Shortness of breath is a common symptom of COVID-19, but feeling short of breath may also be a prominent symptom of blocked arteries or a weak heart.
“Shortness of breath is a symptom that could be related to multiple medical conditions, including infectious diseases, cardiovascular issues, pulmonary disorders, abnormalities of the blood, etc.,” begins Carlos González Quesada, MD, FACC, attending cardiologist with Cedars-Sinai Medical Center and a cardiologist with Cardiovascular Medical Group of Southern California.
COVID-19, medically known as SARS-CoV-2, is an infectious disease.
“For physicians and other healthcare providers, it could be challenging to determine the origin of the shortness of breath,” says Dr. Quesada.
“In most cases complete physical examination and a detailed interview will be enough to narrow the list of differential diagnoses.
“In the current era it is critical to quickly distinguish the patients who are infected with the severe acute respiratory syndrome coronavirus 2 from patients who develop shortness of breath secondary to a cardiovascular condition.
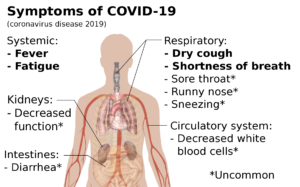
“The context and the clinical picture are essential. Patients infected with SARS-CoV-2 will typically present with associated symptoms such as fever, cough, diarrhea, nausea or vomiting. These patients will likely have a history of exposure to the virus.”
Does shortness of breath from COVID-19 feel different than from heart disease?
“Physicians will usually focus on the characteristics of the shortness of breath to determine the source of the symptoms,” says Dr. Quesada.
“For example, patients with heart failure will develop shortness of breath over the course of weeks to months.”
Heart failure may be acute or gradual and chronic. In either case, the heart does not efficiently pump blood – which means reduced oxygen throughout the body.
“The shortness of breath commonly worsens when they are lying down,” continues Dr. Quesada.
“For example, at night, they will require two or three pillows under the head to improve their shortness of breath.
“In extreme circumstances, these patients will only feel relief when they are sleeping in a chair.
“These patients will also present with swelling of the legs, and not uncommonly, will complain of abdominal fullness.”

Swelling caused by fluid retention (edema). Shutterstock/Valerio Pardi
The swelling of the lower extremities may not be blatantly obvious if it’s mild or if the patient is overweight.
“Patients with heart failure will need to be assessed in the emergency department and potentially be admitted for further management.”
Keep in mind that a person with chronic or acute heart failure may also be infected with COVID-19.
“Patients presenting with a heart attack usually complain of shortness of breath associated with chest discomfort.
“They report chest pressure or tightness. It is not uncommon for these patients to state that their chest pressure feels as if an elephant was sitting on the chest.
“The pain can radiate to their face, shoulder or back. Usually the symptoms are acute and will develop over the course of minutes to hours.
“In some cases [of heart attack], patients suffer from nausea and vomiting. Likewise, these patients will require urgent assessment in the emergency department.
“In contrast to patients with COVID-19, patients with heart failure or heart attack will unlikely present with fever, history of exposure to the virus or diarrhea.”
What about shortness of breath from coronary artery blockages?

Shutterstock/pikselstock
A person with clogged arteries isn’t going to wake up one morning suddenly struggling to breathe or feeling as though there’s an oxygen deficit – when prior everything was fine.
The onset of “getting out of breath” or the need to breathe harder — upon physical activity that normally didn’t require heavier breathing — will be very gradual – because buildup of plaque in the coronary arteries is very gradual.
The more sedentary a person is, the more gradual the effects of reduced blood flow in the heart will seem.
After all, it doesn’t require as much oxygen to be sedentary as it does to be active.
The progression of getting easily winded from routine activities can fool the patient into thinking he’s “just getting old” or “out of shape.”
On the other hand, a person with COVID-19 – even if sedentary – may wake up one morning and seemingly out of the blue feel oddly short of breath and/or experience difficulty breathing.
He or she is not going to think, “Gee, I must be getting old,” or, “Gee, I really need to start exercising.”
Mikael Häggström, MD/CC0, via Wikimedia Commons
Someone with this coronavirus infection may report that the breathlessness was sudden.
However, this individual probably felt under the weather or “coming down with something” for about a week before “suddenly” feeling unable to catch their breath.
They may not have told anyone of preceding symptoms, or, brushed those symptoms off as being from stress, age or the common cold.
Finally, don’t ever self-diagnose – even if you don’t think you’ve had enough community exposure to get infected. If you have unexplained shortness of breath, get to the ER.
 Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
Dr. Quesada is board certified in internal medicine and cardiovascular diseases, with subspecialties in general cardiology plus interventional and structural cardiology. He evaluates and treats many conditions including shortness of breath, chest pain, coronary blockages and clot disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.