Researchers are starting to uncover how excess body weight may influence the development of Alzheimer’s disease.
For the first time, scientists examined how obesity affects Alzheimer’s disease blood biomarkers. The findings suggest that obesity may accelerate biological changes linked to Alzheimer’s, even when early tests appear reassuring.
This research was presented at the annual meeting of the Radiological Society of North America in 2025.
First Evidence Linking Obesity and Alzheimer’s Blood Biomarkers
The research team found that Alzheimer’s-related blood biomarkers increased much faster in people with obesity than in those without.
In some cases, biomarker levels rose up to 95 percent more quickly.
According to senior author Dr. Cyrus Raji, this is the first study to clearly demonstrate a relationship between being fat and Alzheimer’s disease using blood biomarker tests.
That makes it a major step forward in understanding how body weight may influence brain health over time.
Using Long-Term Brain Imaging and Blood Data
To explore this link, researchers analyzed five years of data from 407 participants enrolled in the Alzheimer’s Disease Neuroimaging Initiative.
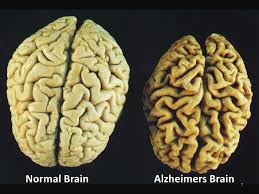
These volunteers had regular blood tests as well as amyloid PET scans, which detect amyloid plaque buildup in the brain, a hallmark of Alzheimer’s disease.
The team examined several well-known Alzheimer’s biomarkers in blood samples.
These included pTau217, which is used to diagnose and monitor Alzheimer’s, neurofilament light chain, a marker of nerve cell damage, and GFAP, a protein linked to supportive brain cells called astrocytes.
Connecting Body Weight to Brain Changes
Researchers looked at how these blood biomarkers related to body mass index, or BMI, over time. They also compared the blood test results with findings from brain scans to confirm consistency.
At the beginning of the study, people with higher BMI actually showed lower levels of Alzheimer’s blood biomarkers and lower amyloid buildup in the brain.
On the surface, this could look like a protective effect.
However, researchers believe this early finding is misleading. The lower biomarker levels in people with significant overweight were likely caused by dilution from higher blood volume, not lower disease risk.
Without tracking changes over time, obesity’s true impact could easily be missed.
This is where long-term data becomes crucial.
A longitudinal study follows the same people over several years, allowing researchers to see how conditions evolve or trend rather than relying on a single snapshot in time.
As the study continued, a different pattern emerged. Alzheimer’s biomarkers and amyloid buildup increased faster in obese participants compared to those who were not.
Obesity Accelerates Alzheimer’s Related Changes
Over time, obese subjects experienced significantly faster rises in key biomarkers.
- Plasma pTau217 levels increased between 29 and 95 percent faster.
- Neurofilament light chain rose about 24 percent faster
- Amyloid accumulation in the brain increased more quickly as well.
Interestingly, blood tests proved even more sensitive than PET scans for detecting obesity’s influence on Alzheimer’s-related changes.
This suggests blood biomarkers could play a growing role in early detection and risk assessment.
![]()