How Painful Is Pronator Teres Syndrome?

Just how painful can pronator teres syndrome be?
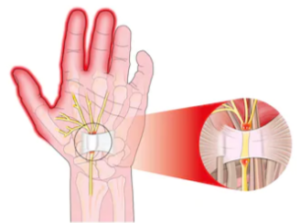
This condition is much under-publicized, and its symptoms can mimic carpal tunnel syndrome (CTS).
Any condition that involves a nerve can cause pain.
Pronator teres syndrome involves pressure on the same nerve that’s involved with CTS: the median nerve, a major nerve running down the arm.
“There are varying degrees of pain and paresthesias with pronator syndrome,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
And what is a paresthesia?
Paresthesia is a sensation of tingling, numbness, burning or prickling on the skin, often described as “pins and needles.”
It commonly occurs in the hands, arms, legs or feet and can be temporary from pressure on nerves, or chronic due to underlying conditions like nerve damage or circulatory issues.
Dr. Oheb continues, “With pain localized over the proximal forearm and paresthesias distally in the thumb, index, middle and half of the ring finger.”
Those finger locations are the same as with carpal tunnel syndrome. This is why sometimes initially, the physician will suspect CTS first.
The reason that the pain or discomfort of either pronator or carpal tunnel syndrome does not affect the entire ring finger or any part of the pinky is due to the distribution of the nerves branching out.
The branching distribution does not reach the muscles and nerves in those areas; thus, they are not part of the pain with these neuromuscular conditions.
Pronator syndrome is less common than CTS, but it can definitely cause pain.
CTS affects about 3-6% of adults, while pronator syndrome is relatively rare, though exact prevalence is unknown.
Estimates suggest pronator syndrome occurs at a rate 10 to 100 times less frequently than does carpal tunnel syndrome due to anatomical differences in nerve compression sites and more prominent symptoms.
“Pronator syndrome usually presents with pain localized in the proximal forearm which is made worse with repetitive prono-supination of the forearm,” says Dr. Oheb.
The pain can be bad enough to prevent strength training or household duties that activates that region.
The proximal area refers to that closer to the center of the body.
In this case it would mean near the elbow and inner portion of the forearm if you were standing with your arm hanging straight at your side.
Prono-supination refers to rotating the forearm from that of a palm-down position to a palm-up position.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Kristiana Gankevych
Carpal Tunnel vs. Pronator Syndrome: Symptom Comparison
Jonathan Oheb, MD, compares the symptoms of carpal tunnel syndrome with pronator teres syndrome.
“Whereas carpal tunnel syndrome is compression of the median nerve at the wrist, pronator syndrome is median nerve compression at the elbow,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
Symptom Comparison
“Symptoms similar to carpal tunnel syndrome include numbness, pain, tingling, burning in the thumb, index, middle and half of the ring finger.
“Differences unique to pronator syndrome include aching pain localized to the forearm, lack of night symptoms (seen in CTS), worsening with repetitive prono-supination, loss of sensation to the palm of the hand (due to a branch of the median nerve that comes off before the carpal tunnel).”
How a Doctor Can Tell Which One You Have
Doctors look at where the pain and numbness show up and what movements trigger them.
Simple exams and nerve tests help tell them apart.
Physicians use physical tests such as tapping over the median nerve, wrist-bending maneuvers and forearm resistance checks, along with nerve conduction studies (EMG), to see where the median nerve is being compressed.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Alexonline
Pronator Teres Syndrome Pain: Solutions
Dr. Jonathan Oheb provides solutions for when the pain of pronator teres syndrome strikes.
Pronator teres syndrome is characterized by compression of the median nerve as it travels through the forearm, typically at the level of the pronator teres muscle.
Though this condition hardly gets any media attention when compared to carpal tunnel syndrome, it sure can hurt at times.
Patients often experience pain, numbness or tingling in the forearm and hand, particularly in the areas served by the median nerve: thumb, index finger, middle finger and half of the ring finger.
There Are Several Options for Relief from Pronator Teres Pain
There are several options, according to Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Resting the forearm muscles, splinting to prevent forearm prono-supination, and nonsteroidal anti-inflammatories are the mainstay of conservative treatment for pronator teres syndrome,” says Dr. Oheb.
“This is continued for a minimum of three to six months before any surgery is considered.”
Prono-supination refers to rotating the forearm from palm-down to palm-up.
As your treating physician about splinting. A splint should still allow elbow movement.
But pain will be mostly prevented if the movement that causes it is stopped — with a splint.
Otherwise, consciously trying to remember to avoid rotating the forearm will prove difficult in day to day life.
For fast pain relief, the NSAIDs may begin working within 45 minutes, but don’t let this give you a false sense of security that you can then rotate the arm as freely as the other one.
The structure still needs rest from its function, which is where the splinting comes in.
For immediate relief of the pain, apply ice.
Sometimes the pain is in the form of a very annoying ache.
There may also be tenderness when the area is pressed with fingertips.
So when the pain of pronator teres syndrome is really dampening your day, remember the following five approaches for fighting off the discomfort:
- Rest
- Splinting
- NSAIDS
- Ice
- Physical therapy. Stick to your physical therapy assignments.
How well do pain pills work for the discomfort of pronator teres syndrome?
“Nonsteroidal anti-inflammatories help with pain as well as with decreasing inflammation and the secondary damage that inflammation causes to the nerve,” says Dr. Oheb.
NSAIDs include Ibuprofen, Naproxen and Meloxicam.
You need to be patient — yet dedicated with your conservative management of PTS.
Surgery for correcting the pain of pronator teres syndrome should be an option when all conservative approaches have failed.
The surgical procedure usually involves making an incision in the forearm to access and release the median nerve from the compressive structures.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ Kristiana Gankevych
How Normal Is Pain After Carpal Tunnel Release?

There are two explanations for pain persisting after carpal tunnel release.
What is a carpal tunnel release?
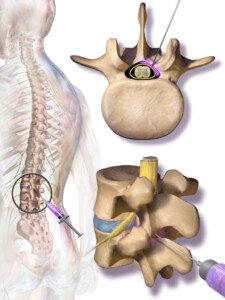
The median nerve and tendons pass through a narrow passageway in the wrist: the carpal tunnel, formed at the wrist bones on the bottom, and the transverse carpal ligament that goes across the top of the wrist.
The tissues will swell when this area is tight (or injured), causing pressure on the median nerve: hence the numbness and tingling, sometimes pain.
In the release procedure, the ligament that’s pressing on the carpal tunnel is cut, making more room for the median nerve/tendons to pass through.
- So why, then, can the pain, numbness and tingling continue after this procedure?
- After all, it seems like a pretty straightforward fix.
“Pain after a carpal tunnel release can be due to either persistent carpal tunnel syndrome or recurrent carpal tunnel syndrome,” says Jonathan Oheb, MD, Chief of Orthopedic Hand and Upper Extremity Surgery at North Valley Orthopedic Institute.
Dr. Oheb explains, “Persistent pain, in which the pain never improves after surgery, can often be due to an incomplete carpal tunnel release.
“This is differentiated from recurrent carpal tunnel syndrome in which the pain resolves and then recurs over the course of time as scar tissue that forms places pressure back over the median nerve.”
Scar Tissue Formation
This is not an uncommon complication after carpal tunnel release.
The carpal tunnel, having been snipped, triggers a healing response from the body, resulting in excessive scar tissue in some cases.
Nearby soft tissues then get bound together, and the skin nearby may feel tight.
Hand and wrist movement may feel restricted.
But that’s not all. The scar tissue can bind the median nerve and tendons, keeping them from smoothly gliding within the carpal tunnel. Pain is the result.
If the pain can’t be managed, then a second carpal tunnel release may be performed.
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik/krakenimages.com
Can One Bowel Movement a Week Be Normal?

If you’re having only one bowel movement a week, this can mean an obstruction, says gastroenterologist Sander R. Binderow, MD.
“It is important to also ask patients if they are passing gas if they have not had a bowel movement for a week,” explains Dr. Binderow, who’s with Atlanta Colon & Rectal Surgery.
“If the person has not passed gas nor had a bowel movement, then there could be an obstruction, and they should seek immediate medical attention if they have not already.”
Can one bowel movement a week ever be normal?
Dr. Binderow says, “If someone is not having bowel movements, but they’re passing gas, have no pain, are not nauseous – then they are probably constipated.
“Although they still may need medical attention, it is not immediate. Laxatives may help.”
This isn’t to say that being this constipated is normal.
But at least the presence of passing gas, and absence of other symptoms, point away from an obstruction as being the most likely cause.
More on Bowel Obstruction As Cause of One Bowel Movement a Week
“A patient with the above symptoms and no BM, especially if onset is sudden and acute, may have a bowel obstruction,” continues Dr. Binderow.
“They need to seek medical care immediately. Laxatives may further harm this situation.”
So will trying to “push” the constipation out by loading up on heavy, rich foods. This won’t push it out; it will only add to it.
Can a change in diet or a particular kind of diet cause a person to poop only once a week?
“Diet won’t affect this at all,” says Dr. Binderow.
And here is some striking news: Suppose you take laxatives and these produce a bowel movement—finally.
Do not make the mistake of thinking that this is a sign that “it can’t be cancer.”
Here is what Dr. Binderow says: “Laxatives may still work in a partially obstructing colon tumor. It does not point away from a tumor.”
If your constipation continues — even if you don’t have pain, nausea or even if you’re regularly passing gas, you should opt for a non-invasive, cancer colon screening exam such as Cologuard.

This can be done at your home and it “only requires following up with a colonoscopy if you receive positive results,” says Dr. Binderow.
Cologuard uses the latest in DNA technology to identify abnormal cells in your stools.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/sasha2109
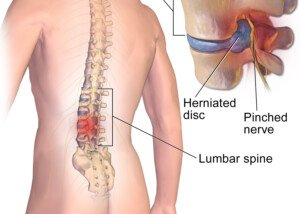
Does Housework Count As Physical Therapy for a Herniated Disc?

Huge mistake if you think your housework magically replaces the physical therapy you’ve been prescribed for a herniated disc.
You’ve been diagnosed with a herniated disc.
You had a session of physical therapy with a specialist, who showed you how to do the exercises at home.
After your first home session, you’ve decided that the exercises are a waste of time.
They’re boring and don’t even seem like they could help anything — mostly easy movements that don’t immediately make your sciatica feel better.
(Tip: You should wait about three weeks to determine if physical therapy works—and that’s only if you’ve been sticking to it faithfully, by the book.)
“Physical therapy is not just about movement,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“It incorporates using your muscles and increasing your flexibility through a set of engagements that are focused on a particular area. You aren’t going to get that in daily activity.
“You need to intensely focus on that particular part of your body.
“Physical therapy is designed to alleviate pain and strengthen and tone core muscles.
“And once you learn these modalities, you can do a lot of them at home.”
If you still believe that “all that housework” you do is just as good as any physical therapy exercises, then how come you developed a herniated disc in the first place?
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, pressfoto
Can Excessive Rest Interfere with Herniated Disc Rehabilitation ?

A spine doctor has bad news for those with a herniated disc who spend lots of time lying around, even if they do therapy exercises.
So you have a herniated disc and it hurts like mad. You do therapy or rehab exercises and do other things for pain management such as taking medications and using heat.
However, the recovery or rehab process will be hampered if you lead a sedentary life, even if you use the pain as an excuse to spend a lot of time in bed or in your favorite reclining chair.
“Yes,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“Studies show that bed rest is actually detrimental to you as far as recuperation from a back injury. I don’t recommend bed rest in any form for someone with a problem in their back.”
And you can bet on it, “sitting” way back in a recliner chair and watching TV counts as bed rest.
Dr. Perry continues, “Being very active, with little down time, is important. Don’t take specific hours of the day to lie down for back pain because inactivity is not good for the spine.
You need to be mobile. If you have neck or back pain, you should incorporate low-impact exercises such as walking, yoga and Pilates into your daily routine to help strengthen your core muscles.”
As a former certified personal trainer for a large health club, I never tire of telling people that HOLDING ONTO a treadmill while walking can potentially cause repetitive stress injuries in various joints, as this throws the body’s natural gait, spinal alignment and posture off-whack. Read more about treadmill incline walking and back pain.
It may seem counterintuitive not to take to sleeping off pain from a herniated disc, but all that sleeping or excessive lounging around will do is numb your awareness of the pain, or put your body in a position that helps conceal some of the pain.
But it does nothing for healing, zero for recovery. Get up and move! The human spine was designed for lots of movement, not inertia.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/fizkes
Are Epidural Injections Safe for the Elderly?

A doctor explains the safety of an epidural injection for the elderly patient including those with heart disease.
You may also be wondering if this procedure is done under general anesthesia (to guarantee the patient won’t move).
“General anesthesia isn’t required for an epidural injection,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“Typically, they can be done with local anesthesia. If the patient is very anxious, a light sedation can be used.”
Epidural steroid injections are usually administered to people who have pain from a compressed nerve at the location of their lower spine.
The irritation results in local inflammation. The drug that’s injected calms down this inflammation, thereby reducing pain.
Epidural injection. BruceBlaus/CC
Whether the patient is younger or elderly, these epidural injections typically last around three months, sometimes a little longer.
They are quite safe for an older patient, but what about one with heart disease?
Heart Disease in an Elderly Patient
“As it relates to heart disease, as long as the patient is in good medical health or being followed regularly by a doctor, an epidural injection is not very risky,” says Dr. Perry. “The problem comes in if the patient is on blood thinners.
“In this case, if you do an epidural, there is a risk of developing a hematoma (collection of blood), which can cause spinal cord compression and be very dangerous.
“Their doctor should ask if they’re on anti-coagulation/blood thinners before giving an epidural injection.
“For the most part, age doesn’t matter when it comes to epidural injections. And neither does the patient’s history of CABG.”
If anything is harmful to the aged person, it’s living with the pain that a compressed or “pinched” nerve in the lower back causes.
Pain is also not always the only symptom; there may be tingling, numbness and weakness in the leg.
The drug that’s used for an epidural injection is a corticosteroid.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Voronin76
Is One Bowel Movement Every 3 Days Normal?
Here’s what a gastroenterologist says about having one bowel movement every three days.
Some people have been led to believe that we “should” have one bowel movement every day—that it’s not normal to skip a day.
But some people have, on average, one bowel movement every three days. Is this normal?
“Normal bowel movements and normal bowel movement schedules range from up to three bowel movements per day and all the way to one bowel movement every three days,” says Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
He adds, “Not everyone has a bowel movement every day.”
Don’t panic if it’s been two days since your last bowel movement.
In fact, even if three days go by, there’s really no need to lose sleep. Dr. Binderow says that “a lot of people react to their bowel movements when they shouldn’t.
“If there is one incident of diarrhea, and then the person takes Imodium, and then they’re constipated so they take laxatives, they’re creating more of a problem than if they do not react to their bowel movement habits when any change occurs.
“If a person is concerned about a change in their bowel habits that does not return to normal within a few days, they should consult with their doctor to address their concern.”
What may seem like three days without a bowel movement might actually be two days if you’re a very busy person.
So it’s recommended that you track your bowel movements on a daily basis.
This way, over time, the picture will become clearer as to what is normal for you.
For example, what’s normal for me are what I call “doubles.” These are two days without a bowel movement.
It’s normal in that, though this is not a common occurrence, it’s also not what I’d consider rare or too unusual, either. It happens.
I could flip through my pages of daily trackings and see that every so often, a double comes up.
There’s even been a few instances of triples: three days without a bowel movement.
To ease any worries about your stools, you may want to have a non-invasive screening test for colon cancer called Cologuard.
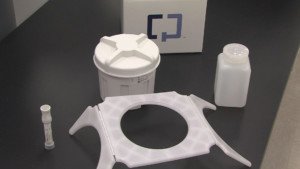
Cologuard uses up-to-date advances in DNA technology to identify abnormal cells in the stool sample that may be a sign of colon cancer or precancer.
 Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
Dr. Binderow performs minimally invasive, robotic and laparoscopic surgery for Crohn’s disease, ulcerative colitis, colon cancer and other colorectal conditions. Adept at routine procedures, he also sees patients with complex, atypical maladies.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Stool Texture vs. Black Tarry Color for Colon Cancer Sign
Just what is meant by “tarry” stools, and is texture important as a sign of colon cancer?
How often have you read that “tarry” stools are serious cause for concern and warrant a prompt visit to a gastroenterologist?
But just what does “tarry” mean in this context?
“Tarry black stool usually refers to a dark black color,” explains Sander R. Binderow, MD, FACS, FASCRS, with Atlanta Colon & Rectal Surgery.
He adds, “Until a bowel movement is truly black, there is no need for concern.”
Bowel movements can easily appear black in non-bright lighting, especially if the toilet bowl is stained from not having been cleaned in a while.
To get a clearer view of your BMs, you should remove some from the toilet and place on a white paper plate under good lighting.
If your vision isn’t clear with close-up views (i.e., you need reading glasses), then make sure your reading glasses are on.
If you still have problems with clear vision for up-close inspections, then inspect your stools without any visual aid — see if that yields a good clear view.
What appears to be a “tarry” stool may in fact just be a very dark green/brown or dark magenta/brown (from beets).
How important is stool texture as far as possible colon cancer?
Dr. Binderow says, “Texture rarely is addressed to determine any health issues because this can vary based on a numerous amount of conditions including your environment and what you eat or drink.
“People place much more importance on the texture of their bowel movement than is necessary.
“The color, if it is not dark brown or dark green and resembles the color of tar, is more of a concern and should be discussed with the person’s physician.”

Black stools
Tar is as black as black can get — ever see hot tar in liquid form in a vat before it’s laid on the ground?
The stuff is blacker than black — and stinks to high heaven, too.
Anyways, don’t get caught up with the texture of your stools, but rather, pay note of the color.
As for colon cancer, you’ll want to consider Cologuard, which is a non-invasive screening test for cancer of the colon.

Cologuard uses the latest advances in stool DNA technology.
It detects the changed DNA from abnormal cells in stool samples which could be associated with cancer or a precancerous polyp.