You Know You’re No Longer Fat AND Healthy When…

Is it when your fasting blood sugar gets over 100?
Is it when your systolic blood pressure gets over 140?
Is It Worthwhile for Smokers to Run?
It’s been said that smoking undoes any jogging or running, or that it’s useless to run if you’re a smoker.
Nothing could be further from the truth.
You can’t really believe that a smoker’s body will be exactly the same – whether he smokes only, or whether he smokes and is a runner.
No body is unaffected by vigorous physical activity – whether its lungs are polluted by cigarette smoke or some other deleterious agent is at play, such as a junk food diet or excess belly fat.
Research shows what common sense says: Vigorous activity, such as running, improves the lung function of smokers.
So if you’re a smoker, don’t EVER feel that donning some running shoes and going out for a jog is a pointless thing to do.

The Study
• Over a period of 10 years, 3,912 adults 27 to 57 were tracked.
• They were deemed active if they exercised at least twice a week with duration of one hour per week minimum.
• Associations between exercise and lung function were apparent among current smokers.
The paper points out that smokers are at a higher risk of poor lung function, and that physical activity such as running is very important for them.
Another key finding was that subjects who were physically active at the study’s conclusion, including those who started out sedentary during the tracking period and then became active, had much greater lung function than participants who were sedentary.
There is an undeniable correlation between exercise and lung health – and this includes among smokers.
Look at it this way: Suppose there are identical twins with the same diet, same weight and same lifestyle, including smoking the same number of cigarettes (same brand) a day.
But one twin runs five miles a day. Is it really plausible that the twin who runs can’t possibly have much better lung function than his sedentary genetic counterpart?
Another Point to Consider
“Yes – it [running] will improve lung function and also motivate smokers to cut down as they sense their loss of fitness and how good it feels to get more fit,” says Richard Honaker, MD, Chief Medical Advisor at Your Doctors Online, with 30+ years’ experience as a primary care physician.
“Though, it does NOT nullify the damage from smoking unless it causes quitting,” adds Dr. Honaker.
The full study results are in the Feb. 2018 issue of Thorax.
 Dr. Honaker has been recognized by D Magazine as one of the Best Doctors in Dallas several times and a Texas Super Doctor by Texas Weekly. He’s also a recipient of the Physician Recognition Award from the American Medical Association multiple times.
Dr. Honaker has been recognized by D Magazine as one of the Best Doctors in Dallas several times and a Texas Super Doctor by Texas Weekly. He’s also a recipient of the Physician Recognition Award from the American Medical Association multiple times.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Source: sciencedaily.com/releases/2018/02/180205102738.htm
How Noise Like Traffic Can Damage Your Heart Health

Research shows what smart people have known all along: Noise pollution such as traffic harms the heart.
Types of Noise that Can Raise the Risk of Developing Heart Disease
• Traffic
• Aircraft
• Industrial
• Recreational
Excessive environmental noise pollution, even when below hearing-harmful levels, can cause a number of damaging health effects such as sleep disturbance, physiological stress and cognitive impairment.
Research also suggests that noise can negatively affect the heart.
According to the Environmental Protection Agency, noise pollution is any unwanted or disturbing sounds, and its impacts should be calculated not just by how loud the noise is, but by how long the exposure is (APHA, 2013).
Research indicates that increased nighttime noise exposure increases levels of stress hormones and vascular oxidative stress and is said to be associated with vascular damage, stress response, cell death and changes in the expression for genes responsible for the regulation of vascular function (Münzel et al., 2018).
Traffic — Among the Most Unbearable Sounds
Hearing continuous traffic (especially trucks barreling by on a frequent basis) while inside one’s home has also been shown to increase blood pressure, heart rate and cardiac output, likely the result of the release of stress hormones (Munzel, Gori, Babisch, & Basner, 2014).
The repercussions of this noise exposure are not as obvious when studied in occupational settings.
How Noise Pollution Damages Your Heart
It is believed that noise will affect the autonomic nervous system and endocrine system, in turn disrupting the homeostasis of humans.
Stress will lead to the activation of different neuro-hormonal systems which attempt to cope with the stressor.
These include activation of sympathetic responses (fight or flight response) and corticosteroids (a defeat reaction) (Munzel et al., 2014).
This stress response changes a number of physiological functions including blood pressure, endothelial dysfunction, cardiac output and blood lipid levels.
The noise-induced dysregulation and disturbed metabolic function encourages the development of chronic cardiovascular disorders (Babisch, 2011).
Can you prevent cardiovascular problems caused by noise pollution?
- It’s advised to be mindful of environments with excessive noise and perhaps even keep a pair of earplugs in your bag or pocket in case you find yourself in these environments.
- You may want to invest in a pair of custom fit earplugs which can be obtained from your local audiologist.
- Another preventive measure is to install “acoustic curtains” if the noise is coming into your home from outside.
- Finally, keep a fan running to drown out outdoor noise pollution. An indoor water fountain or white noise generator will also help.

Dr. Strom is a member of the American Speech Language and Hearing Association and has received several awards including Brooklyn College’s Excellence In Audiology Award.
 Victoria J. Dillon is a doctoral audiology student interning at Advanced Hearing NY.
Victoria J. Dillon is a doctoral audiology student interning at Advanced Hearing NY.
.
Top image: Shutterstock/michaelheim
Sources
apha.org/policies-and-advocacy/public-health-policy-statements/policy- database/2014/07/16/12/50/environmental-noise-pollution-control
doi.org/10.4103/1463-1741.80148
doi.org/10.1093/eurheartj/ehu030
doi.org/10.1016/j.jacc.2017.12.015
Common Conditions that Vulvodynia Is Associated With

Vulvodynia, a painful disorder that causes great distress for many women, is associated with a number of conditions. (more…)
Vulvodynia vs. Vaginismus: Doctor Explains the Differences

A doctor who specializes in chronic pelvic, genital and sexual pain disorders describes the differences between vulvodynia and vaginismus, terms that are commonly used interchangeably.
- Is it vulvodynia?
- Is it vaginismus?
- Is there a difference between vulvodynia and vaginismus?
Yes!
“These two conditions are all too commonly confused with one another,” says Robert J. Echenberg, MD, founder of The Echenberg Institute for Pelvic & Sexual Pain, and co-author of “Secret Suffering: How Women’s Sexual and Pelvic Pain Affects Their Relationships.”
Vulvodynia Symptoms vs. Vaginismus in Day to Day Living
“Dynia means pain, so vulvodynia means pain in the genital region of the female – the ‘saddle area’ between the inner thighs and extending from the clitoris back to the tailbone,” explains Dr. Echenberg.
“Because this area of the body is so private and has so much social stigma and secretiveness, there remains continuing confusion about the many conditions that may contribute to painful sensation with sitting and a variety of daily bodily functions such as urination, defecation and especially penetrative vaginal activities as in sexual intimacy, use of vaginal tampons and even tolerating inspection for a routine Pap smear,” continues Dr. Echenberg.
“Vaginismus, on the other hand, refers to an involuntary tightening or clenching of the pelvic floor muscles – especially the ‘Kegel’ muscles at the base of the entire pelvic floor.
“In the case of vaginismus, there does not need to be an accompanying painful condition causing that tightening – but can be secondary to any reminder or memory of previous actual or perceived trauma or pain in the pelvic region.
“In these cases, the pelvic floor muscles can be so tight as to cause a great deal of pressure sensation and the uncomfortable pressure feeling of something ‘filling or falling out’ of the vaginal or rectal region.
“Vulvodynia always causes variable degrees of muscular spasm or clenching as well, which is the body’s natural protective mechanism to fend off any further threat of touch or actual painful penetrative activity”.
Dr. Echenberg has found in his many years of caring for these conditions that the best term for muscular spasm, secondary to a physical pain condition, should be hypertonic pelvic floor dysfunction, and not “vaginismus.”
Hypersensitivity: Subset of Vulvodynia
A patient may have both vaginismus (HPFD) and vulvodynia – and the latter may be a subset rather than all-out vulvodynia.
This subset “is when the tissue between the vaginal lining and the outside hair-bearing skin on the genital area, the delicate skin inside the inner lips of the labia, becomes sensitive to even slight touch such as the gentle application of a Q-tip to the area,” explains Dr. Echenberg.
A patient might describe this as overly sensitive nerve endings – even when she is merely removing bits of tissue paper that have broken off from a previous wiping after urination.
Dr. Echenberg continues, “This location is known as the ‘vulvar vestibule.’ and when this area is highly inflamed and sensitized, the term used is vestibulodynia or vestibulitis.
“This subset of vulvodynia is the most common reason for entrance pain in reproductive age women.”
Common Descriptors
Dr. Echenberg notes that the following descriptors by patients are common with vestibule inflammation and sensitivity.
- Dryness
- Irritation
- Burning
- Stabbing
- Ripping, tearing
- Hot poker
- Ground glass
- Sandpaper
“There are many theories about the cause of such severe localized pain, but most research is indicating that excessive ‘aggravation’ and sensitivity of the nerve endings in that skin at the vaginal opening is the underlying problem.”
Dr. Echenberg explains that in those women who suffer with vulvodynia and/or vestibulodynia, “The muscles are reacting to painful stimuli arising from any number of possible generators of pain in the pelvic and genital region.
“These muscles are tightening because of perceived need to stabilize and ‘splint’ the pelvic region, just as all the muscles in the arm and neck will spasm and protect against movement of the arm when there is a shoulder separation or other injury.
“Eventually, this clenching becomes persistent and difficult to ‘loosen up’ – just as in the condition of ‘frozen shoulder.’”
In short, Dr. Echenberg acknowledges that there is understandable confusion between the terms vulvodynia and vaginismus, but he reminds us that the experience of the woman may be the same in both.
“Pelvic muscle tightening – whether secondary to an ongoing pelvic pain disorder such as painful bladder syndrome/interstitial cystitis, irritable bowel syndrome, endometriosis, pelvic neuropathies, etc., (pelvic floor dysfunction) – or whether from long term fear or anticipation of pain (vaginismus), the result can severely limit the normal function of the genital area.”
Vulvodynia and Vaginismus Myths
The two big myths are that these disorders are “all in a woman’s head” or are always the result of past sexual abuse or assault.

These myths are not grounded in reality. For example, a virgin who’s never even been fondled can still have vaginismus (hypertonic pelvic floor dysfunction) or vulvodynia.
A 14-year-old virgin may accidentally discover she has either of these conditions when first attempting insertion of a tampon (though will very likely not know her situation has a medical name).
Remember, it’s that anticipation and fear of penetration – even though it’s self-penetration – that induces the muscles to spasm. She cannot relax them like she can relax a flexed bicep.
“Because many gynecologists and other specialists are not currently trained or familiar with pelvic and genital pain conditions, they often fall back on the old assumption that most of these young women must have suffered previous sexual abuse,” says Dr. Echenberg.
He gives examples of many of his young patients having been athletes with such sports as gymnastics, soccer, softball and even years of dance, who have never been abused but who have had multiple cumulative injuries in the “saddle” region – resulting in long term traumas – long since healed – leading to these disorders.
It’s also possible for a patient’s negative anticipation of penetration to have no known etiology.
“Neuropathic and muscular ‘memory’ will then trigger involuntary clenching,” and Dr. Echenberg says that “it is not clinically important whether neuromuscular spasm is called vaginismus, vulvodynia or pelvic floor dysfunction.
“The treatment approaches will all be similar and will almost always involve a pelvic floor physical therapist to help ‘retrain and reboot’ the brain/body connection.”
 Dr. Echenberg combines the most current neuroscience on chronic pain processing, a very personalized bio-psychosocial model approach and 40+ years of medical experience to treat his patients.
Dr. Echenberg combines the most current neuroscience on chronic pain processing, a very personalized bio-psychosocial model approach and 40+ years of medical experience to treat his patients.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ruigsantos.
Why Is Vulvodynia So Often Misdiagnosed? Doctor Explains

Vulvodynia causes painful sex and other kinds of pain “down there,” affects millions of women, yet is so often misdiagnosed.
Why is this? (more…)
Elderly Take Longer than Younger to Realize They’re Falling
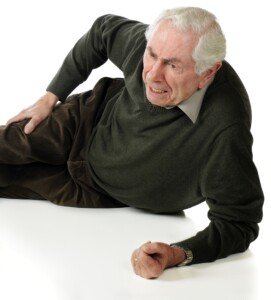
Milliseconds count when you realize you’re falling, and the lag in milliseconds that elderly people have compared to younger is part of the reason they’re more likely to end up flat on the ground. (more…)
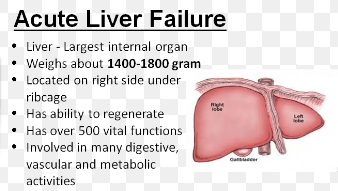
Olive Oil vs. Fish Oil: Which One May Ruin Your Liver?
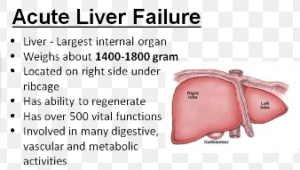
Both olive and fish oils are considered the “healthy oils” or “good fats,” but evidence shows that one of them can damage the liver.
The liver is responsible for hundreds of functions. The last thing you want is compromised liver function. (more…)
How High Must Blood Pressure Get to Cause Stroke?

Is a stroke pretty much guaranteed once your blood pressure reaches a point higher than a specific number?
When the top number (systolic) is at least 140 and the bottom number (diastolic) is at least 90, this is considered high blood pressure (hypertension). (more…)
Can Chronic Stress and Anxiety Elevate the A1C?
Chronic stress or anxiety causes the body to be in a chronic state of fight or flee, and blood sugar is involved.
The A1C test is more accurate than the fasting glucose test for detecting diabetes or prediabetes.
The A1C shows the average blood sugar (glucose) level for the past two to three months. (more…)