HIIT Guidelines for Very Overweight People

High intensity interval training (HIIT) isn’t reserved for just thinner people; obese or very overweight women and men are much capable of employing this method of exercise. (more…)
Lifting Weights or Fish Oil to Prevent Muscle Loss in Old Age?
Which should the elderly do to prevent muscle loss: rely on strength training (weightlifting) or fish oil supplements?
Most elderly people have significant muscle loss, and omega 3 fish oil can actually help — according to studies. But sometimes you have to be really careful where you put your faith.
My elderly father has been taking fish oil gel caps faithfully every day for years, but as time marches on, he continues to lose muscle.
I can’t believe how thin his upper arms have gotten. He doesn’t strength train!
Lifting Weights to Keep Muscle
An elderly person’s first line of defense against muscle loss is weightlifting.
In fact, strength training should be started in younger adulthood for the greatest positive impact. But even when it’s begun in middle age, the results will be extraordinary for those who take it seriously.
So what, then, about fish oil supplements?
Fish oil pills are no replacement for weight-bearing exercise, but research indicates that they will make a difference.
- Insulin sensitivity means that muscle cells have well-functioning insulin receptors, in that these receptors welcome insulin, a hormone.
- Insulin brings to the muscle cells fuel in the form of glucose (blood sugar).
- A well-functioning insulin receptor uptakes the glucose from the insulin, and hence, the muscle cell is supplied with energy.
What is insulin resistance?
Insulin resistance, like the name implies, means that the receptors resist this hormone.
This is a serious problem because the cells end up shorted of their energy source.
Aging cells are more likely to become insulin resistant; being elderly is a risk factor for this problem.
Insulin is necessary for growth of muscle tissue. This is why savvy bodybuilders will consume a meal high in “quick acting” carbohydrates immediately after a weight workout, to spike an increase in insulin!
Insulin boosts synthesis of muscle protein. Increased insulin resistance in the elderly is a key player in loss of muscle strength, says research from University of Texas Medical Branch.
The researchers increased levels of insulin in elderly study participants, and this restored their hampered muscle-building mechanism. “… when we gave seniors double the insulin they would normally produce after eating, their muscles were stimulated like those of young people,” says Dr. Elena Volpi in the paper, and senior author of the study (Diabetologia , Sept. 2009).
The insulin was given intravenously to 14 elderly subjects. Dr. Volpi clarifies that the insulin “resistance” that comes from old age is not the same as the insulin resistance of type 2 diabetes.
Another study shows that omega 3 fish oil enhances muscle protein metabolism.
Omega 3 fatty acids help improve glucose metabolism in people with insulin resistance.

The researchers gave omega 3 fish oil to steers, and the results were that these animals had improved muscle protein metabolism.
The research was headed by Carole Thivierge, Université Laval’s Institute of Nutraceutics and Functional Foods, and she concludes that supplementation with omega 3 fish oil pills can help prevent muscle loss in elderly people.
And yet another study on fish oil suggests the same conclusion. This study, headed by Vera Mazurak, PhD, of the University of Alberta in Edmonton, Canada, examined the role of omega 3 fish oil on muscle loss caused by cancer.
The results were very favorable, and she deduces that elderly people who are at risk for losing muscle should be able to benefit from two grams a day of omega 3s from fish oil.
What does a personal trainer think?
As a former personal trainer at a gym, I stand by my opinion that weight-bearing exercise is the best fountain of youth for the elderly and will go a long way in aiding prevention of muscle loss, and will even restore some lost muscle.
But I just can’t believe that we can preserve muscle mass by ONLY taking a supplement, and doing NO strength training. It can’t be this easy. Because it isn’t.
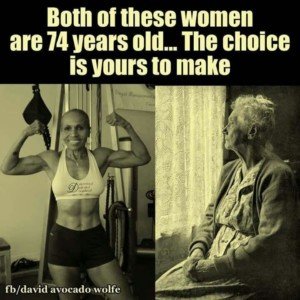
You must bear weight, like the woman pictured on the left above at age 74.
But whether an elderly person lifts weights or not, the research on fish oil omega 3 supplements can’t be ignored.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Sources:
sciencedaily.com/releases/2011/02/110228090202.htm
sciencedaily.com/releases/2009/09/090925115457.htm
sciencedaily.com/releases/2007/05/070509161106.htm
How to Keep Your German Shepherd Very Busy

German Shepherds that are not stimulated will find their own entertainment, such as shredding shoes or consuming cupboards. (more…)
Struggling to Get in 10,000 Steps a Day? Simple Solution!
If you’re struggling to accumulate 10,000 steps a day, no matter how many times you get up during TV commercials, leave your computer station or pace around every time you’re on the phone, I have the solution: (more…)
Which Body Part in Injured Teen Athletes Gets Surgery the Most?

If your teen is involved in sports, don’t be surprised if sooner or later, he or she gets injured and needs surgery.
There is one specific part of the body that when injured, requires more surgery than any other body part in high school athletes.
It is the knee.
(more…)
Can Being Religious Lead to Obesity?

How can religion lead to obesity?
Or is it that very overweight people are drawn to organized religion? What’s truly going on here?
The link between middle age obesity and religion has already been established.
What researchers wanted to know is the cause-and-effect relationship between religious involvement and obesity. So researchers from Northwestern Medicine decided to find out.
“We don’t know why frequent religious participation is associated with development of obesity, but the upshot is these findings highlight a group that could benefit from targeted efforts at obesity prevention,” says Matthew Feinstein, the study’s lead author, in the report.
The research tracked weight gain over a period of time, establishing that obesity comes after the religious involvement, not the other way around.
In the study, 2,433 women and men were tracked for 18 years. The findings in adults 20 to 32 years old was very intriguing:
If they had a high level of religious participation (at least once/week), they were 50 percent more likely to develop obesity by the time they hit middle age.
Variables of age, race, education, gender, income plus baseline body mass index (BMI) were adjusted for.
Does this mean that attending religious functions is bad for your health?
The study authors insist no. In fact, past studies show that “religious” people do tend to live longer than those who aren’t into religion – partly because faithful people tend to avoid smoking or smoke less.
“I am not familiar with this study, but personally I can see a correlation,” says Susan L. Besser, MD, with Mercy Medical Center, Baltimore; Diplomate, American Board of Obesity Medicine and board certified by the American Board of Family Medicine.
“I am a religious Jew — I attend regular synagogue services and participate in all religious events.
“These events generally include festive meals (read: more food, larger portions). So I can understand why weight gain might happen.”
Another possible explanation is that some religious or deeply faithful people are more apt to put their health in God’s hands.
Therefore, concern over diet, portions, exercise and weight wouldn’t be a high priority – hence leading to obesity.
 Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
Dr. Besser provides comprehensive family care, treating common and acute primary conditions like diabetes and hypertension. Her ongoing approach allows her the opportunity to provide accurate and critical diagnoses of more complex conditions and disorders.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Alexisrael, CreativeCommons
Source: sciencedaily.com/releases/2011/03/110324104145.htm
Heart Disease, Depression Linked in Women Under 40
Young women shouldn’t have to worry about heart disease, right?
Well, they should definitely be aware of it, especially since it’s linked to depression in this very age group. (more…)
Causes and Prevention of Hamstring Injuries from Fast Running

When a fitness enthusiast or athlete suffers a hamstring injury, this really blows, but if you know the causes and the solutions, this will put you way ahead of the game.
Hamstring injuries can interfere with training for fitness, sports or physique competition: a hamstring injury disrupts running, and running is a heavily favored fat-burning activity for those wanting to slash body fat. (more…)
Groin Injuries: Which Sports Cause These, Risks, Treatment

Watch even just a little sports on TV, and sooner or later you’ll hear something about an athlete’s groin injury.
Sports that commonly result in groin injuries: running (or sports that require a lot of running or stop-and-go actions, like soccer, lacrosse, football, tennis and hockey.
Groin injuries can also strike inline skaters, surfers and people working their legs at the gym.
“Groin injuries are extremely common and often difficult to manage at
times,” says Peter Vitanzo, Jr., MD, sports medicine specialist at the Rothman Institute at Thomas Jefferson University Hospital, in Philadelphia.
“They can be very disabling for an individual, particularly an athlete.”
Seems as though when a professional athlete gets stricken with a groin injury, it persists and keeps the athlete out of commission for months on end.
Dr. Vitanzo explains, “These types of injuries can be a diagnostic dilemma at times, which can lead to a delay in being evaluated by a specialist and, ultimately, treating appropriately.
“This is one of the reasons these injuries can become chronic and stubborn to manage.”
What is a groin injury?
Vincent Perez, PT, with Perez Physical Therapy in NY, explains that “Groin injuries is a term typically used to describe strains/tears of several muscles: adductors and hip flexors. Those muscles are usually any of the adductors or the iliopsoas, which is the hip flexor.”
Dr. Vitanzo adds that patients may experience pain in the front of the groin area (hip flexor strain or even an iliopsoas bursitis).
Another area of pain is “deep on the inside of the groin (classic adductor strain), or even in the midline in the front of the pelvis (osteitis pubis or ‘sports hernia’).”
But no matter where the problem is, these injuries can be a real impediment to the athlete or trainee.
The muscle-tearing can result in scar tissue, and this is often the cause of recurrence.
Runners with Groin Injuries
In a way, this is a whole special group when it comes to these injuries.
According to Dr. Vitanzo, “In my experience, patients who are runners tend to present much later in their course with chronic symptoms, as opposed to other athletes whom I have dealt with who tend to present right away.

“I think a lot of this has to do with the mentality and passion of the ‘true runner’ and their unwillingness to have to stop running in order to appropriately diagnose, treat and allow these types of injuries to heal.
“This can become a problem because the longer these injuries linger, the longer and much more difficult they are to treat and manage.”
If diagnosis—and therefore treatment—are delayed, then treatment will require more time than ever away from the offending activity. This can be very difficult for the committed runner.
“Many times patients wait until the symptoms get so bad that they just can’t perform their activity anymore to the level they want to compete at.”
Treating the Groin Injury
Dr. Vitanzo says that when diagnosed promptly, these injuries can be managed without incident and the athlete can return fairly quickly to sports activities.
But if there is a delay in diagnosis—for instance, the sufferer thinks he or she can work it out without intervention—then the injury can become plain stubborn.
Perez explains, “They take a while because of the stress the area receives during aggressive sports, and the athlete’s training/rehab usually does not involve enough rotational movements with sufficient speed and intensity. Scarring obviously adds to the time.”
Cross-training should be part of treatment protocol, to prevent deconditioning.
If the injury is acute, then the usual fare of ice and anti-inflammatories is called for.
In a chronic groin problem, inflammation isn’t a key player; rather, scar tissue is—and scar tissue is much harder to treat. But there’s hope.
Dr. Vitanzo explains, “One of the newer diagnostic/treatment options includes use of musculoskeletal ultrasound which I incorporate frequently in managing these patients.
“The beauty of this type of study compared with MRI is that it gives dynamic views of an injury as opposed to static views like an MRI.
“Therefore, you can actually stress the area of concern while performing the study and really localize the injury, even subtle injuries which a ‘static’ study may miss.
“I have also utilized ultrasound guidance to inject these recalcitrant injuries with very good results and quicker return to activity times.”
Risk Factors for Groin Injuries
Perez says that insufficient warm-up and poor flexibility are at fault, along with possibly weakness.
In fact, lack of flexibility can cause a groin pull or strain during a leg press motion.
If the trainee lowers the declined leg-press platform deeply, in combination with feet pointed outward (especially if feet are also far apart), then this will stress the adductor region.

Shutterstock/Motortion Films
This is a good exercise, but for people new at it, very light weights are mandatory.
Otherwise, the trainee may exit the equipment almost immediately feeling something wrong with the groin area.
Any adductor routines that combine resistance with stretching can put a person at risk for groin injuries — unless the trainee is flexible and already conditioned.
To get conditioning, the routine must be initially done gently and with light weights, if any at all.
Furthermore, aggressive stretching — perhaps by eager and impatient martial artists in an attempt to increase “splits” (both kinds) flexibility — can also injure the groin area.
Another risk is when a person engages in a sport that involves a lot of rotation in the pelvic region.
Again, stiff muscles and/or inadequate warm-up will increase risk of groin strains or tears.
Groin injuries do not need to be permanent. Full groin/adductor capabilities can be restored if:
Trainee stops making excuses and heads straight for an orthopedic specialist or physical rehab expert.
Trainee accepts the reality that he or she may need to completely avoid the offending activity for a while.
Trainee devotes time to a structured stretching and cross-training regimen that’s designed to bring back strength, increase limberness and break down scar tissue.
There is no cookie-cutter prescription for groin injury rehabilitation routines.
Groin injuries occur to different sections of soft tissue, and thus, necessitate different treatment modalities for each individual case.
In order to determine specific exercise motions, the sufferer would need a complete evaluation by an orthopedic specialist, who would then most likely make a referral to a physical therapist.
The physical therapist would then perform an evaluation of the groin injury, based upon which a set of specific routines could be designed.
 Dr. Vitanzo passed away in 2020.
Dr. Vitanzo passed away in 2020.
 Vincent Perez has dedicated 25+ years as a licensed physical therapist to managing orthopedic and sports injuries. Perez has treated professional and amateur athletes in all sports including the New York Yankees.
Vincent Perez has dedicated 25+ years as a licensed physical therapist to managing orthopedic and sports injuries. Perez has treated professional and amateur athletes in all sports including the New York Yankees.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock Syda Productions
Do the Inner & Outer Thigh Machines Really Burn Leg Fat?