Does Fasting Glucose Reading of 106 Mean Insulin Resistance?
If your fasting glucose is about 106, do not panic, as this does not automatically mean you have insulin resistance or prediabetes.
A few years ago I visited a general practitioner to find out why I was suddenly having a lot of diarrhea.
I decided to add in a routine physical, which included the standard fasting glucose test.
The result was 106, which netted a “flag” alert in the report, that was e-mailed to me.
The test result came a few days before my visit, and the doctor merely mentioned that it was flagged, but not to worry about it.
Several months later I was reviewing my medical paperwork and saw the printed-out blood glucose result. In the next column it said “impaired glucose metabolism.” WHAT?!
A normal fasting blood sugar reading is 70-100 (mg/dL).
The American Diabetes Association says that 1-2 hours after eating, the fasting glucose (blood sugar) reading should be under 180 mg.
The ADA says that over 125 for fasting glucose means diabetes.
So what does 106 mean?
According to Kaiser Permanente (my HMO at the time of the blood sugar test), a normal fasting glucose result is “less than or equal to 110 milligrams per deciliter.”
Two years ago, however, their normal range was under 100, which was why my result of 106 was flagged.
The Kaiser site for test result information is open only to members, and it states:
“These ranges vary from lab to lab, and your lab may have a different range for what’s normal.
“Your lab report should contain the range your lab uses. Also, your doctor will evaluate your results based on your health and other factors.
“This means that a value that falls outside the normal values listed here may still be normal for you or your lab.”
The site lists factors (other than diabetes) that can cause a high blood sugar reading, and first on the list is “Stress.” This information was not there two years prior to my checking it.

Shutterstock/Gustavo Frazao
If you have a fasting blood sugar reading in the low 100s like mine was, ask yourself how much stress you’ve been under lately.
As a former personal trainer, I am well-versed in blood sugar’s impact on the body, as this is the main fuel source for working muscles and is highly manipulated by exercise and diet.
If you’re under chronic stress, your body is in a perpetual “fight or flight” state.
To prepare for the fight or flight, the liver dumps sugar into the bloodstream as a ready fuel source for muscles.
In chronic stress, however, the fight or flight never comes, and blood sugar remains elevated.
A bout of intense exercise will lower the blood sugar and keep it lowered for awhile, but if the stressor doesn’t go away, the fasting blood sugar may bounce right back up again into the low 100s.
For eight weeks prior to my fasting glucose test, I was under extreme emotional duress – it was really ugly, and I developed microscopic colitis as a result (which caused the diarrhea).
However, disrupted sleep can cause insulin resistance (elevated fasting blood sugar that’s not elevated enough to qualify for diabetes).
David Edelson, MD
For my article titled “Can Poor Sleep Cause Insulin Resistance,” I interviewed Dr. David Edelson, MD, board certified in internal and bariatric medicine, one of the top obesity experts in the U.S., and founder and medical director for HealthBridge.
“There is a strong association between sleep disorders and both obesity and insulin resistance,” explains Dr. Edelson in my article.
“When I refer to sleep disorders, I am speaking of anything that can cause either a lack of sufficient quantity of sleep (insomnia, lifestyle issues) or poor quality (sleep apnea, restless legs, fragmented REM sleep, etc.).”
In fact, insulin resistance (prediabetes) can be caused by just one night of bad sleep, says a report in the Journal of Endocrinology & Metabolism (2010).
“Our data indicate that insulin sensitivity is not fixed in healthy subjects, but depends on the duration of sleep in the preceding night,” says the report.
Not only was I experiencing horrendous anxiety for eight weeks, but throughout that eight weeks, my sleep was disrupted every single night.
After doing my homework about what an elevated fasting glucose might really mean, I was not surprised mine came in at 106.
I was in a fight or flight mode every waking minute, which included lying in bed with a racing heart from the anxiety, unable to sleep soundly.
Two years later I had another fasting glucose test: 85. The stressors of two years ago were well-behind me.
Based on just one blood sugar test of around 106, you should not jump to conclusions and assume you have prediabetes or insulin resistance, especially if you exercise, are not overweight and have a pretty healthy diet.

Dr. Edelson is widely recognized as one of the nation’s top weight loss experts, and was listed in NY Magazine’s “Best Doctors of 2014” issue.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Depression Treatment: T3 Better than Antidepressants

T3 just may work better on depression than antidepressant drugs.
A large percentage of people suffering from depression actually have low thyroid, says Dr. Kent Holtorf, MD, thyroidologist and founder of Holtorf Medical Group in California.
In other words, many people’s clinical depression is caused by underactive thyroid (hypothyroidism) and they don’t even know it, and hence, are unaware of a highly effective treatment: T3.
Hypothyroidism (underactive thyroid) is associated with weight gain, fatigue and feeling cold, but depression is also a common symptom, and may even be the only symptom.
“The largest study done on the treatment of hypothyroidism with antidepressants found that supplementing with the thyroid hormone T3 worked as well or better than all the antidepressants,” says Dr. Holtorf.
“This is one of the hundreds of studies that demonstrate that a large percentage of patients with depression are actually low thyroid.”
Physicians are missing this cause of depression (low thyroid) left and right, and instead, writing out the prescriptions for antidepressants in droves.
The Star*D report is the largest trial, with over 4,000 patients, comparing antidepressant effectiveness for depression treatment.
Dr. Holtorf says the study found that “Sixty-six percent of patients fail to respond to antidepressants or have side effects severe enough to discontinue use.”
Side effects of antidepressants can actually be disabling, including dizziness, nausea, more depression, and suicidal thoughts in teen and young adult patients.
Of patients who do respond well to antidepressants, says the Star*D study, more than half will relapse within a year.
However, this investigation found that “T3 was effective even when other medications — such as Celexa, Wellbutrin, Zoloft, Effexor, or (behavioral) cognitive therapy — were not,” explains Dr. Holtorf.
T3 was shown to be 50 percent more effective, he continues, “even with the less than optimal dose of 50 mcg, under direct comparison with significantly less side effects than commonly used therapeutic approaches with standard antidepressants.”
A standard thyroid function test, obtained by drawing blood, will not reveal low T3 levels.
Hence, a doctor reviewing a patient’s blood work will not pick up on potentially low T3 levels.
I asked Dr. Holtorf why doctors don’t order a specific T3 test when a patient presents with depression.
He replies, “The simple answer is that the tests check what is in the blood, but what matters is what is in the cells.”
The TSH (thyroid stimulating hormone) is the standard test given to people for their annual physical checkups.
Dr. Holtorf says this test is regarded as the most sensitive marker of the peripheral tissue levels of the thyroid.
However, this view is incorrect, he continues. “Most endocrinologists and other physicians erroneously assume that, except for unique situations, a normal TSH is a clear indication that the person’s tissue thyroid levels are adequate.”
Low thyroid levels are clearly a culprit in many cases of depression.
The importance of T3 levels must not be overlooked. Dr. Holtorf explains, “Not only can low thyroid cause depression, but it can make it much worse in the face of depression, so every person needs to get their thyroid levels tested.
“The problem is that the standard blood tests that are typically used by the overwhelming majority of doctors will miss low thyroid levels in depression.
“Why? What is called a free T3/reverse T3 ratio is currently the best method to detect these low levels in depression.”
For all people with depression and even bipolar disorder, a time-released supplementation with T3 should be considered as possible treatment despite a seemingly “normal” serum thyroid level, continues Dr. Holtorf.
A standard TSH test may be “normal” in a patient exhibiting classic signs of depression, but again, the standard TSH test is not sensitive to measuring T3 levels.
Though supplementation with T3 (the active thyroid hormone) may effectively treat a person’s depression, Dr. Holtorf stresses that “Straight T4 (the inactive thyroid hormone) should be considered inappropriate and suboptimal therapy for replacement in such patients.”
The thyroid supplement is not synthetic; it is bioidentical, meaning it’s the actual hormone that the patient takes every day in the form of a small pill.
Here are three study references that report the strong link of low thyroid (T3) to depression:
Int J Neuropsychopharmacology 2008;11:15-25
Journal of Affective Disord 2009;116:222-226
Am J Psychiatry 2006;163:1519-1530
 Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
Dr. Holtorf has published a number of endocrine reviews on complex topics in peer-reviewed journals on controversial diseases and treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How Can Being Diabetic Cause Mood and Anger Problems?
Having diabetes is no excuse to blow your top and be angry at your loved-ones all the time, but this disease indeed could lead to factors that can alter mood and even cause ADHD symptoms.
Now on one hand, it seems there’s no connection between being easily aroused to anger, ADHD or being very moody, and having diabetes.
But on the other hand…
Now suppose an adult or child in your life has anger issues, or frequently has mood disturbances or signs of ADHD.
Diabetes As a Cause
This person can very well have diabetes, and the diabetes can very well be causing or significantly contributing to anger outbursts, moodiness and/or ADHD symptoms.
I asked whether or not diabetes can be connected to anger and mood to Dr. Georgianna Donadio, DC, a nutritionist, health educator and Program Director of the National Institute of Whole Health in the Boston area.
Diabetes Can Cause Angry Mood Problems and ADHD
“The answer is a resounding yes,” she replies. In the brain is a neurotransmitter called dopamine, and excess amounts of dopamine are associated with mood and behavioral changes.
Dr. Donadio explains, “Vanderbilt University Medical Center identified that insulin levels affect the brain’s dopamine system, which is involved in many neuropsychiatric conditions, including drug addiction, Parkinson’s disease, ALS, and so forth.”
Two Types of Diabetes
They are type I and type II. Type I is also known as insulin-dependent diabetes. The patient’s pancreas does not produce any insulin. Ten percent of diabetics have type I.
In type II, the patient’s pancreas produces insulin, but the body does not know what to do with it.
Though about 80 percent of type II diabetics are overweight, and this type of diabetes is strongly correlated with being overweight, lack of exercise and poor eating habits, a thin person can still develop type II if other lifestyle risk factors are present.
Genetics also play a role, but not in terms of destiny, but rather, in terms of predisposition.
If a person has anger problems or ADHD symptoms before developing diabetes, then if the diabetes isn’t managed properly, the condition can have a definite impact on that person’s temper and mood.
Dr. Donadio continues, “In addition, theirs (Vanderbilt University Medical Center) and other studies have provoked questions regarding how controlling insulin levels (such as in diabetes) can have an impact on and for ADD, ADHD, and this suggests that the effects of kids/adults having high carbohydrate/sugar diets may be a critical factor in the development of ADD, ADHD and other neurological/brain conditions.”
She adds: “The brain needs glucose to function properly and without proper insulin regulation, sugar levels can become erratic and seriously impact cognitive and neurological functioning.
“People with hypoglycemia often have severe glucose swings and personality issues as a result.”
Hypoglycemia is low blood sugar.
If you, or and adult or child in your life seems to have anger management issues, throws temper tantrums, has temper outbursts, rouses easily to a hostile mood, or shows ADHD signs, consider the possibility that diabetes is at least partially the cause.
 For 35+ years Dr. Donadio has educated the healthcare community, her patients, students and the public about how the physical, emotional, nutritional and environmental aspects of our lives can produce illness or wellness.
For 35+ years Dr. Donadio has educated the healthcare community, her patients, students and the public about how the physical, emotional, nutritional and environmental aspects of our lives can produce illness or wellness.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Can Carnivora Cure Cancer or Are Radio Ads All Hype?

The ads for Carnivora on the “Coast to Coast” radio show are incessant and strongly hint it can cure cancer.
If you’re a faithful listener to “Coast to Coast,” then you already know that this popular program frequently runs ads for Carnivora.
What really got my attention was that the ad (in the past, voiced-over by “Coast to Coast” host George Noory, and as of 2019, by Carnivora International founder Richard Ostrow), claims that Carnivora can eradicate abnormal cells while sparing normal cells.
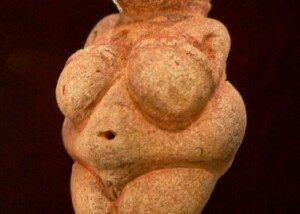
Carnivora is the name of a product that, according to its site is an extract of a species of Venus flytrap known as Dionaea muscipula, and comes in capsule and liquid form.
The description of what Carnivora does is actually the cure for cancer!
It would be illegal for Carnivora International to outright state, “Carnivora can cure cancer.”
Instead the company cleverly masks this bold statement with their claim — but anyone familiar with what malignancy actually is can see right through their cryptic message.
Any company that makes a thinly veiled claim like that had better be able to back it up.
“I have never heard of this specific product, but it is my opinion that these miracle cures touted on media are pure hype and not true (think ‘snake oil salesman’),” explains Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“Consumers should always take these ads with skepticism and speak with their PCP.
“Also, one should be careful about mixing these OTC treatments with whatever prescription medications they are taking; these ‘drugs’ could interfere/interact with prescription medications.”
The product’s site makes it appear as though there’s been a lot of valid, replicated research showing that the product kills cancer cells.
There are things, however, that the company doesn’t tell you, but the American Cancer Society certainly does.
According to the ACS site, there is no scientific evidence that Carnivora is effective at treating any kind of cancer.
One of Carnivora’s claims is that it can reverse skin and other types of cancer.
The ACS site explains that a German physician patented Carnivora after taking liquids from the Venus flytrap and testing to see if they could digest abnormal proteins in cancer cells.
The ACS further says that in 1985, this physician claimed that 56 percent of 210 people with cancer experienced remission or stabilization after taking the extract.
These findings were published in a “little-known German medical journal,” continues the ACS. The findings were never confirmed, either.
The active ingredient in the Venus flytrap is thought to be plumbagin.
The ACS says that claims for what the Venus flytrap can do for malignancy cannot be supported with science.
One of the radio ads on “Coast to Coast” points out that former President Ronald Reagan used Carnivora successfully, but interestingly, the ad doesn’t say for what — apparently wanting listeners to connect the dots and assume he used it for his much-publicized colon cancer.
Yes, Reagan recovered from colon cancer, but he also received conventional medical treatment including surgery!
Another point of interest: The ACS says that most of the studies involving the Venus flytrap extract were done by the doctor who patented Carnivora.
He had a huge financial stake in the clinic that administered the product, as well as in the manufacturer of this product!
The ACS states on its site regarding plumbagin:
“Although animal and laboratory studies show promise, further studies are necessary to determine whether the results apply to humans. It is important to remember that purified compounds such as plumbagin are not the same as the fresh plant extract, and study results would not be likely to show the same effects.”
- So, can Carnivora cure cancer?
- You be the judge.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Sources:
Cancer.org/Treatment/TreatmentsandSideEffects/ComplementaryandAlternativeMedicine/HerbsVitaminsandMinerals/venus-flytrap?sitearea=ETO
Carnivora.com
Cough After Pneumonia Can Last a Few Weeks After Recovering

A doctor says that after recovering from pneumonia, the cough can persist for a few weeks.
“Yes, it is true,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“It is because the damage to the lung tissue (inflammation) can take several weeks to completely heal.”
Years ago a doctor had told my mother that “I think it’s completely normal for a cough to drag on for a couple weeks even after the pneumonia is gone.”
A CT scan showed that my mother no longer had pneumonia.
She had the CT scan because a D-dimer test result was elevated, and when this result is elevated, it can indicate the presence of a pulmonary embolus (blood clot).
This was while she was in the midst of recovering from pneumonia, which of course, was characterized by plenty of coughing and hacking.
The ER doctor said that a CT scan is far more definitive than X ray, and since it showed no pneumonia, she was declared free of the infection, even though she was continuing to cough.
A few days later my mother then had a follow-up with her primary care physician.
I was present in the office and asked just how long a cough is supposed to last after one recovers from pneumonia. This came up a few times during the course of the visit.
In addition to the first verbatim quote mentioned at the beginning of this article, the doctor also stated:
“It’s absolutely normal that you still have a cough. That cough can drag on for another few weeks.
“It caused damage to the airways. Your body still has to clean everything out.
“It can be two or three months before you feel completely normal.”
This was all after I had initially asked, “Can a person still be coughing sputum after the pneumonia is cleared?”
The physician responded, “Yes. It can take a couple of weeks for all that to clear up.”
Never be “afraid” to ask a doctor many questions!
You are not expected to know what a doctor knows, and hence, doctors welcome questions.
So there you have it, stated several times by a doctor seeing my mother who, two days prior, was told that she no longer had pneumonia, but was still having occasional bouts of productive coughing-phlegm or sputum coming up.
The doctor also said that it’s good that all that phlegm is coming up, and that the patient should never swallow it.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Ruslan Huzau
Zanaflex Withdrawal: How to Get off this Drug Smoothly
Here’s best way to get off zanaflex, says a doctor.
Zanaflex withdrawal can be a very troublesome experience, but there’s a way to get off Zanaflex smoothly and safely.
Zanaflex is a drug for muscle spasms.
“The literature and common practice both dictate that Zanaflex (tizanidine) be discontinued by tapering off the drug gradually over a period of one to two weeks,” says Frederick Arthur Ehlert, MD, Cardiac Electrophysiology and Pacing division at ColumbiaDoctors Eastside, NY, NY.
“While there may be some rebound effect if it has been taken on a regular basis for a considerable period of time, gradual reduction of the dose will usually prevent any significant rebound effect.
“There is no replacement or step-down drug, just tapering, which is often easier with the tablet form rather than capsules.
“But if capsule dosage is relatively high it can be halved, and then, if necessary, one’s doctor can prescribe a lower dose to continue the tapering at a lower dose.”

Zanaflex
What are the common withdrawal effects of Zanaflex?
Dr. Ehlert: With the abrupt cessation of Zanaflex (tizanidine), there is a risk of rebound hypertension, which means a high blood pressure, which results from the sudden discontinuation, tachycardia (which means a rapid heart beat, usually a normal heartbeat going faster than normal), and hypertonia (which means muscle spasms).
Can a person just outright quit Zanaflex, and why not?
Dr. Ehlert: Why is that dangerous? The high blood pressure in this rebound effect can conceivably go very high and cause strokes or other organ damage.
Can you recommend some ways a person can go about weaning off Zanaflex, or things they can do (maybe with diet or supplements) that can ease the transition off the drug?
Dr. Ehlert: The recommended initial dose of the drug is 4 mg/day with gradual increases (in 2-4 mg increments over 2-4 weeks to a maintenance dose of 8 mg every 6-8 hrs.
Withdrawal of the medication to eliminate side effects should replicate these increases. Diet or supplements are not really helpful in this.
Remember, to get off Zanaflex with minimal problems, gradually reduce your dose with your doctor’s supervision.
 Dr. Ehlert’s areas of expertise include sudden cardiac death and heart rhythm disorders. He has authored over 40 peer-reviewed papers, reviews and book chapters in electrophysiology.
Dr. Ehlert’s areas of expertise include sudden cardiac death and heart rhythm disorders. He has authored over 40 peer-reviewed papers, reviews and book chapters in electrophysiology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
How Long Before Effexor, Cymbalta, Paxil, Zoloft Take Effect?
When do effects of cymbalta, effexor, paxil and zoloft kick in?
What’s the time it takes for Cymbalta, Effexor, Zoloft and Paxil to start working?
Cymbalta, Effexor, Zoloft and Paxil are commonly prescribed antidepressants, and if you’re thinking of taking an antidepressant, you’ll be wondering how long before drugs such as Effexor, Cymbalta and Zoloft take to start creating some effects against your depression.
Just how long does it usually take before antidepressants such as Effexor, Cymbalta, Paxil and Zoloft to begin taking effect?
“At least 50 percent of those who will eventually respond to the above mentioned antidepressants will begin to demonstrate improvement within one week of treatment initiation,” explains Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
“Users most often report an increase in energy and productivity, and a decrease in sensitivity (particularly to inappropriate comments from others), and a decrease in anger within the first seven days of use.”
If you are battling depression, and have tried holistic measures to relieve it, but natural treatments have failed, and the depression is debilitating, then it may be time to consider an antidepressant.
Antidepressants can do a great job in relieving symptoms of major depression, but you may not have success with the first antidepressant that you try.
You must also ask yourself if you’re truly a candidate for an antidepressant.
A person who simply feels a little down in the dumps may decide that it’s time to take an antidepressant, before trying very effective natural treatments such as rigorous (or even moderate) exercise, a change in diet, supplementation, as well as investigating possible physical causes of mental depression, such as side effects of prescription narcotics and a medical disorder like hypothyroidism.
For some people, antidepressants have been a godsend, especially for people for whom rigorous exercise (such as hormonal exercise) is not an option, or who are so depressed that they are not able to exercise, let alone attend behavior cognitive therapy sessions.
Clinical depression can literally keep a person in bed nearly 20 hours a day.
My mother had a bout with severe depression and it was a battle just to get her to SIT UP IN BED. Thus, exercise was way out of the question.
However, exercise is a great treatment modality for people with less severe forms of depression.
Though it make take a while for the effects of Cymbalta, Effexor, Zoloft and Paxil to kick in, don’t let this stop you from trying an antidepressant if all else has failed.
Wegmann continues: “Remission of mood symptoms is tougher. This may span over an 8-12 week period.
“This is due to the fact that depression is neurotoxic. Depression suppresses levels of a key neural growth hormone known as BDNF (brain-derived neurotrophic factor), leading to the eventual death of neurons in critical memory and reasoning areas of the brain, including the hippocampus and prefrontal cortex.
“Simply put, depression causes brain damage, and it takes 8-12 weeks for antidepressants, assuming they’re working for an individual, to aid in neuron re-generation and repair this neurotoxicity,” says Wegmann.
 Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmann is a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Getting Off Lyrica Without Problems: Minimize Side Effects

Getting off Lyrica may cause a number of discontinuation side effects. This drug is prescribed for the pain of fibromyalgia, and the nerve pain associated with diabetes and shingles.
Quitting Lyrica suddenly can result in withdrawal symptoms including insomnia, headache, nausea, diarrhea and flu-like symptoms.
“Some people withdraw from Lyrica without any ill effects,” says Joe Wegmann, psychopharmacologist and licensed clinical social worker, author of Psychopharmacology: Straight Talk on Mental Health Medications.
I didn’t know there were any serious problems in some people quitting Lyrica until I came upon this by accident on the Web.
This was several months ago, and I filed this information deep inside my mind and forgot about it.
But looking back, I realize that people on the forum reported that getting off Lyrica was producing some very nasty side effects.
But just how widespread is this? Wegmann explains, “These forum threads don’t report on alcohol consumption, illicit drug consumption, polypharmacy issues or associated physical illnesses — very important.”
All that the Web peruser sees are the complaints by the person trying to quit Lyrica. Yes, we don’t know about other variables that can make it difficult to quit this drug.
Nevertheless, it’s a wise idea to taper off this drug, because you don’t know if you’re going to be one of the unlucky ones.
Wegmann explains: “What seems to work with those experiencing a discontinuation syndrome with Lyrica is to place them on a low dose benzodiazepine regimen (diazepam or clonazepam), in conjunction with tapering the Lyrica downward at 50 mg per week.
“This is a safe, slow taper. Many taking doses of 300 mg per day are able to discontinue the drug within seven days without ill effects.”
Here’s a little irony: After I had forgotten about the Lyrica withdrawal information I had picked up on the Web, a neurologist gave my mother two bottles of 75 mg Lyrica capsules for nerve pain associated with carpal tunnel syndrome.
She was instructed to taper ON the drug, to build it up in her system: starting out with one 75 mg capsule in the morning for a few days; then one in the morning, one at night, for a few days; then two in the morning and one at night for a few days; and so on until maintaining on the full dose of two capsules, twice a day (total 300 mg per day).
The neurologist never mentioned anything about withdrawal effects of getting off Lyrica.
And interestingly, I never recognized this drug as the one that I had read about a few months’ prior in the forum, either.
So when about a week later, my mother wanted to quit this medication altogether (she had been up to 225 mg a day by then), because it wasn’t doing anything for the pain, I thought nothing of it.
She outright quit taking Lyrica, and had no withdrawal effects at all, though of course, she’d been on it for only a week as well.
If you’re on Lyrica, consult with your prescribing physician about how to taper off to minimize withdrawal effects.
 Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
Joseph Wegmannis a licensed clinical pharmacist and clinical social worker with more than 30 years of experience in the field of psychopharmacology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Chinnapong
Cymbalta Dizziness Withdrawal: My Solution Worked

Lessening your usual daily dose of Cymbalta can cause a thick kind of dizziness.
Cutting the dose down to wean off Cymbalta (for whatever reason) can leave a side effect of dizziness.
I witnessed it when my mother’s system suddenly was 60 mg less of Cymbalta. She had no choice but to get off Cymbalta because she changed insurance plans.
The new medical plan did not cover Cymbalta, so she got a prescription for Effexor, which belongs to the same class of drugs that Cymbalta does.
She was on 90 mg (three, 30 mg capsules) of Cymbalta per day, taken all at once every evening.
To make the transition smoothly to Effexor, she was instructed to take half a 75 mg tablet of Effexor in the morning, and then another half at night, with 60 mg Cymbalta.
She was to do this till she ran out of Cymbalta, which happened about a week later.
Her body didn’t even recognize the transition; she experienced no side effects from adding in the Effexor along with subtracting 30 mg of Cymbalta per day.
However, her body really recognized something was different when it was time to take one whole Effexor tablet in the morning, and one whole one at night, which was the step to take once the Cymbalta ran out.
The next morning, my mother was dizzy as can be, and couldn’t walk on her own. I knew it had to be from the final stage of the transition.
Because my mother had already been on the Effexor for a week with no side effects, why would increasing the Effexor dose cause so much dizziness?
On the other hand, her body was suddenly 60 mg less of Cymbalta, with NONE of this drug in her system at all at this point.
Thus, the dizziness had to be from Cymbalta discontinuation syndrome.
The dizziness dissipated when my mother sat leaning back, or was lying down. She lied down for an hour soon after getting up in the morning.
She felt fine lying down, but getting up brought the dizziness on full force. She was unable to get down the staircase without assistance.
She sat in a recliner chair and the dizziness diminished. When she sat upright, it returned. She was confined to the chair. She needed a walker to get to the bathroom.
I had an idea: Maybe this Cymbalta withdrawal dizziness had to be worked out of her system, and that wasn’t going to happen if she stayed in the recliner all day.
The dizziness was the only symptom. My mother said several times, “I feel great, except that I’m so dizzy.”
I told her to sit upright while watching TV, and let the dizziness work its way out.
She had napped in the recliner for a few hours and still, the dizziness persisted once she sat upright.
But I told her to continue sitting upright and see if the symptom diminishes. And it did.
I told her to walk around the kitchen a bit; I’d assist to make sure she didn’t fall.
Within a few minutes of walking, my mother reported that the dizziness wasn’t as bad. She then sat upright at the kitchen table.
She napped again in the recliner, and then I told her to walk around the kitchen island five times, and within a minute or so, she told me to let go of her; she felt that good.
She continued walking, and over the next five minutes, the dizziness dissipated even more.
She even did a little kitchen work, and continued staying on her feet. Not long after, the dizziness was completely gone.
A person’s first instinct, when hit with severe dizziness, is to lie down or stay reclined, and not to get up if this makes the dizziness worse.
That’s good advice if the dizziness is due to a medical problem, but in this case, it clearly seemed to be from getting off Cymbalta completely, even though she was now on a similar drug.
Effexor and Cymbalta belong to the same class of drugs, but on the molecular level, they are NOT identical.
For Cymbalta withdrawal dizziness, being up and about, and walking around, was obviously the key to resolving the problem.
IMPORTANT: The patient should walk around only with someone at their side in case they lose balance until they are sure that the dizziness is gone.
I believe that had my mother stayed put in the recliner, the symptom would have plagued her straight through to bedtime.
If you have Cymbalta withdrawal dizziness, see what happens when you do the very thing that you’d never think to do: walk around and do light housework.
However, make sure someone is right at your side at all times, ready to protect you from falling, as I did with my mother.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Five Ways to Prevent Injury from a Treadmill Desk

Learn about these five key ways to help avoid injury from the use of a treadmill workstation.
Though a treadmill desk will reverse the adverse effects of sitting all day on the job, the user can actually develop various injuries, but there are ways to prevent them.
According to Andrea Avruskin, physical therapist based in Las Vegas., here are five ways to avoid injury from a treadmill desk:
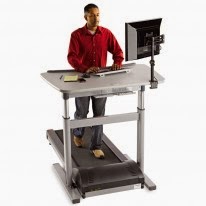
1) “Don’t walk too fast too soon.” Eager beavers will get on the unit for the first time and stay on much longer than they should, believing that walking 1 mph or even .7 mph for two hours continuously is harmless, especially if they already use a treadmill for exercise or briskly walk outdoors.
I’m a certified personal trainer. What people don’t realize is that very slow walking involves biomechanics that are quite different from those of faster walking.
This means that a person who normally does faster cardio exercise on a regular treadmill is not necessarily prepared to walk extremely slowly for prolonged stints. The result can be foot injuries that cause aching and pain.
Don’t stay on for longer than 30 minutes at first. At the first hint of foot discomfort, even if you’ve been on for only 10 minutes, get off.
Take your time working up to longer sessions on the treadmill workstation to avoid injury.
2) Avruskin says, “Use the treadmill desk for breaks from your sitting desk if using the treadmill desk all day long feels like too much.”
3) “Always use well-fitted sneakers that are appropriate for your foot type and are in good shape,” says Avruskin.
Wear your heels to work, but when it’s time to use the treadmill desk, wear walking shoes.
Injuries can be in the form of a blister. Another type of injury that’s avoidable is a corn.
4) Avruskin recommends a standing desk. “This is a perfect compromise between sitting and walking. Use a work surface that is as high as your elbows when standing.
Standing burns many more calories than sitting and keeps your muscles contracting while avoiding the distraction of constant movement of the legs.”
She adds that you should use an anti-fatigue mat and wear supportive shoes even though you’re only standing.
5) Avruskin also points out that a portable pedaler can be placed under a regular desk to keep the legs in motion without the injury risk that a treadmill workstation can invite, such as repetitive stress injuries to the feet or low back discomfort.
The bottom line with preventing injuries from a treadmill desk is to avoid rushing the process; don’t feel you must walk for six hours the first day you use the unit. Give yourself several weeks to get acclimated. Listen to your body.