How Women Can Tone Muscles with the Leg Press Machine

Learn how you can really tone your loose muscles up with the leg press machine.
I rank the leg press very high on the list of exercises for toning the legs, yet most women don’t do this exercise. (more…)
Diseases that Sjogren’s Syndrome Is Often Misdiagnosed As

Sjogren’s syndrome is usually misdiagnosed several times before the patient gets the right diagnosis.
You may have Sjogren’s syndrome and not even realize this, despite having visited doctor after doctor to uncover what’s been happening with your body.
Sjogren’s syndrome is an autoimmune disease that can affect many different systems of the body, multiple organs and produce a menagerie of symptoms, ranging from annoying to moderate, to severe to life-threatening (though the latter is rare).
Though Sjogren’s syndrome affects two to four million Americans, it stands as one of the most misdiagnosed medical conditions, even though there are a variety of tests that can confirm its presence.
Because Sjogren’s syndrome produces joint pain in 80 percent of affected individuals, physicians who specialize in this condition are typically rheumatologists.
“Sjogren’s syndrome can be associated with a variety of autoimmune diseases including rheumatoid, lupus, thyroiditis, celiac sprue (disease), scleroderma, and even with non-rheumatic autoimmune diseases like autoimmune hepatitis, hepatitis-C, HIV,” says Ali D. Askari, MD, Professor of Medicine – Case Western Reserve University.
“Primary Sjogren’s syndrome (as opposed to secondary SS), however, is not associated with any of these and there are differential points in each case,” continues Dr. Askari, Chief, Division of Rheumatology – University Hospitals Case Medical Center.
“As opposed to rheumatoid arthritis,” says Dr. Askari, “the joint involvement is not symmetrical, nodules are formed less commonly, and destructive changes of bones are seen less likely.”
Women make up 90 percent of patients with SS, for reasons that are unknown.
This condition can affect any age group, but it’s rare in people under age 20. The mean age of SS onset is early to mid-40s.
Dr. Askari continues, “The specific radiologic changes and presence of sub-acute cutaneous nodules are more associated with rheumatoid arthritis.
“In lupus there is more involvement of the kidneys, the central nervous symptom — and although the ANA is positive in both, anti-DNA is more positive in lupus than in Sjogren’s syndrome.
“Although photosensitivity can happen in both conditions, the typical butterfly or malar rash (on the patient’s face) is more suggestive of systemic lupus.”
Celiac disease often leads to skin rashes, but the blood test for this will not show the antibodies for Sjogren’s syndrome. In addition, with celiac disease, diarrhea is far more common.
If you don’t get a celiac disease test, yet you have this condition, and you go gluten-free (completely!) for 30 days, then there should be a marked improvement in your condition.
Disease of the thyroid gland could be associated with Sjogren’s syndrome, says Dr. Askari.
“Conversely, primary Sjogren’s syndrome is associated with more frequent occurrence of thyroid inflammation, so-called Hashimoto’s thyroiditis.
“Neurological conditions such as MS particularly can be mistaken for Sjogren’s syndrome.
“More so, primary MS is being diagnosed in patients with Sjogren’s. Differential can be achieved by more frequent presence of specific antibodies in the blood in Sjogren’s syndrome and positive lip biopsy, but the lesions on the MRI of the brain are similar to identical in both cases.”
The lip biopsy would confirm a reduced production of the salivary glands (the lips contain your salivary glands), which is a hallmark feature of Sjogren’s syndrome.
“Finally, in some cases of primary Sjogren’s syndrome, the dry mouth and eyes are later manifestations, and some unusual neurological manifestations, cardiac or liver disease may be one of the first findings,” explains Dr. Askari.
“Additionally, the findings of dryness are not spontaneously expressed by the patient and mainly attributed to the age, use of drugs, etc., and they should be solicited.”
Update: As of April 2024, Sjogren’s syndrome is now known as Sjogren’s disease.
Dr. Askari’s special interests include diseases of the muscles, fibromyalgia, general rheumatology, lupus and Sjögren’s syndrome.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ fizkes
Sjogren’s Syndrome: How Common Is Joint Pain: Percentage Affected

Joint pain is one of the many possible symptoms of Sjogren’s syndrome, an autoimmune disorder in which dry mouth and dry eyes are the hallmark symptoms. (more…)
Why the Obese Should Avoid Sit-Ups

If you’re obese or have lots of weight to lose, stop doing sit-ups, and here’s WHY you need to avoid this useless exercise for fat loss. (more…)
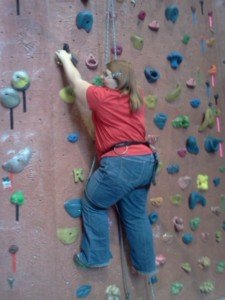
Wall Climbing for Plus Size Newbies GUIDELINES
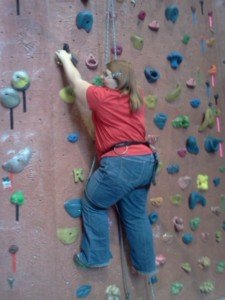
These wall climbing guidelines are specifically for fat or plus size women AND men who wish to pursue this very fun sport.
I used to do a lot of climbing, and though not overweight, I learned a lot in the four years I spent, week after week, climbing all sorts of wall routes.
I achieved a strong intermediate level of skill at top roping. This means that I was regularly top roping to completion, on a first attempt, new routes that were rated 5.10 (A, B and sometimes C).
I was able to work some 5.11’s on top rope, getting to the top (but never on a first try with a newly created 5.11 route).
I did lead climbing on some 10’s, a few 11’s. I also did all kinds of routes such as slabs, corners and overhangs.
Basic Climbing Guidelines for Overweight Beginners
First and foremost, don’t say, “I’m too fat to climb.”
If you’ve ever been in a climbing gym, you will have noted that routes are rated with numbers which usually go down as far as 5.4, maybe a little lower.
These are easy, and parents have their newbie children climbing them.
But they are also for adults who are new to this sport.
These easy routes consist of large, comfy hand-holds and foot-holds.
The issue, then, is stamina, even though a very overweight person may have difficulty just making a few successive moves due to their size.
But with grit and determination, it can be done, assuming that you are not so obese that you have difficulty just walking.
Expect to fatigue quickly. Don’t let this discourage you! After all, the human body is NOT designed to ambulate vertically. We are not squirrels.
You WILL fatigue very fast. Simply sit back in your harness and rest, then resume.
It may take an overweight newbie quite a while to reach the top of the gym’s easiest route, especially if it includes a slight overhang.
There is nobody timing you.
There is no time limit on the route.
If you need 20 minutes, then you take 20 minutes.
Consider it a workout routine.
Expect your forearms especially to quickly burn. This is because you’re using them in a way that you’ve never done before. This fast on-fire feeling also occurs to thin beginners.
The main reason you’ll feel your forearms going dead very quickly is because people who are new to wall climbing will invariably try to muscle up a route, especially a route with big hand-holds.
They will attempt to pull themselves up with their arms, letting their legs drag below them. This is not how to efficiently climb a wall.
However, learning the proper techniques will take time. Do not get in the habit of muscling up the route.
It is said that women climbers learn the techniques faster than do men because they lack the upper body strength to haphazardly muscle up the wall.
Body position, including that of the legs, is crucial for efficient wall climbing.
Even how you place your hand on particular hand-holds makes a big difference.
I can go on and on about the many very effective body movements that propel a person up a wall without any muscling-up, but let’s just keep the focus here on guidelines for overweight beginning climbers.
You will need to learn how to propel up with your legs. This will take time. But how strong must your legs be to learn leg techniques?
Chances are, your legs are already strong enough for most of the techniques.
The so-called loading and rocking-on of a leg are probably not one of them, but there are other lower body tricks you can do even if you’re overweight.
Do not try to muscle up the route. Otherwise you will become quickly defeated.
Choose easy routes to start off with, even if only kids are using them. Novice children flounder plenty on easy routes.
During your downtime at the gym, watch the movement patterns of experienced climbers. Compare them to struggling climbers. You will see a big difference.
If your feet are too large to fit into climbing shoes, then wear the thinnest possible sneakers (not running shoes or other athletic-type shoes)—but just the simplest house-type sneakers.
If you’re sketchy about attempting a top rope route, then start out with some “bouldering.”
Bouldering is more of a horizontal (or so-called traversing) style of climbing, where there’s no rope required, and you’re close to the padded floor.
Traversing or bouldering will strengthen your fingers, hands and other muscles, and give the newbie plus-size man or woman an opportunity to hone basic climbing skills.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Why Swimming Can’t Replace Lifting Weights

Do not fool yourself into thinking that swimming can replace strength training with weights. (more…)
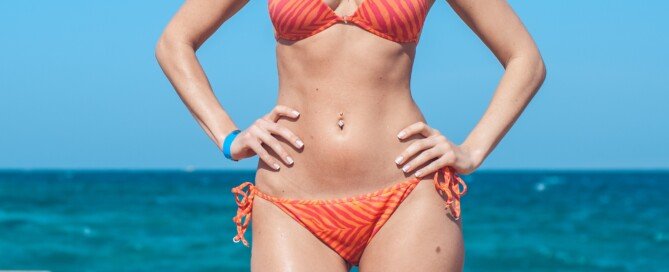
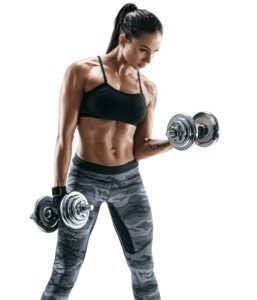
Solution to Super Wide Hips: Make Them Narrower in Appearance
The best solution to your super wide hips, even if you’re thin, is something you’ve probably never even considered.
And that’s to develop your shoulders and back/chest muscles to offset the lopsided appearance that excessive hip girth creates.

Shutterstock/sklyareek
I was inspired to write this article after reading about a woman who, no matter what weight she was at (ranging from 125 to 175), complained of “super wide hips” that she hated.
She said that no matter what her weight, her hips were always 12 inches more than her waist.
But this doesn’t sound all that bad, being that the classic enviable measurements for a woman are 36-24-36.
So I’m thinking that the problem is that first measurement; it may be so small that it creates the illusion that the hips are wider than they actually are.
If you have widely spaced hip bones, you can’t change this. A woman or man with low body fat can still look disproportionately wide in the hip area.
If this skinny person gains 80 pounds, they will probably still look out of proportion.
Offset Wide Hips by Developing a V-Taper
Have you ever noticed that in just about every man or woman you’ve seen with extra wide hips, that their shoulders appeared to be narrow or underdeveloped?
And that they lacked muscle development in their back and torso?
I sure have. Though I’ll admit, I’ve seen wide-hipped people with broad shoulders, and I have to say, the broad shoulders do help offset the wide appearance of the hips.
A V-taper body consists of broad shoulders (shoulders wider than waist) and a V shape that begins from the shoulders and down to the pelvic area.
Shutterstock/RomarioIen
This V shape will help obscure the excessive width of your hips — not to mention will make normal-width hips and a normal-width waist seem even narrower and smaller.
This is why sometimes the waist/hips of a female bodybuilder appear so tiny.
Though it IS small, her upper body development makes it appear even smaller. Same with men.
But you do not need to become a bodybuilder or beef up with slabs of muscle to reduce the appearance of wide hips.
• Take up strength training and concentrate on shoulder, back and chest work.

Shutterstock/Catalin Petolea
• If you’re already doing this, you need to change something.
• I recommend the following: wide-grip lat pull-down, wide-grip seated row or standing barbell row, wide-grip T-bar row, bench press, overhead barbell press and dumbbell side raise.

• Use a weight that’s heavy enough to reach “failure” or near-failure within eight to 12 repetitions.
• Rest one minute to 90 seconds in between sets.
• Do not fear bulking up. Believe me, this is very difficult to do. And besides, if you do end up developing more muscle to your liking, you could always reduce the amount of weight you use, which will cause some of the muscle mass you gained to diminish.
Exercises that will NOT Make Wide Hips Narrower
Forget about any kind of spot-reducing, isolating exercise in the name of making wide hips look narrower.
If these bones are spaced wide apart, you cannot change this any more than you can change your height.
If you feel that a lot of excess fat is making you look wide there, then the above strength training exercises, when done properly and intensely (8-12 rep max) will shrink the fat cells (as well as cause fat loss throughout your body).
No amount of crunches, seated twists, standing twists or swiveling movements will shrink fat cells ANYWHERE in your body.
Another thing that will make your wide hips appear narrower is that of burning the excess fat out of your midsection.
Again, no quantity of sit-ups or crunching will accomplish this. Excess fat in your stomach and waistline will only be sucked out when you force your body to dip into this stored energy for fuel.
This happens when you strength train intensely, dramatically raising your body’s energy needs, forcing your body to raid the fat stores in your midsection (and elsewhere) for recovery fuel.
Additional exercises for burning fat: deadlifts, barbell squats, leg presses, high intensity interval training.
The bottom line is that broad shoulders and a V-taper of trained muscles will create the illusion that your hips aren’t as wide as they actually are, making you look narrower there.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/skrotov
Wall Climbing if You’re Plus Size: How to Get Past Fear
The biggest fear of overweight climbers is often thinking everyone else is staring at them… (more…)
Normal Sleep Paralysis vs. a Failed Out of Body Experience

Doctors say sleep paralysis is from the brain vs. the paranormal OBE explanation?
Sleep medicine doctors quickly offer a logical explanation for sleep paralysis. (more…)