Chances of 89-Year-Old with Hip Fracture Fully Recovering

Are you panicking because a very elderly loved-one, 89, just fractured a hip? I know how you feel.
When my mother was 89, which is considered advanced elderly, she broke a hip after falling, but she’s actually in better shape now than she was BEFORE the injury! (more…)
One Knee Hurts when Squatting but Not Running, Jumping?

How do you treat pain in one knee when squatting but not when running or jumping?
Let’s assume there’s been no traumatic injury to the knee that hurts when you lower down into a deep squat—and I’m talking about a bodyweight-only squat–with both feet FLAT on the floor. (more…)
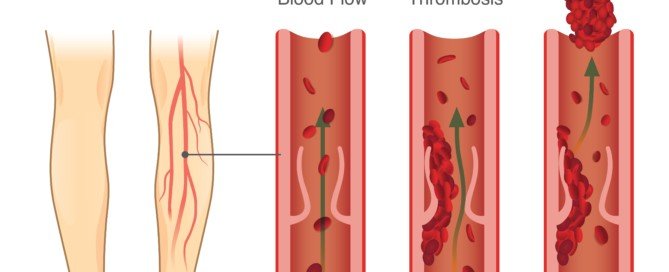
How Is a Long and Dense DVT Removed?
Not all deep vein thromboses resolve with the aid of drugs, especially when they are long and dense.
“DVT stands for deep venous thrombosis, which represents abnormal blood clotting in the veins, usually involving the lower extremities,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
Dr. Tavel explains, “The main problem originating from this disorder is the detachment of parts or all of these venous clots breaking off and landing upstream in the lungs, resulting in a potentially dangerous pulmonary embolus (PE).”
This is a blood clot in the lung that requires immediate treatment.
“The DVT itself will ordinarily resolve without the need for removal, and the treatment of this problem is aimed at preventing further clotting through the use of various anticoagulants,” says Dr. Tavel.
But sometimes a deep vein thrombosis is particularly dangerous: dense and long.
In 2013 a 62-year-old patient presented at the ER of Ronald Reagan UCLA Medical Center with shortness of breath and other symptoms.
A CT scan showed a two foot long DVT which began from his legs and went into his heart.
A clot busting drug was no match for this monster. The man’s doctor referred to the 24 inch long DVT as a “wad of gum in a pipe.”
Dr. John Moriarty told the patient that the only other options were open heart surgery or AngioVac—a vacuum procedure.
The patient chose the minimally invasive AngioVac. A week later he was back home.
How was this dense, very long DVT removed?
- A tiny camera went down the patient’s esophagus so that doctors could see his heart.
- A coiled hose was guided through his neck; one end of this hose was plugged into the patient’s heart, against the DVT.
- Then, the hose’s other end was threaded through a groin vein.
- Then the hose was hooked up to a heart-bypass device which created suction.
The AngioVac sucked up this ultra-long deep vein thrombosis from the heart. The device “filtered out solid tissue,” points out Dr. Moriarty in the report.
It “restored the cleansed blood through a blood vessel near the groin.” No need for a blood transfusion.
The procedure lasted three hours. The clot buster (tPA) would have taken three or maybe four days to work.
Here is more information on AngioVac — a mechanical means for the removal of fresh, soft deep vein thromboses.

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstsock/solar22
Source: sciencedaily.com/releases/2013/09/130918101437.htm
What Does “Shortness of Breath” REALLY Feel Like?

There’s many ways to describe “shortness of breath,” a common complaint among those fearing heart problems or GERD.
Shortness of breath can feel as follows: (more…)
How Weak Women Can Get Pushup STRONG!

Women will get stronger at pushups if they follow my no-nonsense strengthening plan–designed by me, a woman who does pushups very easily.
I was a personal trainer for five years at a gym and taught many women to do pushups.
And I mean REAL pushups, not the cheat kind (e.g., upper back jutting out, face jutting forward, tummy sagging).

Shutterstock/Slatan
I actually do pushups with my feet (not shins, but the tops of my feet only) on a high stool, while maintaining a straight line with my body from head to feet.
However, this is a very advanced way of doing pushups, but it’s just to assure you that my plan will definitely work for women wishing to get stronger at standard pushups.
Seated chest press machine. Women will develop stronger pushups by doing seated chest presses. The motion is actually a pushup angled upward by 90 degrees.

Shutterstock/Travelerpix
The advantage is that a woman, no matter how weak, will always be able to do seated chest presses.
Find a machine with handle widths that are similar to the width you’d place your hands apart in a pushup.
After two warm-up sets with light resistance (15-20 reps), increase the weight load so that 12 reps are difficult. Increase again so that you can barely do eight reps.
Eight reps should take it all out of you. Do two more sets at eight reps. How much weight this will require will vary from one woman to the next.
Flat bench dumbbell press. Lie on a flat bench and simply press upward dumbbells in each hand. Apply the same protocol as with the seated chest press routine.

Shutterstock/Catalin Petolea
Modified pushups. The reason I recommend seated chest press and flat bench dumbbell press, to get stronger with pushups, is that women usually struggle quite a bit with pushups. If all that women did were pushups, they’d quickly become discouraged.

hutterstock/Alexander_Safonov
To keep motivated and fired up, it’s important to perform other chest routines that you can actually do, and thus, feel good about, rather than, “I’m such a weakling!”
Nevertheless, to get stronger with pushups, women should also do these as well. Women will get stronger far faster if they modify pushups so that they can actually complete reps with full range of motion, as opposed to attempting to do military (or men’s) variations of the pushup.
I see women struggling like mad to complete just one military pushup, and after many months, they’re still struggling.
Instead, place your hands on a slightly elevated platform. This can be the round side of a BOSU board, or the flat side of the BOSU.

Shutterstock/sanneberg
If it’s the flat side, grip the edge of the platform so that your fingers are curled over the edge.
Now try pushups with only the tops of your feet on the floor, body forming a straight line from head to toe.
If you can’t, then modify further by placing your knees on the floor. Don’t bow down to the platform!
I see women, with knees on floor, bowing down all the time.
This is not a modified pushup at all. It’s bowing and will not increase your pushup strength.
If you can’t help but bow, then further modify by doing pushups in a standing position, hands either against a wall, or against a ballet bar or railing bar.
Place feet out away from the bar, put hands on bar, keep your body straight, and lean towards the bar.
Don’t bow towards the bar. Now push away. A very novice woman should be able to do repetitions this way. Do four sets, up to 12 repetitions.
Over time as you get stronger, move on to knee pushups with hands on elevated platform.
Along the way, you’ll notice yourself getting stronger with the other chest routines.
Don’t just keep using the same resistance. Every few weeks, increase it, always striving for those 12-rep, and then eight-rep, maxes.
If you have it in you to push yourself to complete muscle exhaustion, you need only do these routines once a week.
If you can’t push as hard as you know you can, then do these routines twice a week with several days in between.
For women to get stronger for pushups, they must employ pinpoint form: no sagging back or shoulder blades jutting out, and no pitching forward of the head in an attempt to touch your nose to the floor while the rest of your body lags behind. And, no bowing!
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com, drobotdean
Are Water Aerobics Enough for Heart Fitness?

Bad News—Water aerobics will do very little for heart fitness.
This isn’t vigorous lap swimming; it’s the so-called water aerobics, the classes you participate in with colorful implements… (more…)
How a Skinny Fat Woman Can Get Her Abs to Show
If you’re “skinny fat” or just plain thin but dream of having abs that show, there IS a way you can achieve this–and it’s not zillions of crunches, either.
Elderly People Doing Pushups vs. Wall Presses

Elderly people can learn to do “real” pushups instead of limiting themselves to wall presses. But–you should start out with wall presses. (more…)
Six Ways to Warn Your Child of Adults Asking for Directions

Do you know how to train your child to recognize the “I need directions” lure from pedophiles? (more…)
Will a Bullied Child Attempt Suicide if You Talk About It?

Are you afraid to bring up suicide to your depressed and bullied child out of fear they’ll get the idea to try ending their life?
Some parents, alarmed after reading about yet another victim of bullies who commits suicide, may still be afraid of broaching this topic with their own bullied child.
“It might put the idea in their head,” the parent might think.
But will bringing up the topic of suicide actually encourage a bullied child to carry out this action?
“No! This is an important issue because it has come up so frequently — particularly with cyber bulling,” says Dr. Marilyn Benoit, MD, Chief Clinical Officer and SVP for Clinical & Professional Affairs of Devereux, the largest not-for-profit behavioral healthcare organization in the country. Dr. Benoit has a family practice as a child and adolescent psychiatrist.
“Literature has shown a direct correlation between people who have suffered bullying in silence, and physical health and mental health impairments,” continues Dr. Benoit.
Parents absolutely must discuss suicide with a bullied child.
“Discussing suicide does not make someone want to commit suicide,” says Dr. Benoit.
“It actually does quite the opposite. It offers the child an opportunity to disclose how awful they are feeling — and gives parents the opportunity to let them know that thoughts of suicide are not bad – rather, they are an indicator of what someone is feeling, and that there are ways for the child and family to receive help.”
Be very careful how you tackle this topic, however. There’s the case of the tween boy who complained to his mother how miserable his life was.
She got mad replied, “Oh don’t give me that! You have it so much luckier than most kids, you don’t even KNOW how lucky you have it!
“I bet if you wrote down all the good things in your life and all the bad things in your life, you’d see that all the good things would outnumber all the bad things!”
That last recommendation may actually sound beneficial, but it had been spoken in a demeaning, angry voice.
HOW you sound, not just the words coming out, is very important.
“I do want to bring up the issue that bullying sometimes leads children to feel so awful and so perplexed that they feel that they want to kill themselves,” says Dr. Benoit.
She urges parents to be very open about this troubling topic.
“We need to let them know that it’s okay to talk about these feelings and talk about bullying.
“This will allow families and children to seek the help they need from mental health professionals.”
If your child is being bullied or harassed at school, then next time there’s new news about a bully victim who committed suicide (and unfortunately, there probably will be in the next few months), discuss the case with your son or daughter.
Get them thinking and brainstorming on what the victim could have done instead of ending their life.
 Dr. Benoit is past president of the American Academy of Child and Adolescent Psychiatry and has provided Congressional testimony on issues including child abuse, teen pregnancy and youth suicide.
Dr. Benoit is past president of the American Academy of Child and Adolescent Psychiatry and has provided Congressional testimony on issues including child abuse, teen pregnancy and youth suicide.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.