Why Does the Diastolic Blood Pressure Vary So Much?

Your diastolic (the lower number) blood pressure just jumps around so much whenever you have a blood pressure reading.
One day it’s 80. Next day or even next hour it’s 68. A few days later it’s in the 70s. Meanwhile, the systolic (top number) value stays pretty much the same.
“That is normal,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“Actually, all measurable bodily functions vary throughout the day depending on what you are doing, your hormones and other bodily functions, circadian cycle,” continues Dr. Besser.
“So, this variability is expected. A comparison might be your home thermostat — even though it is set for one temperature, the temperature in your home will vary during the day and night, depending on many factors (like the amount of sunshine, outside air temp, the number of people in the house, whether the oven is on and so on).”
Do not obsess or fixate on the variability of the diastolic or systolic number of your blood pressure readings.
What’s important is that both numbers are within the range for normal blood pressure.
What Is Normal Blood Pressure?
In late 2017 new guidelines were established by the American College of Cardiology and the American Heart Association.
Normal: Less than 120/80 mm Hg
Elevated: Systolic between 120-129; diastolic less than 80
Stage 1 hypertension: Systolic between 130-139 or diastolic between 80-89
Stage 2 hypertension: Systolic at least 140 or diastolic at least 90 mm Hg
For best results with a home blood pressure monitor, take the reading after you’ve been sitting calmly for at least 10 minutes.
A reading at a doctor’s office may reflect the so-called white coat syndrome, in which BP is elevated due to anxiety.
Increasing your consumption of raw vegetables and fruits, and reducing your intake of processed foods, will lower your baseline blood pressure.
So will structured exercise and quitting smoking.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ Andrey_Popov
Source: acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017
Why Your Chest Feels Heavy After Eating: Heart vs. Heartburn

Ever get that heavy feeling in your chest after eating and wonder if the food is triggering a heart attack or if some heart problem is responding to your meal?
And the meal doesn’t necessarily have to be big or full of fat or grease in order to cause this heavy chest feeling. (more…)
Throbbing Blood Vessels vs. Twitching Muscles

You suddenly feel something squirming or thumping in your neck, stomach or leg: Is this a blood vessel throbbing or a muscle twitching?
Sometimes, the “crawling” sensation occurs in multiple spots at the same time in a large area such as the back of the legs – with various sections acting up only seconds or minutes apart.
The body is rampant with blood vessels, ranging from those that are microscopic in diameter to the biggest blood vessel in the body: the aorta.
So how can you tell if the “twitching” is actually a throbbing blood vessel vs. a muscle?
“Well, actually, the twitching is due to a nerve misfiring causing the muscle to twitch,” begins Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
Dr. Besser explains, “It’s the same mechanism as hiccups, although in that case the misfiring nerve causes the diaphragm (a muscle) to twitch.
“So you really aren’t feeling veins [or blood vessels] at all, but the result of a nerve misfire.”
When I was a child I thought that the squirmy or wriggling sensation (think a worm in the ground) was a vein or artery throbbing, and thought nothing of it. Kids are fearless, aren’t they?
But some adults believe that they’re feeling a blood vessel throbbing or pulsating, when in fact, it’s nothing more than a benign twitching of muscles (fasciculations).
However, let’s face it: It FEELS as though a vein is pulsing or throbbing.
Every day, we can SEE our veins protruding in our hands and feet, and sometimes arms. Imagine if one started throbbing.
What might it feel like? And voila, people draw the conclusion that their veins are pulsating or vibrating.
But rest assured, next time you feel a worm crawling under your skin, this is not a vascular situation. It is muscle fibers misfiring.
By far, the most common causes of twitching muscles are fatigue, physical stress, exercise and anxiety – including anxiety over the fasciculations.
Another cause is magnesium deficiency. This mineral promotes muscle relaxation.
If your body is short on magnesium, then another mineral — calcium — will cause muscle contraction.
Ongoing twitching can be caused by inadequate calcium and magnesium.
So it’s time to stop fearing that your blood vessels are throbbing, and instead, to realize that you can bet the farm that it’s just some harmless muscle twitching.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Image Point Fr
One Nipple in Men Bigger than the Other: Why?

Are you a man who spends too much time inspecting the nipple that’s bigger than the other?
Or perhaps you see it as one nipple being smaller than the other. (more…)
Can Low Blood Pressure Make You Cold?

Do you ever get waves of suddenly feeling cold or chilly, despite the room temperature being 72 or even 75?
Could this be low blood pressure?
Not only do your hands feel cold, but you know you’d feel more comfortable with a sweater on.
When you place your hands to your tummy, you can’t keep them there because they’re so cold!
Yet otherwise you feel perfectly fine.
Can low blood pressure make you feel cold?
“No, your blood pressure does not really affect your temperature,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“Temperature regulation is controlled by different mechanisms than blood pressure regulation,” continues Dr. Besser.
“And feeling cold really isn’t related to blood pressure at all (within normal ranges).
“Obviously if you have a serious illness that causes low blood pressure (like significant blood loss), you might also feel cold.”
But for the vast majority of people who, for no apparent reason while at their computer, watching TV or during some other passive activity start feeling chilly, the cause is not related to low blood pressure or significant blood loss.
If you feel cold constantly or on a frequent basis with no explanation, see a doctor, as there are MANY medical conditions that can cause one to feel chilly.
If the sensation is only on a periodic basis, it could be anxiety related, even if you’re not actively thinking of the stressors in your life.
It could be background anxiety, kind of like a “stress malware program” running in the background of your mind’s computer.
It could also be a heating malfunction in your home that’s not showing on the thermostat.
Check the heat source (e.g., heating vents that run along the baseboards) to see if heat is being generated.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/bissun
Why Does My Heart Beat Fast when Trying to Fall Asleep?

It’s not always increased awareness that makes you realize that your heart is beating pretty fast as you lie in bed to go to sleep at night.
Though for some people, this explanation holds.
“It may be an increased awareness of your body’s function (you are just lying there focusing on yourself without distractions),” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore, and Diplomate American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
Dr. Besser continues, “Two, because you are just lying there you may start to think about your day (and the stresses). Obviously that my raise your pulse.
“Lastly, when you lay down your blood pressure and other bodily functions adjust to your new position — that could also cause a transient increase in pulse.”
If you know for a fact that your heart beats faster after lying down at bedtime – because you’ve taken or felt your pulse while awake at night and then taken or felt it again after getting in bed – this is clearly not an issue of increased awareness.
Keep in mind that simply taking or feeling your pulse while in bed can induce anxiety that makes your heart beat faster.
You may want to wear a pulse oximeter that records heart rate while you’re up and about for a few hours before bedtime, and then keep it on your finger after getting in bed and falling asleep.
Next time you awaken, remove it. It will have retained a recording of the data.
The only caveat is that sometimes these devices are tricky as far as retrieving the data.
But if you can figure it out, you’ll note that once you fall asleep, your heart rate will be slower than it is at any point of the day.
You’ll also be able to see if your heart rate truly does soar after you lie down.
Note the time you get into bed, because the oximeter data will have a timeline to match that up against.
Shifting around in bed, struggling to find a good position with the blankets and pillows, etc., will raise heart rate.
But once you’re lying still, the oximeter will record what your pulse is, as well, and you can look at the objective data after you upload it to your computer.
If you truly had a heart problem that was causing an accelerated pulse, this would happen while you were up and about.
A heart problem doesn’t wait until you’ve just gotten into bed to start speeding up your pulse, especially since lying down reduces your body’s energy needs – save for that transient adjustment to your new position that Dr. Besser pointed out or slugging the pillows.
Lying down to go to sleep may also be a conditioned stimulus to anxiety – thinking about your day, as Dr. Besser also pointed out.
Or, it may be the next day that you’re thinking about that gets your heart beating faster than usual.
Solutions
• A full cardiac workup that comes out negative for any problems will really put your mind at ease.
• However, you may still find your heart beats fast the moment you lie down for sleep – due to anxiety about the issue despite normal test results, and/or anxiety about your life.
• Before going to bed, get ready for the next day as much as possible.
• Lay out next day’s clothes.
• Prepare next day’s breakfast as much as you can, such as cracking and mixing the eggs and seasoning them, then placing them in a covered bowl in the refrigerator. Set out the pan and spatula, plates and silverware, etc.
• Prepare next day’s lunch.
• Set snail mail you want to send at your front door so you won’t forget it.
• Write out a to-do list of tasks you must get done the next day.
This way, by the time you lie down to go to sleep, your anxiety levels will be reduced, and your heart should not be beating so fast anymore due to anxiety.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Supawadee56
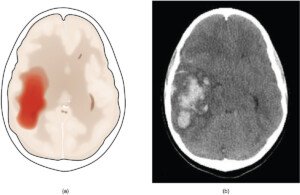
Can an MRI Miss a Head Injury and Not Show It?

Head injuries are very common, including among kids, so it’s crucial for an MRI to show a head injury.
However, this isn’t always the case — in that this technology doesn’t always show trauma to the brain. (more…)
Getting an MRI if a Family Member Has a Brain Aneurysm

Did you recently learn that an immediate family member has an aneurysm and are wondering if you should undergo yearly MRI screenings, what with all the anxiety this would cause? (more…)
Why Aren’t There Routine MRI Screenings for Brain Aneurysm?
Medical plans don’t include the mention of “routine” MRI screenings for a brain aneurysm.
And this seems pretty odd, given that often, the first symptom of such an aneurysm is a thunderclap headache soon followed by death. (more…)
Can an Unruptured Aneurysm Cause Headaches?