Cancers that Can Mimic TMJ Symptoms & Lead to Misdiagnosis
There are several kinds of cancer that can mimic TMJ symptoms and lead to misdiagnosis.
And in fact, misdiagnoses of TMJ disorder has actually been made in some cases. (more…)
How to Role Play with Kids to Teach Stranger Danger
You can’t just lecture “Don’t talk to strangers” to young children; you must role play and role play good and hard.
Can You Have TMJ Without Jaw Clicking and Popping?
TMJ causes so many symptoms—many you’d never even imagine—that some patients with full-blown TMD never have a single pop or click of their jaw.
Clicking, popping and grinding noises coming from one’s jaw are almost always caused by TMJ disorder. (more…)
Can TMJ Disorder Symptoms Be on Only One Side?

Do not let what seems like TMJ symptoms on only one side of your face frighten you into thinking that this means cancer. (more…)
TMJ Headache vs. Brain Tumor Headache: Symptom Comparison

TMJ disorder can cause a fierce headache, but so can a brain tumor.
In fact, the onset of brain tumor headaches can mimic head pain caused by a temporomandibular joint disorder.
Though the popping and clicking of “TMJ” gets a lot of attention, TMJ disorder (also known as TMD) can also cause considerable headaches, plus pain in the jaw, face and neck.
How a TMJ Headache Feels Compared to a Brain Tumor Headache
“TMJ headache is usually on both sides of the head, worse in the morning and may be associated with trouble eating or moving the jaw,” says Brijesh Chandwani, DMD, BDS, Diplomate, American Board of Orofacial Pain, with Connecticut & NY TMJ.
However, a brain tumor headache can also be on both sides of the head AND worse in the morning!
During sleep fluid builds up in the brain, caused by the mass, and this fluid creates pressure that, come morning, manifests as a headache which, as the day goes on, subsides. But brain cancer can also cause headaches at any time.
“While TMJ headaches are uncommonly associated with brain cancer, failed treatment response and symptoms such as tingling or numbness sensation, dizziness, sudden onset of pain should warrant a visit to a neurologist,” advises Dr. Chandwani.
“I had a patient several years ago who had headaches along with sudden restriction of his jaw and he was diagnosed with a benign brain tumor.
“Some patients with brain cancer just feel a headache and a lack of normal sensation in the jaw and head region (abnormal ear or taste sensation, etc.).”
If a person has headaches (and orofacial pain) that are attributed to TMJ disorder, and TMD treatments have failed, then a visit to a neurologist is in order to see if a brain tumor might be causing these symptoms.
A paper by Levitt et al in The Journal of Craniomandibular & Sleep Practice states:
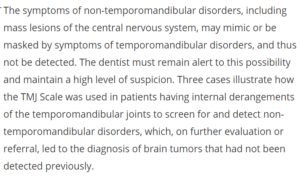

Dr. Chandwani has 15+ years of experience focusing on TMJ disorders and sleep disorders.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/YAKOBCHUK VIACHESLAV
Sources
tandfonline.com/doi/abs/10.1080/08869634.1991.11678361
onlinelibrary.wiley.com/doi/abs/10.1002/j.1875-595X.2000.tb00808.x
oralhealthgroup.com/features/extracranial-meningioma-mimicking-a-temporomandibular-joint-disorder/
Tenderness Under the Chin: Causes Including TMJ Disorder

A tenderness that develops under one’s chin can become quite worrisome, bringing to mind the worst possible scenarios as to cause. (more…)
Headaches, Dizziness, Eye Pain, Blurry Vision: Likely Cause

If you’ve been suffering from headaches, dizziness (vertigo), eye pain and blurred vision, and have seen a dozen specialists who’ve failed to figure out the cause, let alone an effective treatment… (more…)
Can Night Sweats Be Caused by TMJ Disorder?

Before you panic that your night sweats are caused by lymphoma or HIV, there’s a possibility they’re caused by TMJ disorder.
Night sweats can be bad enough to require changing one’s clothes.
“Patients with TMJ disorders frequently have a destructive bite with worn down teeth that forces their lower jaw backwards,” begins Jeffrey Haddad, DDS, of Doolin Haddad Advanced Dentistry in Rochester, MI.
“This backwards positioning can cause narrowing of a person’s airway while they sleep, which leads to obstructive sleep apnea.
“Conversely, a person with an obstructed airway may clench and grind their teeth, which can wear down the teeth and deteriorate the bite, leading to TMD symptoms and pain.”
“We have seen a significant increase in the number of patients we treat for combined obstructive sleep apnea/TMD since our practice began monitoring and treating sleep apnea in our practice.
“In fact, it is now protocol to have every one of our TMJ patients utilize our sleep monitor to determine if a sleep breathing disorder is present.
“Night sweats are a very common symptom of a sleep breathing disorder. Therefore if a patient is experiencing this, it could be a result of a combined TMJ/sleep breathing disorder.”
Night Sweats and Sleep Apnea Link
“Night sweats are associated with several sleep symptoms,” says a paper in the Annals of Family Medicine (Sept. 2006).
“Both night sweats and sleep disturbances are commonly experienced by adult primary care patients,” continues the paper.
“When their patients report night sweats, clinicians should consider asking about sleep quality and sleep-related symptoms.”
A report in the British Medical Journal Open states: “The prevalence of frequent nocturnal sweating was threefold higher in untreated OSA [obstructive sleep apnea] patients than in the general population and decreased to general population levels with successful PAP therapy. Practitioners should consider the possibility of OSA in patients who complain of nocturnal sweating.”
TMJ, Night Sweats, Sleep Problems
“Recent data indicates an estimated 75% of people with TMD also have sleep breathing disorders, and 52% of people with sleep disorders have TMD problems or are prone to them in their lifetime,” says Dr. Haddad.
“These are essentially the same patients with poor jaw posture, resulting in either pain and discomfort and/or a compromised airway.
“We have refined our treatment approaches and the design of our oral therapy appliances as more and more research connect TMJ and sleep disorders.”

Dr. Haddad lectures nationally on cosmetic dentistry, TMJ disorders and practice marketing, and utilizes the latest technology to ensure the utmost in patient comfort and care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Damir Khabirov
How TMJ Disorder Can Affect Your Eyes and Vision
If you’re having problems with your eyes that doctors can’t figure out, it’s possible that a TMJ disorder could be the cause. (more…)
How Well Can a CT Scan Identify Ovarian Cancer?

Ovarian cancer is one of the deadliest cancers because it’s usually not discovered until it has spread.
A CT scan is sometimes taken in women who have symptoms suspicious for ovarian cancer. (more…)