Congestive Heart Failure vs. ALS: Symptom Comparison
If you’ve been suffering from worsening fatigue, congestive heart failure may come to mind, but ALS can also cause this.
Is there a difference between early stages of ALS fatigue and that of mild congestive (now known as “chronic”) heart failure?
Chronic heart failure is when the ability of the heart to pump an adequate supply of blood with each beat is compromised.
There may or may not be an issue of congestion causing fluid retention.
Systolic heart failure is when an insufficient volume of blood gets pumped with each beat due to weak cardiac muscle, though the chambers of the heart fill with an adequate supply of blood to be pumped.
Diastolic heart failure is when the pumping action is adequate, but not enough blood fills the chambers to be pumped out with each beat.
ALS is a motor neuron disease in which the nerves fail to properly conduct electrical impulses to contract muscle fibers.
This problem originates in the spinal cord, brain stem and brain where neurons start dying.
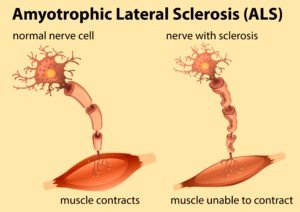
As a result, muscle tissue—because it never receives instructions to contract from the dead nerve cells—begins wasting away.
Chronic congestive heart failure and ALS cause fatigue.
But is the fatigue from one different from the other? At least in the early stages of ALS vs. mild heart failure?
As ALS progresses, other symptoms come into play that don’t fit the bill for a cardiac problem.
And as chronic heart failure progresses, this too brings forth symptoms that are not present with ALS at any stage.
Symptoms of Class II and III Chronic Heart Failure
- Comfortable at rest, but normal physical activity may cause fatigue and shortness of breath (II) or with III, you’re still okay at rest, but there’s an obvious limitation with even mild exercise: fatigue and shortness of breath.
- Fatigue is actually one of the first-noticed symptoms.
- Along with that fatigue in early CHF may also be edema (swelling) in the ankles, and weight gain from fluid retention.
As congestive heart failure progresses, you’ll probably also experience a cough from fluid buildup in the lungs, wheezing and a shortness of breath that’s not only from impaired pumping action of the heart, but fluid buildup (edema) in the lungs.
This will cause an increasing intolerance to exercise or physical activity.
As CHF progresses, the patient will experience shortness of breath at rest—and in fact, may need supplemental oxygen for sleep.
The CHF patient does not have a mechanical problem with breathing; their ability to inhale works just fine.
The issue is inadequate blood circulation and edema in the lungs. In fact, they may have no problem whatsoever taking deep breaths.
“Shortness of breath” is not the same as difficulty inhaling.
“Shortness of breath” is what one feels when there’s not enough oxygen circulating in their body—as in a healthy person who just sprinted across a parking lot, or a person with CHF who just walked up a short flight of stairs.
“Muscular weakness is a prominent feature with ALS, and exercise intolerance is a hallmark of heart failure,” says Roger Mills, MD, cardiologist and former professor of medicine, University of Florida, and author of “240 Beats per Minute. Life with an Unruly Heart.”
“However, the weakness of ALS is more or less constant and slowly progressive.
“Early on, heart failure patients are not so much weak as [they are] exercise intolerant.
“The ALS patient can’t go up stairs because he/she does not have the leg strength to lift his/her body.
“The heart failure patient can’t make it all the way up because he/she becomes short of breath after five or six steps.”
The collection of CHF symptoms are hard to dismiss as the disease progresses. These include loss of appetite, fluid retention and nausea.
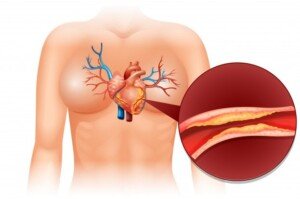
A unique characteristic of CHF is that, due to the impaired pumping action of the heart, blood is diverted away from the arms and legs (less critical areas), to supply the brain and heart.
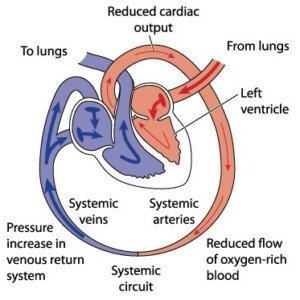
Heart Failure. Shutterstock/Blamb
Patients thus often feel weakness or fatigue in their legs and arms. This will affect the activities of daily living.
Meanwhile, again, they have no trouble breathing, but often FEEL short of breath.
As for the actual ability to walk up a flight of stairs, let alone hop up the steps, “It depends on how far ALS has progressed,” says Mitzi J. Williams, MD, clinical neurologist with Morehouse School of Medicine and clinical advisor for the Multiple Sclerosis Foundation.
“In early stages, someone may be able to hop up the stairs,” says Dr. Williams.
“If weakness and fasciculations progress, this will no longer become possible. The symptoms only continue to progress — so the symptom will not improve once they can no longer hop up the stairs.”
As chronic heart failure worsens, the patient will still be able to climb a staircase with normal ambulation – with no impairment in the operation of their neuromuscular system.
However, there may be pauses every few steps as they catch their breath.
Symptoms of Early ALS
- Difficulty walking, which may include stumbling
- Weakness in the legs
- At this point, the arms may feel fine (whereas in CHF, all four limbs are simultaneously affected due to blood-supply diversion)
- Cramping muscles
- Twitching muscles
- Slurred speech
- Trouble swallowing
If someone with ALS has at least one other symptom besides fatigue or weakness, this will point away from congestive or chronic heart failure.
For instance, CHF doesn’t cause slurred speech or tripping due to lack of coordination.
ALS typically starts in one part of the body, then spreads, whereas the weakness and fatigue of congestive (or chronic) heart failure is global since it’s caused by inadequate blood supply.
As ALS progresses, respiratory function becomes impaired. Breathing is controlled by muscles.
Because motor impulses are not reaching these muscles, the patient begins experiencing difficulty with the mechanics of breathing. But by then, they will have already been diagnosed.
As both congestive heart failure and ALS progress, the disparity in their symptom profiles increases, though they often just begin with weakness and/or fatigue.
The element of weakness, rather than fatigue, is more pronounced in early ALS; and the element of fatigue, rather than weakness, is more prominent in mild congestive heart failure.

Dr. Williams is author of “MS Made Simple: The Essential Guide to Understanding Your Multiple Sclerosis Diagnosis.” She is a member of the American Academy of Neurology.

Dr. Mills is the former medical director of the heart failure and heart transplant service at the University of Florida, was a staff cardiologist at The Cleveland Clinic and has authored over 100 peer-reviewed publications. “240 Beats a Minute” is available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Causes of Fast Resting Pulse in Athlete Besides Overtraining

The reason some athletes have a fast resting heart rate has nothing to do with their training.
Athletes can have medical conditions that cause a fast resting pulse. (more…)
What’s the Best Cardio Equipment for Diabetics?

If you have diabetes and want to use the best cardio machine for your condition, you’ll be surprised at just what this piece of equipment is. (more…)
How a Diabetic Can Get Six-Pack Abs
Here are the basic guidelines for how someone with diabetes can get six-pack abs.
The good news is that for diabetics who want six-pack abs, there is nothing different they need to do as far as the training exercises. (more…)
Sudden Sharp Chest Pains on Left Side: Causes

There’s actually quite a few causes of sudden sharp pain on the left side of one’s chest, ranging from heart problems to serious lung conditions to harmless muscle strains.
Causes of Sharp Chest Pain on the Left Side
“The ‘type’ of pain or the location of the pain in the chest area doesn’t necessarily rule out heart related issues,” says Dr. Kavitha Chinnaiyan, MD, a cardiologist at William Beaumont Hospital in Royal Oak, MI.
“Although the heart is placed slightly to the left of the midline in the chest, heart-related discomfort can be located anywhere above the diaphragm.”
Acute pericarditis is one such cause of sharp pain on the left side of the chest.
This presents most commonly with a sharp stabbing pain in the chest, behind the breastbone or in the left side of one’s chest.
However, in some patients, sometimes the discomfort is dull or aching rather than sharp and stabbing.
What is pericarditis?
The pericardium is a sac-like membrane; it surrounds the heart. When this membrane becomes irritated or swollen, it’s pericarditis.
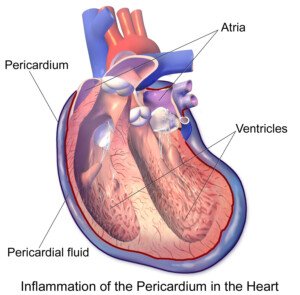
Source: BruceBlaus/CreativeCommons
Sharp chest pain is not typically due to coronary artery blockages, but “not typically” doesn’t mean it can’t ever be, either.
Pain Worse with Movement
If this is the case, it rarely means coronary artery disease. It’s very likely a musculoskeletal issue — such as a strained muscle from activity.
Does your left side sharp chest pain fluctuate with movement?
Dr. Laman says that this “most commonly indicates that the ribs, muscles, cartilage [costochondritis] or lungs [e.g., pneumonia, pleuritis] are involved.”
Blood Clot in a Lung
A blood clot in a lung has the potential to cause a sharp pain.
You’re at risk for this condition if any of the following applies: recent long airline flight with very little leg movement; recent long car trip with legs in cramped quarters and no rest stops to stretch the legs; recent joint replacement or abdominal surgery; excessive bed rest; birth control pills; pregnancy; obesity.
A smoking habit adds to the risks.
Signs that Left Side Sharp Chest Pain Is Not a Heart Blockage
• Pain increases with inhalation
• Duration is a few seconds
• Gets worse when you press on your chest
• Movement aggravates it
How likely is left sided sharp chest pain to be a heart attack?
Harvard Health Publications says that “pain clearly on one side of the body than the other” is “less likely to be a heart attack.”
However, a heart attack CAN cause pain on the left side—but it’s usually not sharp, piercing or stabbing.
Additional Causes of Sharp Pain on the Left Side of the Chest Only
• Intercostal neuralgia (damage to nerves that run between the ribs)
• Heartburn/acid reflux
• Recent pressure against the breast
About that last point, that has happened to me. A person may confuse a pain that originates in the breast with one that’s more “chesty,” so I thought I’d mention it.
I had been leaning forward and massaging my left elbow (golfer’s elbow) with my right hand.
My right arm kept pressing against the right side of my right breast.
A few hours later I started getting shooting, stabbing pains there.
Over time I noticed that when this occurred, I had massaged my elbow a few hours prior.
I then began massaging my elbow in a different sitting position, making sure my right arm was not contacting my breast.
The sharp right “chest” pain never returned.
So if this kind of pressure is occurring to your left breast (which can also happen if you sleep on it wrong), then it just could trigger a sharp pain that seems to be coming from your chest.
My doctor told me that this phenomenon is the result of breast tissue being very sensitive, and it’s nothing to worry about.

Dr. Chinnaiyan has authored and co-authored 100+ manuscripts and abstracts. She has served as the Chair of the Board of Directors of the American Heart Association of Southeast Michigan.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Twinsterphoto
Source
health.harvard.edu/heart-health/chest-pain-a-heart-attack-or-something-else
pijn.com/en/patients/cause-of-pain/diagnoses-per-body-region/upper-back-chest/intercostal-neuralgia/
If You Had a Heart Problem Would Chest Hurt if Pressed?

So if you have a heart problem like severely clogged arteries or a rhythm disorder, would pressing your fingers or palm on your chest bring out any pain?
What if you were having a heart attack?
“Pain reproduced by pressing on the chest or with body motion” is “less likely to be a heart attack,” according to Harvard Health Publications.
The key term here is “less likely.” This does not mean “100 percent definitely not.”
CAN a heart attack make pressing on the chest hurt?
“It can, even though there is a misunderstanding that pain on pressing the chest wall means it is not coming from the heart,” says Dr. Kavitha Chinnaiyan, MD, a cardiologist at William Beaumont Hospital in Royal Oak, MI.
Dr. Chinnaiyan is founder of Heal Your Heart, Free Your Soul, an online, yoga-based prevention program.
Dr. Chinnaiyan explains, “On rare occasions, there can be tenderness over the chest wall when one is having a heart attack or pain as a result of blocked arteries.
“In general, however, pain when pressing on the chest wall happens in heart-unrelated conditions like inflammation of the rib joints (known as costochondritis).”
Kaiser Permanente Health Matters states that “If chest pain increases if you press your finger on the painful site, it is probably from a strained muscle, ligament or maybe even a fractured rib.”
Costochondritis is an inflammation of the cartilage in the chest wall (this is no secret among weightlifters), and this kind of pain should last only several days.
Movement and pressing on the hurting area will aggravate it.
Have you ever noticed that in any of the symptom lists you’ve read for heart attack (or pending attack), the symptom of “hurts when the area is pressed on” never shows up?
Heart Attack Symptoms
• Pain is not responsive to rest
• Sweating
• Nausea
• Shortness of breath
• Weakness
More Symptoms to Consider
• Tightness, burning, fullness, squeezing or pressure in the chest
• Pain in center of chest
• Numbness, prickling, pinching or pain in the jaw, neck, back or one or both arms
• Vomiting
• Dizziness or lightheadedness
• Unexplained fatigue
• Cold sweat
What about arrhythmia symptoms?
• Fluttering in chest
• Racing pulse
• Slow pulse
• Chest pain
• Shortness of breath
• Dizziness, lightheadedness
• Sweating
• Fainting, feeling faint
These arrhythmia symptoms are also typical on symptom lists, and “hurts to press chest” is never included.
Kirk Laman, MD, a cardiologist with healthcentral.com, states on the site: “…women with heart blockages sometimes present with sharp pain. As a general rule, the pain is not worse with pressing on the chest.”
The key phrase is “As a general rule.”
So what does all of this mean?
• Never assume unexplained chest pain can’t be a heart attack or severe artery blockage just because it doesn’t hurt to press on your chest.
• Discomfort from pressing on your chest does not rule out a heart problem.
• In the vast majority of cases when pressing on the chest hurts, there is not a heart problem.

Dr. Chinnaiyan has authored and co-authored 100+ manuscripts and abstracts. She has served as the Chair of the Board of Directors of the American Heart Association of Southeast Michigan.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sources:
health.harvard.edu/heart-health/chest-pain-a-heart-attack-or-something-else
wellness.uci.edu/chestpain.pdf
mayoclinic.org/diseases-conditions/heart-arrhythmia/symptoms-causes/dxc-20188128
healthcentral.com/heart-disease/c/410684/84172/sharp-chest/
Stabbing Chest Pain when Lying on Left Side: Heart or Muscle?
Chest Pain with Hoarse Voice: May Be Cancer or Aortic Aneurysm
Heart Palpitations While Walking: Causes & Solutions

Is there something inherently unique about walking that causes PVCs or heart palpitations?
Yes, there is something that just might be going on only when you walk.
And one of those is anxiety.
“Stress and anxiety are the most common cause of heart palpitations,’ says J. Mark Anderson, MD, DABFM, of Executive Medicine of Texas and who is board certified in family medicine.
Let’s take a look at anxiety as a reason why your palpitations seem to occur only during times of walking.
The term “palpitations” is sometimes used to reference a suddenly racing pulse.
But it more commonly refers to what seems to be a delayed, skipped or extra heartbeat.
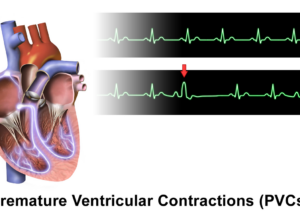
And this sensation is also often referred to as PVCs: premature ventricular contractions.
It’s the PVC that makes you think that your heart skipped a beat or had a sudden irregular beat, flutter or thumping.
First, take note of when your walking seems to bring on the PVCs.
“Some people tend to go for long walks or power walks as a way to deal with the stress of the day or to start their morning,” says Dr. Anderson.
“When the walks are coupled with stressful thoughts, like what awaits you at the office, palpitations are more likely to occur.”
Maybe they occur only when you’re walking from the parking lot of your workplace to your office? Hmmm, very interesting!
This sounds like job anxiety — a “program” running in the back of your mind as you subconsciously anticipate stress from your boss, coworkers, clients or workload.

Shutterstock/Creativa Images
Is it only when you walk on a treadmill? Perhaps this is the time that your mind wanders, venturing into stressful territory, or maybe there’s an influx of intrusive negative thoughts.
Maybe while you’re walking for fitness, you just can’t help play out in your mind some unnerving scenarios, such as confronting a hostile family member about the money they owe you.
Maybe it’s a time that you usually re-enact scenarios that have already happened—that you wished you had handled differently and you’re mad at yourself for not.
Stress and anxiety can definitely trigger palpitations — and maybe those treadmill walks, or walking in the nearby park or walking your dog, are a conditioned stimulus for feeling stressed.
Have you noticed that, despite walking “causing” your PVCs, you don’t get PVCs or palpitations while you’re strength training at the gym or engaged in other activity that’s more intense and distracting than mere walking?
This is a tip-off that the PVCs are being generated by anxiety — that’s triggered by walking.
However, here’s a fair question:
Is there something inherent in the actual biomechanics of walking that causes palpitations?
“These can be worsened by the use of caffeine,” begins Dr. Anderson.
“This is because your heart rate tends to speed up in these circumstances.
“The same is true when walking, especially power walking. If no other symptoms are present, it will normalize when you sit down or relax.
“Palpitations that are accompanied with dizziness, fatigue or other symptoms should be evaluated by a healthcare provider.”
More times than not, though, it’s just that walking sometimes encourages thoughts to wander and imaginations to get a little wild, and the walking may also be towards a source of stress, such as your workplace from the parking lot, or the mall where you face large shopping tasks.
The Key Questions
• Whenever you have palpitations, are you always walking?
• They never occur during heavier physical exertion?
• Never during gardening (which can be very relaxing)?
• Never during yoga, swimming or strength training?
• And…it’s only sometimes during walking, not always?
Answering “yes” to these questions points towards anxiety as a cause.
You may also want to ask yourself what you eat or drink shortly before going on fitness walks. As Dr. Anderson pointed out, caffeine can trigger palpitations.

Shutterstock/NOBUHIRO ASADA
Another Big Question
Have you been diagnosed with heart disease? If so, the presence of PVCs or palpitations becomes more significant.
It’s advisable that you get a full exam by a cardiologist to see if you might be at risk for coronary heart disease.
Source: Freepik.com/brgfx
The doctor may order a cardiac stress test and echocardiogram. PVCs with coronary heart disease are not a good combination.
That said, you should also ask yourself if walking has become a conditioned stimulus for palpitations because every time you walk for an extended period, you start worrying about PVCs!
Maybe you had a few PVCs while walking, and that single incident has now thrown you for a loop? Anxiety triggers hormones that can make the heart jump or flutter.
PVCs can have a medical cause and also be caused by liquor, medications and magnesium/potassium deficiency.
But again, if you have them ONLY when walking, this points away from a pathological or pharmaceutical cause.

Dr. Anderson is coauthor of the award-winning book, “Stay Young: 10 Proven Steps to Ultimate Health,” and host of the nationally syndicated Staying Young Show which goes to podcast as Staying Young Show 2.0.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sources:
webmd.com/heart-disease/atrial-fibrillation/features/pounding-heart-anxiety-afib#1
heartmdinstitute.com/heart-health/what-is-a-heart-palpitation/
Best Exercises that Help Prevent PVC’s

Can exercise, rather than drugs, be beneficial for premature ventricular contractions?
Or is it the other way around—that some kinds of exercise can increase PVC’s?
Sedentary Men with PVCs Benefit from Exercise
• 196 sedentary middle-aged men who had PVCs were put on an exercise program for 18 months.
• For the men who adhered well to the regimen, the work threshold for the trigger of PVCs increased (meaning, a higher level of exercise was necessary to bring out the PVCs when compared to before the exercise program was implemented).
• Frequency of PVCs was reduced. (American Journal of Cardiology, 4/73, vol 31, issue 4)
So for starters, if you’re a middle-aged sedentary man who gets premature ventricular contractions, exercise will likely reduce these.
If light to medium exertion brings on PVCs (i.e., carrying a crate of books up the stairs), then as you become more conditioned from structured exercise, the amount of exertion needed to bring on PVCs will get higher.
Is there a “best” exercise for someone who has PVCs?
NOT getting enough exercise can trigger a premature ventricular contraction.
If you’ve been having PVCs, you’ll want to discuss marathon-based activity with a cardiologist to see if that’s safe.
Your doctor will want to give you a cardiac workup. You may be told to scale back.
However, it’s safe to make an effort to get in at least 8,000 steps, even 10,000, every day.
In addition, half an hour of medium exertion or 15 minutes of high intensity are safe as well (again, see a cardiologist just to be sure).

Freepik.com, jcomp
It seems intuitive that rhythmic aerobic exercise (hiking, incline walking, a step class, pedaling, running, sports like tennis) would be among the best exercises for premature ventricular contractions — without going overboard to the degree of a marathon.
For overall heart health, this kind of exercise is strongly recommended by many cardiologists, the American Heart Association and the American Council on Exercise.
Exercise for EVERYONE with PVC’s
“In general, people should get a healthy amount of exercise,” says Daniel P. Morin, MD, FACC, formerly Director of both Electrophysiology Research and Cardiovascular Research for Ochsner Health System, and currently Professor of Medicine and Cardiology at University of California, San Francisco.
“Some types of PVC’s may be increased during exercise, as some PVC’s only occur during a certain range of background heart rate,” explains Dr. Morin.
“For the same reason, other PVC’s may disappear during exercise. Exercise by itself is rarely the direct cause of PVCs.”

If you’re normally sedentary, but exercise brings on PVCs, see a cardiologist for an assessment and individualized recommendations.
On the other hand, if you have PVCs at rest, and notice that they don’t occur when you exercise, that’s good news.
A third possibility is that you have premature ventricular contractions at rest, but they increase with exercise. Again, it’s best to see a cardiologist.
The type of cardiologist you should see is an electrophysiologist.
This type specializes in the electrical activity of the heart, rather than the plumbing (arteries). This is a very important distinction.
Additional Triggers
• PVCs that seem to be triggered by exercise alone may actually be getting a boost from pre-exercise caffeine intake.

Shutterstock/NOBUHIRO ASADA
• Another potential trigger is anxiety over the idea that exercising may cause PVCs!
• Keep track — though not with a worried mindset — of your pulse when you’re performing moderate-level duties of day-to-day living such as hauling around heavy garbage, carrying toddlers up a flight of stairs, playing with the kids in the backyard, chasing around the dog, etc.
Usually when performing these tasks you’re not thinking of your heart rate.
Make a point of remembering to ask yourself, AFTER you’ve performed these tasks, “Did I have PVCs during any of that?”
There is no single specific exercise (e.g., walking lunges, certain yoga poses, leg pressing, dumbbell squats, Zumba) that’s been proven to be best for PVCs.
But the heart and overall body just love consistent aerobic and strength training.
 Dr. Morin’s clinical interests are in device therapy for cardiac dysfunction (including cardiac resynchronization therapy) and treatment of cardiac arrhythmias with medical therapy and/or catheter ablation.
Dr. Morin’s clinical interests are in device therapy for cardiac dysfunction (including cardiac resynchronization therapy) and treatment of cardiac arrhythmias with medical therapy and/or catheter ablation.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Doidam 10
Sources
heart.org/HEARTORG/HealthyLiving/PhysicalActivity/FitnessBasics/American-Heart-Association-Recommendations-for-Physical-Activity-in-Adults_UCM_307976_Article.jsp#.WHValVMrLxM
acefitness.org/about-ace/press-room/300/american-council-on-exercise-recommends-60-minutes
Drjohnday.com
Awakening from Sleep with a Racing Heart: Causes, Solutions

If a racing heart is waking you from sleep, this can be even scarier than PVCs.
When you’re sleeping, your body is at its lowest energy needs, so why would your heart suddenly start racing? (more…)