Back and Arm Strength Training for Older People

Many senior age men and women do back and arm strength training wrong.
As a fitness expert, I like to point out that old age is never an excuse for poor form. (more…)
Sitting Disease Causes Fat Buildup Around the Organs
Excessive sitting is strongly associated with how much fat surrounds your organs.
This is the most dangerous kind of fat, called visceral fat, and is waiting for anybody who spends a lot of time sitting. (more…)
Amount of Exercise Needed to Prevent Heart Failure in Old Age

Never believe that congestive heart failure is a required part of getting old, because a study shows that exercise can help prevent this very common condition. (more…)
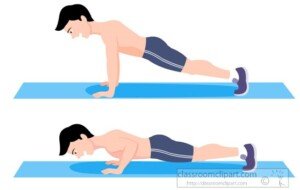
10 Pushup Mistakes Women Make; How to Correct Them

There are 10 pushup mistakes that many women make and don’t even realize it.
But they can be eliminated very easily.
Here they are, in no particular order.
Being too presumptive.
A big mistake is to automatically assume you’re “too weak” to do pushups. Well, this is partly true.
You WILL be too weak to do pushups — if your body is not well-trained in chest pressing motions and especially if you’re carrying extra weight.
Because this article is about the pushup mistakes that women make, I’m not going to go into detail about how to get strong enough to do a pushup.
But in a nutshell, getting stronger on free weights and chest press equipment will land you in pushup territory. Do not underestimate yourself if you want to nail a set of pushups one day.
Trying to learn pushups by doing only pushups.
This erroneous approach overlaps the previous mistake. For an untrained woman, pushups are just plain hard. Even untrained men can’t do them.
The best way to train for pushup ability is to do free weight and machine chest and shoulder presses.
I speak from experience. I don’t have to do pushups to maintain my ability to do them. The ability is a natural baseline function, courtesy of my other chest and shoulder routines.
Quantity over quality.
I’ve seen women doing many reps – of incomplete and/or poorly formed pushups. Three or four solid, perfect, full range motion pushups beat out 12 half-baked pushups any day.

Shutterstock/Slatan
Focus on pulling off one perfect pushup with full range of motion, even if your knees must be on the floor, or your hands on something elevated (which will also make the movement easier).
When you can complete one, then your next goal is two, and so on. Rather than look ahead thinking, “I gotta complete eight even if they suck,” think instead, “One pushup at a time; let’s make THIS one good!”
Incomplete range of motion.
This results from not being strong enough to complete the ROM. Fine. But complete ROM is important for progress.
So what to do? How about adjusting your body position to accommodate the lack of strength?

Shutterstock/Alexander_Safonov
Either do the pushups off your knees or elevate your hands on a bar or edge of a bench.
Bowing to a statue.
Many women who do knee pushups use wrong form. They bow down with each repetition. Sometimes their butt is higher than their shoulders at the bottom of the movement.
The form for a standard (feet-only) pushup applies to a knee and hand elevation version.
Getting too fancy.
I’ve seen women struggling with various versions that are just way beyond their capabilities.
Do not assume that fighting through a set of wobbly one-hand-on-medicine-ball and one-leg-up-in-the-air pushups with incomplete ROM is a better workout than a set of simple, old-fashioned pushups with picture perfect form.
Keep it simple. The fancy stuff is not more effective at shaping the physique or burning fat.
Hands too far apart.
Oddly, I’ve seen this more among women than men. The further apart the hands, the more strain on the shoulder joint, namely the rotator cuff tendons.
Misaligned body segments.
The back of your head, upper back and butt should be aligned, so that all three sections would evenly touch against a giant ruler if a giant ruler were to be placed alongside the back of your body.
Hip sag and scapular jut.
When the body portions are not aligned, often the hips markedly sag and the scapular bones jut out.
Twenty reps of these are no match for the worthfulness of only three perfect “real” pushups.
Not warming up.
For more trained individuals, starting a workout with pushups may work just fine for them.
But if you’re struggling with this compound movement, you’ll want to consider warming up first with other chest routines.
For example, after completing your bench press routine, your shoulder joints will be plenty warmed up for pushups.
Don’t think you must do pushups first with the idea that if you do anything else before them, you’ll then be too fatigued to do any sort of pushups.
I find that I’m stronger with pushups after they are preceded by two different chest routines, say, dumbbell presses and Hammerstrength seated chest presses.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Freepik.com
Do You Get a Cardio Workout Climbing Wall Routes?
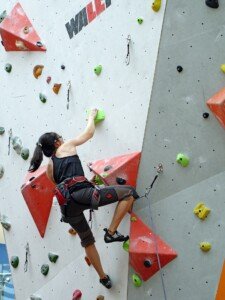
Though rock wall climbing can be seen as a resistance workout, there can be a good cardio component to this kind of activity, depending on some factors. (more…)
Strength Training for Women: Machines or Free Weights or Both?

If a woman had to choose just one type of strength training, should it be free weights or machines?
After all, there are advantages – and disadvantages – to both approaches of resistance training. (more…)
How Busy People Can Burn LOTS of Fat Minutes a Day with Exercise
You need only a few minutes here and there throughout your busy day to burn fat; there’s no such thing as not having time for fat-burning exercise.
You need to know the correct technique.
This exercise technique has been shown by many scientific studies to be highly effective at burning fat.
The technique can be applied across the board as far as type of movement (e.g., walking, pedaling, stepping, running, hopping).
One of the studies that shows the effectiveness this fat burning approach was done by McMaster University researchers, as they demonstrated that just six minutes of intense exercise a week equates to 60 minutes of medium intensity exercise.
Find the setting of your preferred type of cardio equipment that requires you to push your hardest to maintain.
You should be able to maintain it for half a minute, after which you’re very exhausted. Find your settings for this: 30 seconds takes it all out of you.
NOTE: Treadmill users should NOT hold onto the machine other than to change the settings.
Once the settings are in place, KEEP YOUR HANDS OFF. If you can’t, you’re going too fast or the incline is too high.

Shutterstock/gpointstudio
Between each 30 second blast, you go easy for 2-4 minutes. Do 6-8 work intervals total. Then you’re finished.
The McMaster study examined people who did these “sprint” exercises only three times per week.
The report said that in the study group, muscles had a substantial increase in citrate synthase, which is an enzyme suggestive of the muscle cells’ ability to use oxygen: fat burning.
Lack of time to exercise for very busy people, then, no longer holds water.
McMaster University conducted another study that shows a busy person with no time to exercise will actually get more bang out of their buck with “sprint” training, also known as high intensity interval training or burst exercise.
This other study, however, reveals that interval training need not be your absolute maximum effort in order to still be very effective.
Study author Professor Martin Gibala explained in the paper, “Doing 10 one-minute sprints on a standard stationary bike with about one minute of rest in between, three times a week, works as well at improving muscle as many hours of conventional long-term biking less strenuously.”
The less-than “all out” effort is ideal for those busy women and men who are new to exercise, are older or have an injury to work around.
Gabala, et al, has demonstrated that these brief spurts of high exertion are just as effective at also cutting one’s risk of diabetes, strokes and even heart attacks.
In fact, to obtain the same results from traditional exercise, the busy individual would have to invest over 10 hours of medium-level bicycling over a 14 day period!
When I was a personal trainer I’d inform my time-crunched clients that the fat burning effects are incited by the increased release of human growth hormone and testosterone during the periods of high intensity.
These hormones are natural fat burners, and long duration cardio does not trigger higher release of these hormones.
With intensity interval training, in which you are pedaling or walking or jogging at work-effort for anywhere from a total of three to 10 minutes, more fat will be burned — much more — than if you did an hour of “slow” or steady state cardio!
Do the math: How much time does the busy indiviual need to perform six, 30-second intense bursts, including the several minutes’ rest in between?
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Sources:
sciencedaily.com/releases/2005/06/050602113341.htm
sciencedaily.com/releases/2010/03/100311123639.htm
How to Burn More Fat if You Have a Slow Metabolism

Is your metabolism freaking slow and preventing you from losing weight despite your daily efforts?
I’ll bet the farm that you have not tried the very exercises that will fire up your lethargic metabolism. (more…)
Can Exercise Cause INTENSE Chest Pain from GERD?

You may already know that GERD can cause chest pain, but what about severe or intense pain, which can frighten people into thinking that their heart is in serious trouble? (more…)
Can Laryngopharyngeal Reflux Cause Nasal Congestion ?