Can Stabbing Sciatica Pain Affect only the Butt?

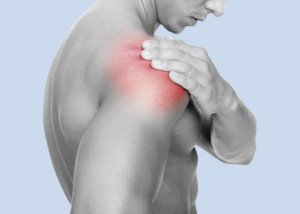
If you have a stabbing butt pain only, can this be caused by sciatic nerve problems?
Imagine walking around in the house or at a store, or standing in line, when suddenly a stabbing pain surges through your rear-end.
This happens from time to time, and there are no other symptoms. The pain occurs only in your buttocks.
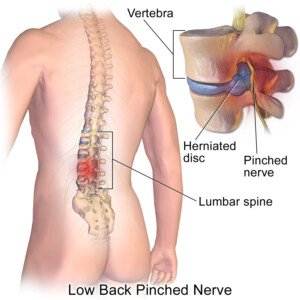
“Stabbing-type sciatic pain indicates the sciatic nerve has been pinched, which can be caused by acute injury or repetitive micro-trauma,” says Dr. Jeff Langmaid, DC, founder/owner of The Evidence Based Chiropractor, LLC, in Tampa, FLA, a research-based marketing and practice growth company that serves thousands of chiropractors across the world.
“It doesn’t have to be limited to the buttocks,” continues Dr. Langmaid.
“It can carry down to the leg, then calf and down to the foot. Sciatic pain can run across through the entire sciatic nerve, although some patients only feel it in one or two places.
“It doesn’t have to just be pain, but can include burning, tingling and the electric leg shock. Sciatic nerve pain is often felt as a result of a lumbar disc herniation.”
A stabbing type of pain that comes on suddenly, whether it is only in your behind, only down a leg and especially both in the butt and leg, is highly suspicious for a pinched or compressed nerve.
This includes the sciatic nerve — a major nerve that runs down the butt and leg, all the way to the foot.
As mentioned, a lumbar disc herniation is the usual cause. The disc bulges out and compresses or “pinches” a nerve that comes out of the spine. The affected nerve is not necessarily the sciatic one.
As for sciatic nerve compression, this can also be caused a little further down in the buttocks by a tight piriformis muscle.
If this muscle presses upon the nerve, it can induce pain, tingling or numbness.
Stretching and strengthening exercises (see below) can help relieve the condition.

Hip extension for the butt.

Stretch for the piriformis muscle. Shutterstock/Maridav
 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Miss Ty
Can Specific Exercises Increase the Risk of a Herniated Disc?
If a spinal disc might easily tear in some people, could certain exercises raise the risk of a herniation?
A herniated disc is when disc material bulges (herniates) out from the spinal column. This puts pressure on nerves.
“At times, our discs can withstand tremendous load and at other times, they can tear like tissue paper,” says Dr. Jeff Langmaid, DC, founder/owner of The Evidence Based Chiropractor, LLC, in Florida, a research-based marketing and practice growth company that serves thousands of chiropractors across the globe.
“They are very strong in some planes of motion and very weak in other planes of motion.
“Exercises that have both twisting and loading are very challenging to a disc and can increase the likelihood of an injury to the disc.
“Some of these exercises may include straight leg raises, deep knee bends or the wood chop, to name a few.”
Exercises that Simultaneously Involve Some Degree of Twisting plus Loading
- Walking lunge while holding a weight and twisting to one side with each step.
- Renegade row (pushups alternating with a dumbbell row)
- Bent-over dumbbell row (most people do twist somewhat when doing this).
- Any oblique-twisting exercise against resistance
- Some yoga routines
If you’re doing something at the gym that involves simultaneously twisting and loading, you may want to rethink your perceived need to do this particular exercise if you’re concerned about a disc herniation.
There actually is no need to simultaneously bare heavy loads and twist, whether your goal is to lose weight, gain muscle or achieve a certain appearance to your physique.
Unless you’re training for a wood chopping competition (and yes, “timber sports” have wood chopping events), do not combine twisting with load bearing.
Also be mindful of what seems to be linear movements that are heavily loaded, such as the leg press.
I knew a fitness director at a gym who “blew out a disc” (herniated it) when he went down very deep in the leg press apparatus, causing his lumbar area to leave contact with the apparatus, while attempting to press up a very heavy load.
 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: BruceBlaus/CreativeCommons
Can Cardio Exercise Prevent Sciatica?

Sciatica is a cause of sudden attacks of severe pain that can shoot down the leg, often starting in the butt.
Cardio exercise is something that you should strongly consider if you’re determined to knock down your chances of ever developing sciatica.
This disorder is very common and involves pressure at some point along the higher portion of the sciatic nerve.
This major nerve extends down the buttocks, continuing down the upper leg and then lower leg.
Cardio Exercise and Sciatica
“Cardio exercise has the potential to indirectly limit or prevent sciatica,” says Dr. Jeff Langmaid, DC, founder/owner of The Evidence Based Chiropractor, LLC, in Tampa, FLA, a research-based marketing and practice growth company that serves thousands of chiropractors all over the world.
He continues: “If you have good cardiovascular fitness, chances are you are maintaining a healthy weight and are staying active.
“Both of those are key contributors to not only preventing sciatica, but overall health and wellness.”
Sciatica does not just happen.
The key is consistent, structured exercise, not irregular or inconsistent bouts of physical activity.
- This means that the periodic pickup basketball games do not count.
- Neither does housework.
Dr. Langmaid continues, “Additionally, many cardiovascular exercises can contribute to core strength and stability.
“For instance, a seated rowing machine is a cardiovascular activity, but provides a strength training component with it that can go a long way towards preventing sciatic pain.
“There are also certain cardio exercises and activities that can increase our flexibility, and the combination of core strength, flexibility and cardiovascular endurance is best together for preventing or limiting sciatica.”
Proper Use of a Treadmill
Walking is a form of aerobic exercise — when done with enough intensity to get the heart rate elevated.
If you use a treadmill, do not hold on. This interferes with natural spinal alignment when walking.

Shutterstock/Khakimullin Aleksandr
When the spine is concerned, you do not want anything less than correct biomechanics when conducting cardiovascular exercise.
If you feel you’re going to fall off unless you hold on, then slow the speed or lower the incline.
Swing your arms so that your upper and lower body move the way nature intended.
In addition to doing consistent cardio activity to help prevent sciatica, you should employ the exercises depicted below.

Freepik.com/yanalya

 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Does Slow Walking on a Treadmill Desk Stiffen Your Back?

Have you found that walking even just one mph on your treadmill desk after 30 minutes leaves your low back feeling oddly stiff? What’s going on here?
A chiropractor explains why slow walking on a treadmill desk can cause lower back stiffness.
“Our bodies are built for motion and perform at their best when we have adequate movement throughout the day,” says Dr. Jeff Langmaid, DC, founder/owner of The Evidence Based Chiropractor, LLC, in Florida, a research-based marketing and practice growth company that serves thousands of chiropractors all over the world.
“The intensity or duration of motion is going to depend on the individual.
“If you have health challenges such as a cardio-pulmonary disorder, you may be recommended a low-impact activity that is consistently done throughout the day.
“Other patients might be more apt to do some brisk, high-impact exercises five-to-seven days per week.
Of course the gold standard is to be active each day. Elevating your heart rate is important for cardiovascular fitness.
In terms of low back pain, I advocate for continual motion each day.
Whether it is high-impact or low-impact will depend on the physical condition and health history of each patient.
It is always best to consult with your trusted health care provider before beginning an exercise routine.
Even the highest level of athlete has a threshold of activity where tissues are pushed too far and injury can occur.
In short, both high-impact and low-impact activity can be beneficial.
It depends on the specific individual and if they’re experiencing any other challenges or pain. Both are certainly better than no exercise at all.
 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/stefamerpik
Can Sciatica Cause ONLY Pain?
How is it possible that sciatica can cause only pain and no other symptoms like numbness or tingling?
“Symptoms of sciatica can vary,” begins Dr. Jeff Langmaid, DC, founder/owner of The Evidence Based Chiropractor, LLC, in Florida, a research-based marketing and practice growth company that serves thousands of chiropractors across the globe.
. Patients can experience burning and pain, numbness and tingling. Symptoms can vary by person depending on where the nerve is injured or affected.
“There are different points along the sciatic nerve where they can be affected. Even within the spine, there are different tissues or structures that can affect the nerve roots which become the sciatic nerve.
“Your symptoms will be based upon the place of compromise and structure causing compression or injury. So that is why different patients may have different symptoms.”
Sciatica Can Affect Even the Foot
Compression of the sciatic nerve at the spinal cord level can actually cause symptoms in the foot on that same side.
A condition called “foot drop” can result. The foot drops when a person walks. There is difficulty flexing the ankle joint, as you would when putting on a pair of socks.
There’s nothing wrong with the foot itself. The problem originates near the spinal cord where the sciatic nerve is irritated.
This is an issue of foot weakness rather than pain. If a person has pain in only one area of the body — the foot — then sciatica probably is not the cause.
Sciatic pain typically presents in the low back, buttocks and/or upper leg.
Sciatica Treatments
Rarely is surgery needed. There’s a host of conservative treatments that have proven very effective, sometimes resolving the issue in a matter of only several weeks.
These consist of medications, physical therapy exercises, stretches and epidural injections in the low back.
In summary, don’t ever say, “This pain can’t possibly be from sciatica because there’s no tingling or numbness.”
 Jeff Langmaid, DC
Jeff Langmaid, DC
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/aceshot1
sscpywrt26
Here’s WHY an Energy Drink May Cause a Heart Attack

WHY are energy drinks suspected as a cause for heart attacks in some people?
Don’t assume it’s the caffeine. How often do you hear of people dropping from heart attacks because they drink five cups of coffee a day?
But something else is going on when it comes to energy drinks and a heart attack.
The QT Interval
There is something called a QT interval on an EKG (the test that prints out your heart rhythm).
The QT interval is corrected by a formula to correspond to the heart rate at the time of the EKG. This is called the QTc.
There is a normal range for the QTc, and it’s calculated in milliseconds.
A QTc longer than this millisecond range will get a doctor’s attention — depending on the patient’s medical history, symptoms and medication usage — because QT prolongation can mean a higher risk of sudden cardiac arrest.
But a QTc outside the normal range can also mean operator error (the nurse putting on the EKG leads) and computer miscalculation from the EKG.
Other factors must be considered when noting a prolonged QT interval, such as personal history of fainting episodes.
Energy Drinks May Prolong the QT Interval
A prolonged QT interval means a highter QTc value. For some people this means a higher risk of sudden cardiac death, which may appear as a heart attack.
Why Energy Drinks Cause Apparent Heart Attacks
In one investigation (Shah et al), researchers took a look at the QT interval of 93 healthy people after they drank one to three cans of an energy drink.
An EKG showed that their QT intervals were 10 milliseconds longer than the limit for the normal range.
Now you may be thinking, “Only 10 milliseconds? How can that make a difference?”
Well, it does. Milliseconds count when it comes to how well the heart recharges for its next beat.
If it takes too long (again, measured in milliseconds), this heightens a person’s risk of ventricular fibrillation leading to cardiac arrest.
This isn’t a heart attack per se, but rather, the quivering instead of beating of cardiac muscle, making it impossible to pump blood throughout the body.
In general, a cardiologist becomes concerned when there’s an extra 30 milliseconds to the QT interval from baseline.
The Shah et al study showed that energy drinks can prolong QT interval.
There is a genetic form of this condition, called genetic long QT syndrome.
But even if the prolonged QT interval is caused by an extraneous agent, such as an energy drink, this anomaly is just as serious a concern and has the potential to cause heart problems.
The study also notes that energy drinks increase blood pressure, which certainly isn’t good for the heart.
Stay Away from Energy Drinks
A beverage with carbohydrates will provide you with energy. If you’re growing fatigued during sport or training, drink some regular juice or have a banana, peach or apple.
A so-called “energy” boosting drink is not necessary, even though these are marketed to athletes.
“Certain energy drinks can increase the heart rate significantly because they are stimulants,” says Yaser Elnahar, MD, a cardiologist with Hunterdon Cardiovascular Associates in NJ.
“If you have an excessive amount of stimulants, they can cause rapid heartbeat or even arrhythmias.
“There have been case reports of excessive energy drinks and heart attack — in which the researchers felt the excess intake led to low blood flow and clotting that led to a heart attack.
“There aren’t trials showing energy drinks cause heart attacks directly.”
 Dr. Elnahar has publications in the Journal of Atrial Fibrillation, the Journal of Clinical Medicine and Research, Reports in Medical Imaging, and more.
Dr. Elnahar has publications in the Journal of Atrial Fibrillation, the Journal of Clinical Medicine and Research, Reports in Medical Imaging, and more.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Yuttana Jaowattana
Source: sciencedaily.com/releases/2013/03/130321205524.htm
Can’t Rid Belly Fat Despite Cardio 7 Days a Week?

What’s REALLY going on when you can’t get rid of your belly fat despite doing cardio exercise seven days a week, week after week?
There’s a reason why the fat won’t budge.
And the stomach fat won’t budge even though your cardio exercise could be jogging, “power” walking, cycling or an aerobics class — and you’re even sweating and huffing hard.
But the excess belly fat just doesn’t want to depart from your body.
Something Interesting About Great Abs
Lots of cardio is not the best thing for ripping off belly fat.
Which type of athlete has the most buff body and tightest, trimmest waist? One such athlete is the sprinter.
Not that everyone should want to look like a competitive sprinter, but it’s the point I’m driving at:
It only makes sense that if you want to strip off belly fat, you must do some derivative of what these athletes do in their training.
The core of their training is that of alternating short bursts of output with a slower movement.
Sprinters will sprint hard, then walk around for several minutes before sprinting again.
Soccer players will run hard, and then there’s always that loll in the game or practice.
Rid Belly Fat without Cardio Every Day — but Only 2x/Week
As a former fitness trainer, I recommend high intensity interval training.
This is a form of cardio, though technically, it’s an “anaerobic” type of exercise.
It creates hormonal changes in the body that accelerate the fat burning process.
An example is dashing up several flights of stairs, then slowly walking back down thenm, maybe pacing around in the landing for another minute or two, then dashing back up the steps as fast as you can.
You only need to do this for six to eight cycles to create a significant belly fat-burning effect.
Twice a week will do, and you should strength train three times a week.
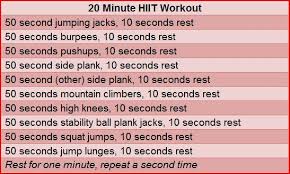
If you don’t add strength training to the mix, you’re shorting your body of optimal fat burning.
Stop doing cardio seven days a week, day after day, week after week–even hour-long sessions of “steady state” aerobics won’t do much for stubborn belly fat.
Do high intensity interval training (“HIIT”), and for best results add strength training.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/Suwan Wanawattanawong
Think Your Burping Is Caused by Angina?
Are all burps the same or can some be caused by angina?
Angina pectoris is the medical term for chest pain that results from reduced blood flow in the heart’s arteries.
Sometimes, shortness of breath accompanies an episode of angina.
The restriction of blood flow is caused by coronary artery disease: plaque buildup inside the heart’s arteries.
An uncommon form of angina is when the reduced blood flow results from a spontaneous spasm of these arteries (which has nothing to do with whether or not they are filled with plaque).
Burping with Angina?
“Burping is a very unusual presentation for acute coronary syndrome,” says Lance S. Burns, MD, emergency medicine specialist, of Legacy ER & Urgent Care, Frisco East location.
What is acute coronary syndrome? This is a category of pathological processes that result in a shortage of blood supply to the heart, usually caused by an arterial blockage (namely plaque buildup), but can also be caused by a spasm of a coronary artery as mentioned prior.
You may be burping during an angina episode, but this doesn’t mean that whatever’s causing the angina is also causing the burping.
Dr. Burns adds that “indigestion is a very common symptom for cardiac issues and frequently is ignored or confused with a gastrointestinal etiology.”
If you’ve recently gone to the emergency room for a complaint of chest pain — whether or not you were also burping — and you were told that there’s nothing wrong with your heart — you should absolutely follow up with a cardiologist appointment.
The ER doctor will order tests to see if a patient recently had a heart attack or has abnormal heart structure, pneumonia or a blood clot in the lung.
But these tests do NOT show if your coronary arteries are blocked, let alone how blocked they might be.
They also can’t rule out angina. Burping aside, your next move should be a full workup by a cardiologist.
 Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/TunedIn by Westend61
Why Are EKGs so Short, only Seconds?
Ever wonder how a short, eight-second EKG could tell a doctor about someone’s heart?
Lance S. Burns, MD, emergency medicine specialist, of Legacy ER & Urgent Care, Frisco East location, performs many EKGs in the ER as part of his profession.
I asked him why EKGs are so short and how they can provide enough information to doctors.
After all, if a person has an abnormal heart rhythm, there may still be long periods of time in between abnormal beats.
What are the odds that the abnormality will show during the eight seconds that the EKG is being taken?
Cardiologists and ER physicians are the two types of specialists who commonly administer the EKG.
Dr. Burns explains, “EKGs are not typically looking for arrhythmias. Therefore, unlike the longer rhythm strips or event monitors, the EKG need only be long enough to capture only several heart complexes.
“The EKG is looking at the electrical flow through heart muscle. If this is abnormal, it will be apparent in any one heartbeat.”
What can cause an abnormal electrical flow through heart muscle?
Blockage in a coronary artery is one possible cause, though an EKG is not used for the definitive diagnosis of coronary artery disease.
The gold standard of diagnosis for the so-called clogged arteries or blockages is the catheter angiogram, though other tests such as a cardiac stress test can indicate the presence of blockages.
Dr. Burns continues, “If the concern is trying to detect arrhythmias, then a much longer period of analysis (often days) will be needed.
“Certain arrhythmias, such as atrial or ventricular fibrillation, occur continuously and will be captured on an EKG, even with the short period of analysis.”
If a longer period of monitoring is needed, the patient can undergo a non-invasive placement just under the skin of an event monitor.
 Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/megaflopp
Sudden Brief Chest Pains: Heart or Other Cause?

What are the odds that sudden brief chest pains mean a pending heart attack or other heart problem like angina?
“Very brief chest pain is often non-cardiac, although this complaint requires an appropriate workup for proper evaluation,” says Lance S. Burns, MD, emergency medicine specialist, of Legacy ER & Urgent Care, Frisco East location.
A doctor wants to tell you that based on test results, your sudden brief chest pains are NOT being caused by a heart problem, rather than tell you this simply because the brief nature is not typical for pending heart attack or blocked arteries.
Dr. Burns continues, “Brief chest pain is often either chest wall or pulmonary in etiology, usually eluding a definitive diagnosis.
“The feeling of a ‘catch’ or sharp pain in the chest is very common and typically benign. The longer the pain lasts, the higher the possibility that there is a more concerning underlying etiology.
“Of note, pleurisy is a lay term describing sharp chest pain, which is worse with inspiration [inhaling] or movement.
“It is important to rule out potential life threatening diagnosis such as pulmonary embolus, aortic aneurysm, collapsed lung (pneumothorax), cardiac tamponade [collection of fluid] or coronary insufficiency.”
Sudden pain in the chest of very short duration can also be nerve or muscle/soft tissue related, stemming from a hard workout involving muscles and soft tissue in that region.
Make a note of when any sharp short chest pains occur. Is there a pattern? Are they usually the day after your chest workout or hardcore chin-up routine?
(Yes, the hanging and then pulling up causes stretching and isometric stress, respectively, on the chest muscles.) Muscle spasms can be brief and hurt quite a bit.
A ruptured or dissecting thoracic aortic aneurysm typically causes a ripping, excruciating chest pain —and it’s not brief, but it’s of sudden-onset. It’s life threatening and requires immediate medical intervention.
However, whenever anyone presents to the ER with chest pain, physicians will move fast to rule out the most serious possible causes.
 Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
Dr. Burns has over 30 years of experience, and he specializes in emergency medicine as well as family medicine. For more info: Legacy ER & Urgent Care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.