Black Hairs Growing on Breast: Causes

“If dark hairs suddenly appear on your breast,” begins Dr. Janet Prystowsky, a board certified dermatologist in New York, NY, with over 25 years of experience, “hormones are most likely the culprit.”
When women notice a black hair or two sprouting on their breasts, they want to know what could be the cause of this.
Dr. Prystowsky continues, “Many women experience dark hairs on their breasts, usually during periods of hormonal change like puberty, pregnancy or menopause.
“Generally this growth of dark hair (known as hirsutism) is harmless.
“However, there are some reasons to be concerned. Polycystic ovarian syndrome (PCOS) can cause unwanted hair growth, as it changes your hormonal balance.
“If you have PCOS or another hormone condition, you may also develop acne, problems with menstrual periods, trouble losing weight and diabetes.
“A tumor that releases male hormones could also cause these symptoms.”
“Check with your doctor to make sure that your black hairs are just part of your body’s normal hormonal fluctuations and not attributable to PCOS or another hormonally unbalancing condition.”
Here are the red flags for a tumor related cause:
Rapid onset of new hair growth, especially in adulthood.
Other virilizing signs: deepening of the voice, male pattern baldness, clitoral enlargement.
Irregular or absent menstruation
Abdominal pain

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
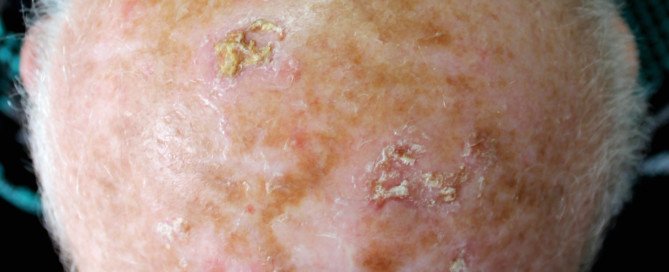
Can Scabs on Your Scalp Be Cancer?

Scabs on your scalp, even just a single one, can be cancer, says Dr. Janet Prystowsky, a board certified dermatologist in New York, NY, with over 25 years’ experience.
“The most dangerous scab you can find on your scalp is from skin cancer,” she says.
“Any scabbing condition on the scalp that does not respond to usual treatments within a month should be re-evaluated and potentially biopsied.
“Skin cancer of the scalp (including melanoma, basal cell carcinoma and squamous cell carcinoma) is frequently mistaken for one of the more common scalp problems.
“Delay in diagnosis leads to a larger and more serious skin cancer.
“Even though hair should be able to protect the scalp from the sun, frequently skin cancer may appear in part lines or areas where the hair was cut short during childhood. It can occur anywhere on the scalp, however.”
Squamous cell carcinoma, like basal cell carcinoma, is intimately linked to cumulative sun exposure.
This is why this cancer typically appears in areas that have received heavy exposure to the sun.
Balding men are especially prone to these non-melanoma skin cancers unless they’ve habitually worn hats or sunscreen on their scalps when outdoors.
Basal cell carcinoma is the most common cancer in the world, and the most likely cancer to grow on a scalp.
This cancer, which is almost always non-fatal, will start looking scabby if left untreated for long enough.
They are slow growing and can easily be brushed off as nothing to worry about in their early stages, especially if they’re located where a person would not readily see them, such as on the scalp.
A squamous cell carcinoma is more dangerous, in that it can metastasize to distant parts of the body. These, too, can look like a scab.

Actinic keratosis; Source: skincancer.org
A precancerous condition called actinic keratosis often develops on scalps that have received a lot of sun exposure over the years.
If left untreated, these can start looking scabby (though predominately red/pink).
About 10 percent of these atypical growths, if left untreated, morph into squamous cell carcinoma — which can be fatal.
The American Cancer Society estimates that squamous cell carcinoma kills about 4,000 people in the U.S. every year.
This is why if you see any kind of scab development on the scalp that has a progressive nature — get it checked by a dermatologist.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Dermatology11
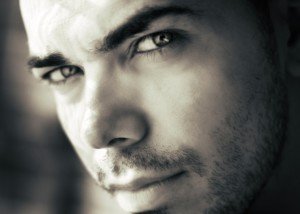
Bumps on Penis: Types, What They Mean
If you have strange, itchy or hard bumps on your penis, there is a particular type of doctor who will have excellent insight into what can be going on.
And that is a dermatologist. This is because the penis is covered with skin.
Disease processes or infections can manifest themselves in the skin, and a dermatologist can determine what that disease process or infection is.
Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience, cites a variety of causes for “bumps” that can appear on the penis.
Clear Bumps
In about 10 percent of men, these are normal “and are nothing to worry about,” says Dr. Prystowsky.
Single Hard Bump
If this appears to be just beneath the skin, it “could be a harmless cyst,” she says. It should be taken out or drained.
Cluster of Blistery Spots
This may be herpes. If not treated they’ll eventually burst and become scaly and red.
There are at least three more reasons for the development of bumps or spots on the penis, and one can lead to cancer, says Dr. Prystowsky.
If you have any bumps on your penis, even if they’re small and don’t itch, it would be a smart idea to make an appointment with a dermatologist rather than with a primary care doctor.

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Syda Productions
Penis Bumps, Spots and Dots Guide by a Doctor
Here is a DOCTOR’S explanation for the many causes of different bumps, dots and spots on your penis and what can be done about these.
Forget the forums with laypeople’s explanations for why you have tiny red bumps or white bumps or dots or spots on your penis.
You may think that this problem belongs to a urologist, but the penis is covered with skin, and anything that goes on with the skin falls under the specialty of dermatology.
The Many Different Kinds of Bumps, Dots and Spots on the Penis
“Some dots on your penis may be perfectly normal or harmless,” says Dr. Janet Prystowsky, board certified dermatologist in New York, NY, with 30+ years’ experience.
“Others on the other hand may be sexually transmitted diseases.
“Clear bumps around the penis head are normal for about 10% of men and are nothing to worry about.
“A single hard bump that seems to appear just under the skin could be a harmless cyst that should be excised or drained.
“A cluster of blistery spots, however, may be herpes. These red spots eventually burst and become red and scaly.
“Another infection, syphilis, looks more like a red, painless ulcer.
“Molluscum contagiosum is a viral infection that causes small pearly-colored bumps.
“Genital warts is another viral infection that causes small, rough bumps.”
Deadly Virus
“The HPV (human papilloma virus) causing the genital wart could be dangerous and lead to penile cancer, which can be quite serious,” says Dr. Prystowsky.
“The Gardasil vaccine is intended to help young men and women avoid infection with HPV.
“Also, oral contact with genital warts can lead to life threatening oral/throat cancer from certain bad strains of HPV.
“There are many reasons your penis may have a small bump.
It is important to make sure that if the bumps are infectious, they are treated before being spread to someone else.”

In combination with her focus on early skin cancer detection and removal, Dr. Prystowsky provides a wide range of revitalizing and rejuvenating treatments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
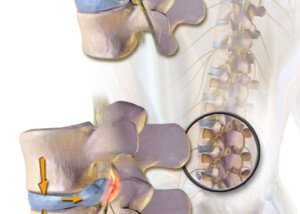
Can Dehydration Alone Cause a Bulging Disc?

A bulging disc in the lower back can cause low back pain.
Many people drink much less water than they actually believe.
For optimal health and well-being, getting enough water is crucial.
When a disc bulges, this means that the spongy, shock-absorbing tissue that’s between the vertebral bones juts or oozes out of its place.
This can irritate nearby nerves, leading to pain or aching in the low back. The discomfort may radiate down a leg or include tingling.
Not Enough Water
To avoid dehydration, you should not wait until you’re very thirsty.
In fact, dark yellow, and especially orange, urine is an indicator that you’re not adequately hydrated — even if you do not feel thirsty.

Shutterstock/gritsalak karalak
Is there a connection between dehydration and a bulging disc?
“Yes, dehydration can cause a bulging disc,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
It’s hard to believe, but true: Not drinking enough water can lead to a bulging disc.
“As most people know, the body is made up of 67 percent water, and some of that water is stored in the spine,” explains Dr. Perry.
He continues: “Our spinal discs are composed of two parts: annulus fibrosus —tough circular exterior composed of collagen fibers, and nucleus pulposus — inter core with a loose network of fibers suspended in a mucoprotein gel.”
The discs are shock absorbers. Dr. Perry explains that “about 75 percent of the pressure applied to the disc is on the nucleus pulposus.
“When the discs become dehydrated, the pressure is no longer on the nucleus pulposus but spreads throughout the entire disc.
“When pressure spreads to the annulus fibrosus, you can get cracks or bulges.
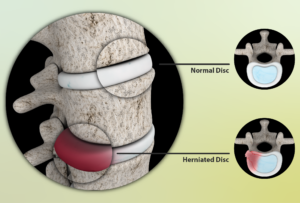
Source: myupchar. com
“This can also create pressure on the nerves and lead to other issues such as leg pain caused by sciatica.”
Dr. Perry adds, “Another interesting thing to note is that when we’re up standing or walking all day, we put enough pressure on our discs that can cause some people to even lose one-forth inch of height between when they wake up and go to bed.
“This is due to pressure and compression causing dehydration of the discs.
“When you lie down at night, the discs have time to extend and intake water. The discs are more likely to expand and the cushion effect becomes more apparent during rest and sleep.”
To make drinking eight to 10, eight-ounce glasses of water every day more feasible, make homemade lemonade, drink tea or add some water to your morning orange juice.
Soda never counts as water. Snack on cucumbers, watermelon and tomatoes, which have a high water content. Drink water with your meals instead of juice, soda or milk.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Miss Ty
Drinking Water for a Bulging Disc for Recovery
Dr. Michael Perry, MD, says that drinking water is very crucial for recovering from a bulging disc.
A bulging disc also goes by the terms “herniated disc,” “lumbar herniation” and “lumbar pinched nerve.”
“It is important to drink between eight to 10, 10-ounce glasses of water per day to maintain hydration,” says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“If you’re outside or working in a hot and humid environment, it is important to increase this volume before you start to work.
“It makes a significant difference when you consume more water before you become thirsty; that way your body never becomes dehydrated in the first place.
Why Water Is Important for Treating a Bulging Disc
“Maintaining hydration combined with decreased force on the spine when lying down can help the discs reabsorb some of this additional water,” says Dr. Perry.
“This isn’t proven, but it may help prevent further bulging or even make the existing bulging less significant.”
Consider plentiful daily water intake as part of your conservative treatment for your herniated disc.
How to Fit in Eight Glasses of Water a Day
• Every morning, fill a pitcher with at least 80 ounces of water. Hopefully you already know there are eight ounces in one cup.
• The pitcher will be your supply for the ensuing day and evening.
• Drink only from the pitcher for a very easy way to track your intake.
• Replace soda and sugary juices with the water.
• Make it a point to have a glass first thing in the morning before you do anything else.
• Tea, coffee, soda and alcohol do not count towards your water intake.
• If you can’t drink water unless it’s chilled, and you’re struggling to drink 80 ounces throughout the day, you should try room-temperature water, as the lack of chill should make it go down faster.
• Give this plan some time to work towards improving your bulging disc.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: myupchar. com
Time It Takes for Lifting Weights to Bulge a Disc
“It could take seconds, or it could take years,” for weightlifting to cause a bulging disc, says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
I was inspired to write this article after the fitness director of the health club, where I used to be a personal trainer, walked in one day with a slow, tentative gait. I asked him what was wrong and he said, “I blew out a disc leg pressing.”
Dr. Perry explains, “Typically, anyone who uses their back in any type of physical activity will have generalized wear and tear. With that, the disc and spine will become degenerative over time and that, in itself, can cause a bulging disc.”
In the fitness director’s case, it took seconds: a single, acute event.
Though the floor leg press machine is supposed to stabilize the back (and it does, relative to the instability of the back squat and deadlift), the lower spine can also be subjected to high levels of stress if you’re straining from a very low position to push up a very heavy sled.
If your butt is off the seat at this point, this makes those lumbar discs even more vulnerable.
This is why I recommend that if you’re going to press from a very low position (knees by armpits), to use no more than a moderate amount of weights, e.g., that which you can press for at least eight reps.
Dr. Perry continues, “Chronic condition: A former acute injury to the spine can accelerate the degenerative process. If you have an acute back injury, 10 years down the road you may develop additional pain.
“This isn’t related to new trauma, but related to the injury from 10 years ago. That injury accelerated the degenerative process.
“Acute condition: If you’re a weightlifter, any time you apply pressure to your spine (whether you’re doing deadlifts, squats, bench pressing, etc.), you can herniate [bulge] a disc or cause nerve compression.
“In rare cases, this disc herniation in the lower back can cause cauda equina syndrome – when the nerve roots at the end of the spinal cord are compressed [causing paralysis, numbness, incontinence]. Cauda equina syndrome develops rapidly and is a surgical emergency.”
Does this mean avoid squats, deadlifts and leg presses because lifting weights might cause a bulging disc? Of course not.
Lack of weight-bearing exercise is far more dangerous, because the individual who never strength trains and then one day is helping a friend rearrange some furniture, shoveling snow or just leaning forward to pick up a potted plant…can “throw his back out” and require immediate medical attention.
Or, an extra-long session of housework or yardwork could render a non-strength-trained person in bed all day the next day due to back pain.
When lifting weights, you must use picture-perfect form, and to build strong or big muscles, you do NOT have to gun for the one-rep max.
But even if you do eight reps, you must pay strict attention to textbook form.
I see so many people performing deadlifts and back squats with lousy form; they risk getting a bulging disc.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
MRI vs. CT Scan for Low Back Pain: a Comparison

Low back pain is America’s No. 1 nonfatal health problem. An MRI, but also a CT scan, can tell a doctor a lot about what’s going on in one’s lower back.
The question though, is, which is better for diagnosing low back pain: an MRI or a CT scan?
For sure, from the patient’s point of view, the MRI sounds a lot better because it doesn’t emit the radiation that a CT scan does.
On the other hand, those with claustrophobia would rather undergo the CT scan than be “inside a tube.”
Patients who don’t want to feel trapped inside a tube can also inquire about the possibility of an “open” MRI.
An open MRI has wide sides and open space around the body, not a tight tunnel, allowing more visibility and airflow.
Low Back Pain: MRI vs. CT Scan
“The best test to obtain when looking at the spine is an MRI” rather than the CT scan, says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
“These scans are the best for soft tissues, such as your spinal nerves, disc, cord and ligaments,” continues Dr. Perry. “An MRI will allow your doctor to see cord and nerve compression.”
That’s not the greatest news to those who fear enclosed spaces and don’t care about radiation.
But it’s really good news because you should be concerned about radiation, and the MRI is truly superior at imaging the causes of low back pain.
So if you’re scared of being inside a tube, remind yourself that the MRI equipment does not emit radiation, and the CT scanner does.
“When you may have a bone issue, such as a hairline fracture, spurring or arthritis, a CT scan is the best test to obtain,” says Dr. Perry.
“A CT scan is preferable if you have a pacemaker, defibrillator or morphine pump. When you have one of these implanted devices, an MRI scan is contraindicated because of the MRI’s ability to interfere with the functions of these devices.”
If you’re scheduled for an MRI due so low back pain, bring good earplugs with you, as this machine produces loud knocking noises throughout the procedure.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Can Prolonged Sitting on the Toilet Cause Sciatica?

Yes, sitting a long on the toilet and reading can cause sciatica, says a spine doctor.
It may seem benign — sitting on the toilet for extended periods and reading, talking on the phone, texting, what-have-you — but this can lead to sciatica, says Dr. Michael Perry, MD, member of the North American Spine Society and American College of Sports Medicine.
In sciatica, the sciatic nerve is irritated. One cause of irritation is pressure against the nerve.
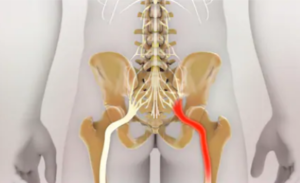
Sciatic nerve. Shutterstock/Nathan Devery
This can easily be caused by extended time sitting on a toilet, especially if the seat is hard — which it typically is.
The leaned-forward position that most people assume adds even more pressure on this major nerve.
Have you ever developed a numbness and tingling along your hamstring group after sitting on a toilet for a while? That’s the sciatic nerve being imposed upon.
“When you are sitting down, whether it is on a toilet or in a chair, you are applying more pressure to your discs than when in any other position,” says Dr. Perry.
“Some people tend to pull out a newspaper or a magazine while leaning forward on the hard toilet seat for an extended period of time.
“If that person also has an underlying disc abnormality, this significant and extended pressure can cause further deterioration.
“You may begin to experience shooting pain, electrical shocking pain or numbness because of this increased pressure while sitting in this position.
“If someone has a disc abnormality and they do feel this pressure and increased sciatica symptoms, it should be treated.
They should remain cautious and alert of sitting on the toilet for an extended period of time.”
If you cannot help but spend a lengthy amount of time on the toilet due to a major bowel movement or constipation, then try your best to periodically lift the affected leg off the seat to help relieve some of the pressure on the sciatic nerve.
 Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
Dr. Perry is chief medical director and co-founder of USA Spine Care & Orthopedics, and is frequently sought out for his minimally invasive spine surgery expertise.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Viacheslav Nikolaenko
sscpywrt26
Can Excessive Walking Cause Knee Bursitis?
If you already have bursitis in your knee, then it stands to reason that excessive walking will make you aware of it.
But this doesn’t mean that a lot of walking actually causes bursitis in the knee.
We live in a society that’s so sedentary that a lot of walking is viewed as something potentially harmful, when in fact, lots of walking is exactly how the human species survived and flourished. The problem is all the sitting that we do.
But let’s get back to bursitis of the knee. Something causes this when people have it.
Bursitis doesn’t just happen. A bursa is a fluid-filled sac (it’s supposed to be filled with fluid).
“The knee joint contains several bursae, which can be grouped by location into the medial, lateral and frontal bursae,” says Devin B. Peck, MD, owner of Austin Interventional Pain in Austin, TX.
Medial means inner; lateral means outer; and frontal means front.
“There are five medial bursae, four lateral and five frontal bursae,” continues Dr. Peck.
Causes of Bursitis in the Knee
“The most commonly-affected by inflammation leading to bursitis are the suprapatellar and pes anserine bursae. Pes anserine bursitis results from overuse and is common in runners.”
Now you might be thinking, if bursitis is common in runners, why wouldn’t a lot of walking be a cause?
This is because when we do a lot of walking, it tends to be for the sake of either transportation (such as a lot of walking on the job) or non-hard-impact exercise (fitness walking).

When bursitis is caused by running, it’s because the patient has been running way beyond that required for transportation or general fitness.
In other words, the patient has likely been training for long-distance running events or breaking personal record sprint times over short distances, which may include hurdling.
The patient may also have been running only in the name of fitness, but logging five miles at a grueling pace on hard concrete every single day. That’s still a lot of running.
This kind of running is not what ancient hunter-gatherers did for survival.
Sure, they jogged, but it was for transportation over natural terrain, not marathon training on an asphalt street.
Sure, they sprinted, but only to catch their dinner or escape from danger, rather than over and over and over on an asphalt surface every day to break personal record times.
Bursitis in the knee isn’t always caused by running, but if you’ve been diagnosed with it, it’s extremely unlikely it was caused by walking.
Dr. Peck also says, “It may lead to pain and a discrete area of tenderness over the medial tibial condyle, the bony protuberance on the inner aspect of the lower knee.”
 Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
Dr. Peck’s areas of interest include chronic and acute musculoskeletal pain, sports injuries, arthritis and cancer pain, among many others. Austin Interventional Pain was established in 2019.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.