Early ALS Muscle Atrophy vs. Benign Atrophy Appearance

“It can be difficult to distinguish between early ALS atrophy and normal atrophy,” says Bonnie Gerecke, MD, MD, director of the Neurology Center at Mercy in Baltimore.
The typical course goes as follows:
• You notice a muscle has been twitching, such as in the calve, hamstring, chest or eyelid.
• After getting annoyed enough, you google “cause” of twitching muscles.
• ALS sites appear in the search results and grab your attention.
• You begin reading one ALS site after another, and all say that “muscle twitching” is a symptom, but they also say that “muscle atrophy” is a symptom.
• You then begin checking your muscles for signs of atrophy.
• You begin discovering signs of atrophy, such as one calve is bigger than the other, or there’s a “dent” in the front of your thigh.
Benign thigh dents take on a variety of forms.
Atrophy means shrinkage of muscle due to disuse. This happens in healthy people all the time, and can be quite noticeable depending on the circumstances.
We’ve all seen the atrophy of a limb after a cast for a broken bone, that’s been in place for weeks, is finally removed.
Telling the Difference Between ALS Atrophy and Benign
“Early ALS atrophy may be more focal,” says Dr. Gerecke.
“This means that it may start in a specific muscle group, such as the small muscles of the hand,” continues Dr. Gerecke.
“It then spreads to affect other muscles of the same limb, for example.”
So for instance, ALS may begin in the foot, then locally spread, being confined to the lower leg.
Eventually the other side of the body will become affected, most likely beginning with the opposite foot and lower leg.
ALS atrophy does not strike the entire body at the same time. It begins very locally.
Shutterstock/joshya
Dr. Gerecke explains, “Normal atrophy such as that associated with aging tends to be more symmetrical and diffuse.”
But what if you notice local atrophy?

Well, here’s the thing about this. You must ask yourself what proof you have that what you’re seeing is actually shrinkage of muscle.
If you frantically inspect your body in the mirror, you just might find what you’re looking for: signs of atrophy – or rather, what you THINK are signs, such as:
• One calve is smaller than the other.
• There’s a depression of skin below the right collarbone but not the left.
• One foot is slightly larger than the other.
• One forearm is smoother than the other.
• The veins in the top of one foot are more visible than in the other.
• One thigh has a dent.

Shutterstock/Motortion Films
You even confirm some of the size differences with a measuring tape. You’re convinced you have localized atrophy.
Dr. Gerecke says, “Normal atrophy is also not as pronounced as pathological atrophy associated with ALS.”
You may be thinking that ALS, like any degenerative disease, starts out very small; that it has a very early stage – and that during this stage, the atrophy would actually not be pronounced.
But if it’s ALS, it won’t be long before the wasting becomes increasingly obvious – and accompanied by weakness.
In fact, the weakness will very likely come before visible signs of muscle shrinkage.
So you have to keep reminding yourself of a few things:
• If you’re healthy, time passage will become very reassuring, since in a healthy body, there is no progression of visible or functional pathology.
• Parts of your non-dominant limbs are bound to be noticeably smaller than the dominant ones, but smaller doesn’t necessarily mean atrophied due to less use.
• You may find that your non-dominant left lower leg is smaller than your right, but that it’s also the leg you jump off of when doing single-leg jumps across a water puddle, and that your right leg was never the better one at leaping.
• The body is naturally asymmetrical. There are dips, dents and depressions on one side that are not on the other.
You’re not a Greek statue. You’re imperfect. There’s going to be asymmetry!
So though the visible distinction between early ALS and benign atrophy may be difficult to tell, just hold tight and realize that you are, from a statistical standpoint, panicking for no reason whatsoever.
Let time passage work its wonders on you.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
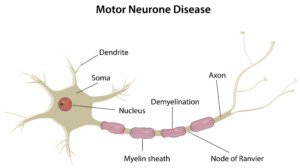
Top image: Shutterstock/BLACKDAY
Why Quitting Smoking after a TIA Is So Important

Do whatever it takes to quit smoking if you’ve had a TIA. Smoking damages the blood vessels in the brain.
But not only that, it also causes conditions that are independent risk factors for transient ischemic attack. (more…)
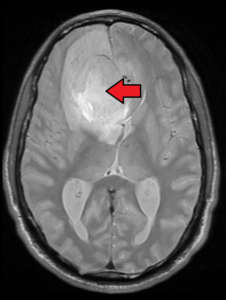
Should Family Members of Brain Aneurysm Patient Have MRI?

If you just learned a family member has a brain aneurysm, you definitely should schedule an MRI scan of your brain, as there is a familial link to this condition.
This genetic link was shown in a large study (Neurology. 2013 Jun 4;80(23):2154-65).
The paper states: “Our comprehensive meta-analysis confirms a substantial genetic contribution to sporadic intracranial aneurysm.”
You Learn an Immediate Family Member Has a Brain Aneurysm
• You should undergo an MRI, whether that first-degree is your parent, your sibling or your child.
• First discuss the MRI screening with your primary care physician.
“We’ve had situations where an adult in her 40s was found to have a cerebral aneurysm,” says Curtis Pavlick, a cerebrovascular physician assistant, in a report at clevelandclinic.org.
“On the suggestion that others be checked, her sister was found to have one and their mother was found to have one.”
Pavlick points out that the risk increases if you and/or other family members have risk factors for a brain aneurysm, like high blood pressure and smoking. Other risk factors are unmanaged diabetes and street drug use.
So how is the aneurysm discovered in the original family member in the first place? You’ve heard the saying, “He had an aneurysm and died.”
An aneurysm is a bulge in a blood vessel; the bulge has weakened walls that are at risk for dissecting.
People don’t “have an aneurysm and die.” They have a ruptured aneurysm – meaning, it dissected or burst, resulting in a hemorrhage.
These bulges usually have no symptoms and can be stable for many, many years—and in fact, people could live well into old age without any incident.
Only upon autopsy is the aneurysm discovered, and there may even be two or three of them – all silent for that person’s entire long life.
Most are discovered by accident when the head is scanned (CT, MRI) for an unrelated reason such as head trauma from a car wreck.
So that family member is then discovered to have a silent aneurysm. Their parents, siblings and kids should undergo an MRI. An MRI emits no radiation.
If an MRI detects an aneurysm, it may or may not require treatment, but at a minimum, will require monitoring. In other words, not all aneurysms are time bombs.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Sources:
health.clevelandclinic.org/2014/09/if-your-relative-has-an-aneurysm-you-might-have-one-too/
ncbi.nlm.nih.gov/pubmed/23733552
Exercise Guidelines after Brain Aneurysm Coiling or Clipping

Are you a weightlifter or runner with an unruptured, newly coiled aneurysm?
Just what does “return to full activities” really mean?
Exercise is encouraged by surgeons who clip or coil brain aneurysms, but the term “exercise” needs to be defined.
Patient Recovered from Coiling or Clipping of an Unruptured Brain Aneurysm: Exercise Guidelines Including Weightlifting
“Six months after treatment, I do not put my patients on any restrictions,” says Farhan Siddiq, MD, a neurosurgeon with University of Missouri Health Care.
“There are no activity or weight-limiting restrictions,” continues Dr. Siddiq.
“I encourage patients to resume normal life and be active. I encourage daily exercise of whatever degree they prefer. I have not had any patients have any problems with that.”
So if you were, prior to the discovery of your cerebral aneurysm, a bodybuilder, kickboxer, Crossfitter, skier, rock climber, mountaineer or marathon runner, you can resume these activities full-force after the six month mark.

If you were never into any intense exercise, you can certainly take it up, be it powerlifting, high intensity interval training, judo, whatever you please.
Don’t let your coiled or clipped aneurysm stop you.
Dr. Siddiq adds, “If coiling or clipping is inadequate or if a patient may require later treatment, then I might recommend some restrictions; but that is very rare.”
What About Short Term Exercise Guidelines for Clipped or Coiled Brain Aneurysms?
Avoid lifting anything more than 10 pounds for three days after the coiling or clipping.
It’s important to discuss lifting and activity restriction with your doctor for the short-term.
This includes a month out, and six months out, from the procedure.
But remember, you’ll need to wait six months, depending on the intensity of the exercise, to resume certain high-level activities.
This excludes easier activities such as gardening and brisk walking.
But you would have to wait six months to resume pushing your limits with big strength training moves such as the barbell squat and bench press.

Dr. Siddiq is fellowship-trained in endovascular surgical neuroradiology and vascular neurology from the University of Minnesota Medical Center. His areas of special focus also include brain aneurysms and carotid disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: vecteezy.com
Sources:
thewaltoncentre.nhs.uk/uploadedfiles/documents/Elective%20Coil%20occlusion%20of%20brain%20aneurysm%20Patient%20Information.pdf
mayfieldclinic.com/PE-Coiling.htm
Life after a TIA: 5 Steps to Kill the Fear of Another One

Once you’ve had a transient ischemic attack, life as you know it will never be the same — but there are five measures you can take to regain power over your life. (more…)
Will the DASH Diet Help Prevent a Second TIA?
If you’ve suffered from a TIA, perhaps you’re wondering if the DASH diet will help prevent another one of these mini-strokes, which can mean a massive stroke in the near future.
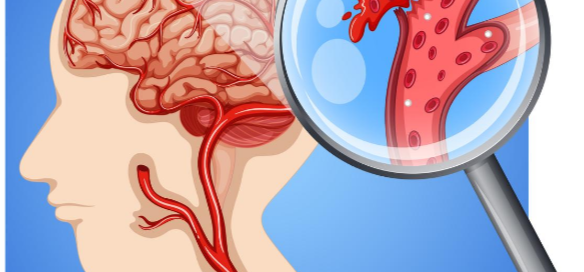
Can an Aneurysm Cause Very Brief Stabbing Head Pain?
Can your “jabs and jolts” stabbing head pain be caused by an aneurysm that’s about to rupture?
Aneurysm pain from rupture is classically a “thunderclap” headache: sudden in onset, and excruciating, the worst head pain ever. (more…)
Twitching Muscles: Fasciculations vs. Myokymia
What you think is a muscle twitch from MS (myokymia) may actually be just a harmless fasciculation; there’s a way to tell the difference with these two kinds of muscle twitching. (more…)
Can Multiple Sclerosis Start with a Twitching Nose?

There actually is a type of facial twitch that’s associated with multiple sclerosis.
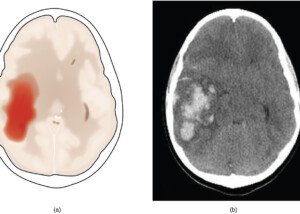
Can a Brain Tumor Cause Eyelid Twitching?
A brain tumor can cause an eyelid to droop, but the big question is: Can a brain tumor cause an eyelid to twitch?
Many people who have a persistently twitching eyelid are terrified that this is being caused by a brain tumor.
“Eyelid twitching is very common and is usually benign, but can be serious in rare cases,” begins Kaushal M. Kulkarni, MD, board certified ophthalmologist and neuro-ophthalmologist in private practice in New York.
Usually, when an eyelid twitches, there’s something going on with the tiny muscles of the eyelid.

Credit: Leitz31337 at English Wikipedia
These very tiny muscles are contracting—and this is what you feel and see as the twitching (fasciculations).
Do not confuse a twitching eyelid with a drooping one.
There are many causes of the drooping, which is called ptosis. One is a brain tumor.
So you’re probably wondering, “If a brain tumor can cause an eyelid to droop, can it also cause the eyelid to twitch?”
Is the Twitching in just One Eyelid?
Dr. Kulkarni explains, “Intermittent eyelid twitching or fluttering in just one eyelid, which comes and goes, is very common and usually due to a benign condition called eyelid myokymia.”
Myokymia is the medical term for harmless muscle twitching on a very small scale.
“It is commonly brought on by stress, lack of sleep or caffeine,” says Dr. Kulkarni. Sometimes, an eyelid twitches for no real reason.
“However, if the twitching involves more than just the eyelid and involves the head, face, cheek, mouth or jaw, it needs to be evaluated by a doctor.”
Are BOTH Eyelids Twitching?
“If the twitching or spasm is in both eyes, this is usually a condition called blepharospasm,” says Dr. Kulkarni.
“This is a condition that causes intermittent spasm of both eyelids for reasons we do not completely understand.
“It is a benign condition, hence the name benign essential blepharospasm. It can usually be treated with Botox injections around the eye.
“In fact, this was one of the original uses for Botox. It was only after patients with blepharospasm who received Botox injections and noticed that their wrinkles disappeared that Botox became popularized and marketed as it is today!”
The thing about BOTH eyelids twitching (bilateral fasciculations) is that this is a very reassuring sign that the cause is not likely a brain tumor.
When a brain tumor affects the eye or surrounding structures, it is almost always just one eye – and the same eye at that.
Same side twitching but…are there also spasms of the nose, cheek, lip, chin, etc.?
This is called hemifacial spasm: one side of the face. Botox may be effective depending on cause.
“If there is an artery compressing the facial nerve, a neurosurgical procedure can sometimes relieve the spasm,” says Dr. Kulkarni.
Brain Tumor As Cause of Twitching Eyelid
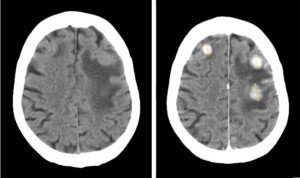
The three lit-up spots are three separate tumors. Jmarchn commons.wikimedia.orgwikiFileBrainMetastasisFromBreastCancer
“Anyone with hemifacial spasm needs to have a brain scan to check for a brain tumor compressing the facial nerve,” says Dr. Kulkarni.
This nerve is one of the cranial nerves that leads to the brain.
There is a type of brain tumor — a Schwannoma of the facial nerve in the cerebellopontine angle – that can cause an eyelid to twitch.
This brain tumor is rare – and benign. Plus, by the time it would ever cause eyelid fasciculations, it would certainly also be causing other symptoms such as hearing loss, tinnitus or dizziness.
Another tumor that affects the brain and can cause an eyelid to twitch is a meningioma (90 percent are benign).
However, a malignant tumor of the brain stem can cause eyelid twitching, and over time it will progress to hemifacial spasm.
In all fairness, it must also be mentioned that the worst brain tumor that an adult could have, the glioblastoma multiforme, is capable of causing a twitching eyelid.
The Journal of Neurosurgery (March 1962) notes the case of a man, 31, who had “loss of consciousness and dizzy spells associated with involuntary twitching of the right eyelid and right shoulder.”
However, this case report describes a very rare situation of a GBM spreading beyond the cranium. GBMs are rare enough as it is, with a diagnosis rate of two to three per 100,000.
Putting Things into Perspective
Eyelid twitching that originates from a brain tumor is extremely rare.
Furthermore, by the time the fasciculations arise, there will likely be other symptoms (e.g., other facial disturbances, vision issues, headache, vomiting, seizures, weakness).
Just rubbing an itching eyelid can make it flutter.
Relax, don’t panic over this extremely common condition that you’ve probably experienced many times during childhood and didn’t give it a second thought. Oh, to be a kid again!
Eye-Related Symptoms of Brain Tumor: Compilation from the Following Sites:
Webmd.com, cancer.net, mayoclinic.org, cancercenter.com, medlineplus.gov
• Changes in vision
• Partial or complete loss of vision
• Double vision
• Blurred vision
• Loss of peripheral vision
• Inability to look upward
• Drooping eyelid (ptosis)
• Pupils different size
• Uncontrollable eye movement
• Bulging eye
Non-Tumor Brain Causes of Eye Twitching from Mayoclinic.com
• Tourette syndrome
• Oromandibular dystonia, facial dystonia
• Multiple sclerosis
• Dystonia
• Cervical dystonia
• Bell’s palsy
These non-tumor brain conditions, however, almost always come with other symptoms alongside the twitching eyelid.