakness in a hand.
Pinched Nerve in Lower Back
• Pain can shoot down the butt and leg.
• There may be numbness, burning or tingling.
If your pinched nerve doesn’t seem to be going away on its own, or “un-pinching” itself, the conservative treatment may begin with physical therapy.
“Modalities such as strength exercises will typically work over a period of time,” points out Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
Dr. Perry adds, “It will take about two to three weeks — with two to three sessions minimum per week before patients will begin to see results.”
Dr. Perry recommends that patients wait at least three weeks to see if physical therapy is working.
It may even take up to six weeks for noticeable results. Hang in there.
PT may also include aerobic exercise and stretching.
Additionally, hot and cold compresses, plus pain pills, may be employed.
Surgical candidates are those for whom the symptoms are unbearable or for whom PT and other conservative approaches have not yielded results after six weeks.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Solid Web Designs LTD
Can You Prevent Sleep Apnea Sleeping Upright?

Which is more tolerable for preventing sleep apnea: sleeping upright or sleeping lying down with a CPAP machine on?
This is a million-dollar question to people diagnosed with sleep apnea who can’t stand using a CPAP machine – a special mask that prevents obstructive sleep apnea from occurring.
“People with untreated obstructive sleep apnea tend to find ways to mitigate the problem, often unconsciously — they just find that they sleep better if they do certain things,” begins Joseph Krainin, MD, board certified in sleep medicine and neurology and founder of the online sleep apnea clinic Singular Sleep.
“Raising the head of the bed can definitely help by removing the impact of gravity on promoting upper airway obstruction at the level of the tongue base and soft palate,” continues Dr. Krainin.
“I often encounter patients early in their journey with OSA who sleep with two pillows.
“This may progress, as the disorder gets worse, to only being able to sleep upright in a chair.”
Ever sleep in a chair? It’s not very comfortable unless the chair is reclined somewhat—which then wouldn’t make it really upright.
Of course, there are special implements that you can fashion to your bed to allow you to sleep at nearly a 90 degree angle of trunk flexion relative to your legs.

Theoretically you can prevent sleep apnea by sleeping upright – if you can find a setup that’s tolerable throughout the entire night — such as a wedge pillow.
Your head and neck may be quite comfortable in the upright position using the wedge implement, and even your legs could be quite comfy with a pillow or two beneath your knees.
But your poor butt would probably start getting very uncomfortable shortly into your sleep.
To circumvent that problem you could always use a bed with a mechanism that cranks the mattress upright — and simultaneously cranks up the opposite end to elevate your legs, reducing pressure on your bottom.
These types of beds are pricey, but even if you could easily afford one, you’d still end up being locked in one position — since sleeping on your side while upright would be unbearably uncomfortable.
Thus, sleeping upright is not a practical solution for sleep apnea.
However, if you end up in a situation where you’re separated from your CPAP machine and must go to bed without it…you may want to figure out a way to keep your body propped up overnight.
 In 2013 Dr. Krainin was elected a Fellow of the American Academy of Sleep Medicine, an honor reserved for sleep doctors who’ve made significant contributions to the field in education, research and service.
In 2013 Dr. Krainin was elected a Fellow of the American Academy of Sleep Medicine, an honor reserved for sleep doctors who’ve made significant contributions to the field in education, research and service.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.











































