How Many CT Scans Should a Head Trauma Patient Have?
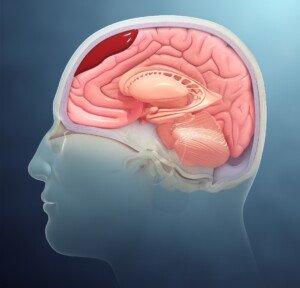
Just how many CT scans are needed if someone has a small brain bleed resulting from a not-so-severe head trauma?
This can be banging their head on the bottom of the bathroom sink after kneeling on the floor and getting up.
Is it possible for a doctor to over-order CT scans in a head trauma patient with a chronic subdural hematoma (slow brain bleed)?
Years ago my mother had seven CT scans in 29 days due to a chronic subdural hematoma.
Certainly, she is not the only person to ever undergo many CT scans of the head in a short period of time.
Concerns of Radiation Exposure of Multiple CT Head Scans over a Short Time Period
What About for Milder Head Trauma?
The January 2013 issue of Neurosurgery has a report that questions the need for repeated CT scans in patients with non-severe brain bleeds.
“The available evidence indicates that it is unnecessary to schedule a repeat CT scan after mild head injury when patients are unchanged or improving neurologically,” says the paper.
In the case of my elderly mother, the diagnosis was chronic subdural hematoma (nowhere near as severe as acute subdural hematoma).
• On 11/28/10 my mother had a CT scan after hitting her head.
• Next day she had another one. Both were normal.
• However, 42 days later (01/09/11) she had another CT scan after awakening with neurological symptoms. That image showed the brain bleed.
• Two days later she had another CT scan following surgical draining of the blood/fluid from her brain.
• About a week later she had another one because she was experiencing new-onset neurological symptoms — that were ultimately attributed to an anti-seizure drug given pre-emptively for the head injury.
On 01/24/11 she had another computerized tomography (scheduled), but this one was based on yet a new set of neurological symptoms (that were soon found to be caused by a recurrence of the brain bleed).
The next day she had yet another CT scan (in the ER) following acute delirium. The ER doctor said the delirium was an adverse reaction to the Medrol Pak (oral steroids) that were prescribed for the injury.
On 01/27/11 she had another imaging following her second surgical draining.
That all seems like a lot of head CT scans, but it’s important to keep ahead of brain bleeds, and to weigh the risk vs. benefits.
It would take many years for radiation exposure to cause adverse effects, if any, and if the patient is already elderly , the concern over radiation becomes smaller.
The standard protocol is to give repeated CT scans after even mild head trauma, since bleeding in the brain can be life threatening or cause permanent neurological damage.
Whether the patient truly needs routine follow-ups based on a timeline, vs. another scan based on symptoms or what the previous scan showed, is up to the treating physician.
The Neurosurgery study authors favor neurological examination as a stronger determinant in treatment changes.
Symptoms, not timelines, should guide the need for CT scans for small slow brain bleeds, says the study.
These findings do not necessarily apply to victims of severe head trauma.
 Dr. Mendi has published several articles in radiology journals and has expertise in MRI, women’s imaging, musculoskeletal, neurological and body imaging.
Dr. Mendi has published several articles in radiology journals and has expertise in MRI, women’s imaging, musculoskeletal, neurological and body imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Pixel-Shot
Source: sciencedaily.com/releases/2013/01/130103113848.htm
Should I Go to ER After Hitting Head on Bathtub?
Hitting your head on a bathtub after falling can cause bleeding in the brain, but should you rush to the ER simply because you bonked your head on the bathtub?
What if you’re fully conscious and “feel fine” afterwards?
Symptoms of the brain bleed may not begin occurring until weeks after you hit your head on the bathtub!
Bathtubs are hard as hell.
I will never forget that distinctive “THUD!” at about 8:45 that morning. I immediately knew what it was and raced up the stairs and into my parents’ bedroom to get to the bathroom, calling for my mother.
She was lying on the floor, head and shoulders propped up against the side of the bathtub. I knew exactly what had happened.
She had passed out while standing and fell, dead weight, to the floor, hitting her head on the bathtub along the way.
She had very severe orthostatic hypotension and was supposed to alert me whenever she got up from a lying or seated position, so that I could prevent the falls when she passed out.
This time she didn’t alert me; I had been snoozing downstairs on the sofa.
My mother was conscious immediately after hitting her head on the bathtub (I was up there in seconds).
I helped her up and examined her head, finding no bump or blood.
My mother wasn’t 100 percent alert, though, because at first she told me she had not hit her head.
I pressed about this, and then she said she had indeed.
She also told me, after I had asked, that she did not have a headache, was not in pain.
I helped her into bed, and all I could think about was a subdural hematoma (brain bleed).
Ever since my mother developed the mysterious orthostatic hypotension, I had feared subdural hematoma from falling and hitting her head; I couldn’t be with her 24 hours a day.
Based on the sound that her head had made when it hit the bathtub, I wasn’t convinced that there wasn’t a bump somewhere on her head — and a ripe condition to trigger a brain bleed.
Check Victim’s Head; Don’t Take Their Word for It
I told her to point to exactly where she’d hit her head on the bathtub.
I pulled away at her hair and, sure enough, there was a section of matted blood on her hair.
“We’re going to the ER!” I announced. “There’s blood on her head!” I told my father.
If someone in the household hits their head on the bathtub and you find them lying on the floor fully conscious, consider taking them to the ER.
“After sustaining head trauma by hitting someone’s head against a bathtub, an urgent medical evaluation may be in order,” says Natasha Fuksina, MD, an internal and integrative medicine specialist who combines traditional and functional medicine to restore health and function.
Dr. Fuksina continues, “An elderly person on multiple medications, including blood thinners (such as Coumadin, Eliquis, Xarelto), can quickly develop a subdural hematoma (bleeding outside of the brain underneath the skull) or bleeding inside of the brain.
“If a person felt faint and dizzy and that resulted in a fall and hitting the head on the bathtub, with or without loss of consciousness, they have to be evaluated in the ER regardless of their age.”
The victim’s description of what happened or “where it hurts” may not be accurate due to compromised mentation.
The CT scan of my mother’s brain was normal, but she was held overnight for observation and a follow-up scan the next morning, which was normal.
I asked the doctor, “Is there a possibility that a few months from now, there could be bleeding in her brain from this?” He said that there was a very “slim” chance.
Six weeks later, following six weeks of normalcy as far as no neurological symptoms, my mother awakened with a blazing headache and significant lower body weakness.
I took her to the ER and sure enough, the CT scan showed a chronic subdural hematoma!
Scientific Animations, CC/BY-SA/Attribution-ShareAlike 4.0 International
Though the initial ER visit results were negative, don’t let this keep you from going to the ER a second time.
And sometimes the bleeding will be evident 24 hours later on that follow-up CT.
Age of the victim plays into this. A brain bleed is far more likely in an elderly person who hits their head on a hard surface like a bathtub from a fall.
It’s way more likely, in fact, when compared to a young adult or even middle-aged person.
“A young person or middle-aged adult will most likely not sustain any life-threatening head injuries from hitting their head on a bathtub,” says Dr. Fuksina.
“If someone develops dizziness and changes in consciousness, then prompt medical attention is still warranted.”
So regardless of age, if there are neurological symptoms, get to the ER!
If the person is elderly but shows no symptoms (nausea, worsening headache, confusion, amnesia, off-balance), get them to the ER, but don’t panic.
Remember, a bathtub is as good as concrete when hitting your head.
 Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
Dr. Fuksina is the founder of astraMDhealth, which includes telemedicine. Double board certified in internal and obesity medicine, she focuses on a personalized approach, including metabolism and genetic makeup, to customize treatments and preventive care.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Normal CT Scan After Hitting Head: Brain Bleed Can Still Occur
Can Chronic Subdural Hematoma with Symptoms Go Away on Its Own?
Slip & Fall, Hit Head Hard on Concrete: Brain Bleed Prevention
Hit Head? Bleeding in Brain Symptoms Can Occur Six Weeks Later
Really Dry Skin Around Eyes: Causes & Solutions
Dry skin around the eyes is a common problem.
It is not always corrected by simply dabbing on skin lotion or moisturizers.
“Dry skin of the eyelids is frequently referred to as blepharitis (which just means inflammation of the eyelid),” says Dr. Dendy Engelman, a board certified dermatologic surgeon with Manhattan Dermatology & Cosmetic Surgery.
Causes of Dry Skin Around the Eyes
Dr. Engelman explains, “The potential causes of blepharitis are many: allergic contact dermatitis, seborrheic dermatitis, irritant dermatitis, so treatment needs to be catered according to the cause.”
Dermatitis (contact and irritant)
• Keep track of anything that can possibly come in contact with the skin under your eyes throughout the day.
• You’d be surprised at what can end up there that you’d never think of.
• This includes household cleaning agents that are on your fingers — that get transferred to the skin beneath your eyes.
• Other possible culprits are pet dander, cosmetics, hair care products, fragrances and chemicals from the workplace.
• Once you’ve figured out what comes in contact with that area, eliminate them as best you can and see what happens.
Seborrheic Dermatitis
- This common problem involves the sebaceous glands. Not only is dry skin a symptom, but often, the skin flakes, itches and appears as a pinkish patch (sometimes with a tinge of dull orange).
- Do not scratch or rub the affected area no matter how badly it itches.
- Your doctor can prescribe an ointment to rid the problem.
Dr. Engelman continues, “Eye irritation can also be a symptom of ocular rosacea, a subtype of the disorder [rosacea] that can potentially be very serious if allowed to become severe.
“Once a medical cause has been ruled out, a nice OTC option to try to mitigate dryness around the eyes are Ocusoft lid scrubs.
“I recommend patients use these twice daily to help cleanse the delicate eye area.”
 Versed in the latest techniques and technologies, Dr. Engelman provides a wide range of services including fat removal, mole excision, Mohs surgery and skin cancer treatment.
Versed in the latest techniques and technologies, Dr. Engelman provides a wide range of services including fat removal, mole excision, Mohs surgery and skin cancer treatment.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com, bearfotos
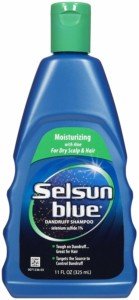
Get Rid of Seborrheic Dermatitis with Selsun Blue
Getting rid of seborrheic dermatitis is easier than you think with Selsun Blue.
Selsun Blue’s active ingredient is one percent selenium sulfide. Selsun Blue is a popular dandruff shampoo, and any similar shampoo with this active ingredient should be just as effective at treating seborrheic dermatitis.
I was diagnosed with seborrheic dermatitis some years ago. My doctor told me to just put Selsun Blue on the patches, then rinse.
I wonder how many people, who struggle with seborrheic dermatitis, have tried Selsun Blue or another shampoo with the one percent selenium sulfide. Maybe I’m an exception, but the stuff works like a charm.
I put my index finger to the bottle’s opening and tip it, getting a good gob on my finger. I then smear the shampoo on my skin, giving it a thick coat.
This is primarily on the sides of my nose, including where the nose has a crease.
It’s also on the front lower part of my nose, and sometimes on my forehead, between but above my eyebrows.
There’ve been times when the seborrheic dermatitis appeared below my eyebrows, and I dabbed the shampoo there as well.
There’s no reason to wait any length of time before rinsing. After you apply the shampoo, just rinse with water.
Any residue can be wiped away with a few Q-tip swabs held together. There’s no need to rub. Be gentle.
A wet sponge will also work on flatter areas. I’ll dab with the sponge on the front of my nose and on my forehead.
I’ll then splash water on my face. Residue is removed with the Q-tips.
I’ve noticed an improvent within 24 hours, and a complete elimination in about three days or less.
However, what typically happens is that I get lazy and stop applying the Selsun Blue.
Invariably, the seborrheic dermatitis returns. Sometimes I’ll let it go several days, but it isn’t long before I’m forced to apply the shampoo again.
If I applied the Selsun Blue every day, or maybe even every other day, this would prevent flare-ups of the seborrheic dermatitis.
But let’s face it: It’s a drudgery to have to do this every single day or even every other day.
Sometimes I forget. Sometimes I remember and just decide to skip it, because I know that when the seborrheic dermatitis flares up again, I could make it disappear within three days by just putting the shampoo on it.
The reason the active ingredient in this shampoo is so effective is because the process that leads to seborrheic dermatitis is the same process that leads to scalp itchiness and dandruff — that’s what my doctor told me.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Regional vs. General Anesthesia for Hip Fracture Surgery

If you need hip fracture surgery (or replacement), you’re better off requesting regional anesthesia rather than general.
Many people don’t know that hip surgery can be performed with only regional anesthesia, and instead automatically assume that the patient must be “completely knocked out” in order to have this procedure. Not true at all.
My father had hip replacement surgery a few years ago and it seemed that anything less than general anesthesia was out of the question.
However, a study from the Perelman School of Medicine at the University of Pennsylvania concludes that regional presents a substantial reduction in mortality as well as pulmonary complications.
Twenty percent of hip fracture patients die within one year of injury, says Mark D. Neuman, MD, assistant professor of anesthesiology and critical care, and the study’s lead author.
The paper notes how common hip fractures are: 1.6 million a year worldwide, with most occurring in people over age 65. After age 80, mortality spikes.
Regional anesthesia may include epidural, spinal or a nerve block, while general has the patient unconscious; their nervous system is considerably depressed, such that they can’t even breathe on their own and must be intubated.
In this study, the patients who had hip fracture surgery with regional anesthesia had a 29 percent lower adjusted odds for mortality when compared to general anesthesia.
As for the decrease in adjusted odds for inpatient pulmonary complications, it was 24 percent with regional vs. general.
Being that hip fracture is such a global burden, these study results are not to be ignored.
These findings “highlight an important potential opportunity to improve outcomes among a growing population of vulnerable surgical patients,” says Lee A. Fleisher, MD, chair and Robert Dunning Dripps professor of anesthesiology and critical care.
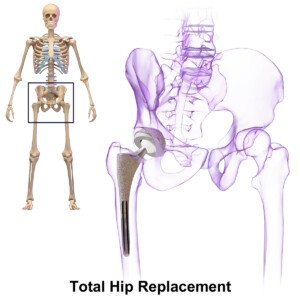
BruceBlaus
If you’re concerned about breaking your hip bone when you’re “old,” there are things you can do to dramatically lower the chances of this happening.
If you don’t lift weights, then start.

Freepik.com
Strength training will strengthen bone by forcing muscles to pull against bone to generate joint action.
This stresses the bones and makes them adapt by becoming denser. Denser bones are less likely to break.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Source: sciencedaily.com/releases/2012/06/120620100827.htm
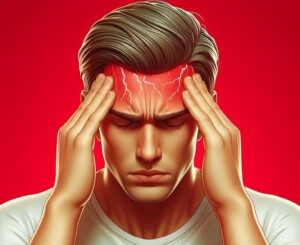
Is Physical Rehab for a Herniated Disc Supposed to Hurt?
How can a patient do physical therapy for a herniated disc if it hurts too much to exercise?
What if you have a herniated disc and find that the physical therapy exercises are impossible to do because you can’t get into the position without a lot of pain? Should you just grin and bear it?
Or does the pain mean that the exercise is actually making things worse for the disc?
First off, you certainly do not want to hastily make the decision to undergo surgery just so that you can avoid physical therapy.
People who have surgery to repair a herniated disc will still be required to stick to a physical therapy program.
And surgery is never a picnic.
How to Deal with the Pain of Physical Therapy for a Herniated Disc
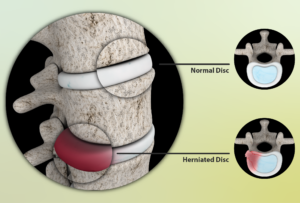
Source: myupchar. com
“Physical therapy is employed to diminish pain and suffering,” says Kenneth K. Hansraj, MD, who specializes in minimally invasive spine surgery, laminectomies and spinal fusions, and is author of the book, “Keys to an Amazing Life: Secrets of the Cervical Spine.”
“Unfortunately, especially in the phases of pain, just touching the involved spinal area may lead to further pain and tenderness.
“I encourage my clients to stay with the therapy at this point, since the therapy will lead to diminished inflammation and restoration of function along with further tolerance of therapy.”
In other words, before progress is to be felt, the patient may have to endure some inconvenience.
Pain does not always mean that something is getting injured or made worse.
In this case it would mean that the physical therapy is involving the compromised structures — and of course there will be some hurting. But stick it out; give it a chance.
In addition to the physical therapy for your disc herniation, you can implement the use of heat packs and stretching exercises to combat pain. Below are a few stretching exercises.



Freepik.com
 Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
Dr. Hansraj is an orthopedic surgeon in Poughkeepsie, NY, and is affiliated with St. Francis Hospital-Roslyn. He received his medical degree from Drexel University College of Medicine and has been in practice for 20+ years.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik/yanalya
Improve Your Blood Sugars by Tweaking Carb Intake

There are several ways to improve your blood sugar levels (glucose metabolism) by making changes to your carbohydrate intake.
You may have increased awareness of glucose metabolism in an effort to prevent type 2 diabetes or even prediabetes.
And not all type 2 diabetics are overweight, by the way — even though obesity is a major risk factor.
“People without diabetes will metabolize most any form of glucose without any problem,” begins Julie Cunningham, MPH, RD, LDN, registered dietitian and certified diabetes educator.
“As some people get older and heavier, they may develop prediabetes, which is essentially a condition in which the body has trouble metabolizing glucose quickly,” continues Cunningham.
“This can be improved by eating complex carbohydrates, such as whole grains, beans, fruits and vegetables, rather than simple carbohydrates, such as white bread, pastries, candy and sweetened beverages.
“Complex carbs are digested more slowly and create less of a spike in blood sugar levels.”
That’s your general way to help control blood sugar — whether you have diabetes or not.
But there are some more refined and clever tricks you can employ to manage and improve your blood sugar levels.
Changes You Can Make with Carbohydrate Intake to Help Improve Blood Sugar
- Limit carb servings to 60 mg or less per meal or snack.
- Eat protein with your highest carb servings, and ideally, with other carb servings such as fruit plates. E.g., deviled eggs with your dish of fruit or fig newtons.
- Don’t eat carbs close to bedtime — or at least, have only a small amount or under 20 g such as a medium apple.
- Be strategic with when you eat carbs. E.g., eat your daily apple or banana right before your step class, chest workout or treadmill run. Have another one of your daily fruit servings in the middle of a weight workout.
- At the conclusion of any workout, have another piece of fruit before your post-workout meal.
- Have your biggest carb serving of the day (pasta, rice, potatoes, etc.) within one hour of your strength training workouts.
- If you decide to indulge in a very quick-acting carb like a large glass of juice, or a helping of apple pie, a bowl of ice cream or fresh baked chocolate chip cookies, coordinate this so that it’s within one hour (ideally 30 minutes) of a strenuous workout, when glucose metabolism is most efficient.
- Space out your carb feedings. If you normally eat four servings of fruit at once, divide this into a separate four servings to be eaten once every 45-60 minutes.
- Limit juice; eat more whole fruit. Increase fiber intake.
- Replace white bread and white rice with whole grain and brown/wild/basmati, respectively.
- Limit processed foods (e.g., granola bars, some cereals, frozen dinners), which are full of quick-acting carbohydrates. Of course, for most people concerned about blood sugar, it’ll be impossible to eliminate altogether favorite processed foods. But DO make an honest effort to cut back.
How to Monitor Your Blood Sugar Levels

Shutterstock/Maya Kruchankova
To check if your glucose metabolism has improved – or at least if it’s normal — buy a home blood sugar test kit from the local drug store.
But don’t become obsessed with frequently checking your blood sugar, as this can become as obsessive as checking your body weight.
 Julie Cunningham specializes in helping men and women with diabetes and prediabetes learn how to eat to manage their blood sugars–so they can get back to the things they enjoy.
Julie Cunningham specializes in helping men and women with diabetes and prediabetes learn how to eat to manage their blood sugars–so they can get back to the things they enjoy.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lean Fit People Who Exercise Can Get Insulin Resistance

It’s alarming but true that lean fit people who exercise can develop insulin resistance.
You’ve most likely heard of insulin resistance, and it seems that every article about insulin resistance contains the words overweight, obese, lack of exercise, inactive and poor diet (or something similar).
Read enough articles on insulin resistance and you’ll soon be convinced that only overweight (especially obese) people who never exercise get this prediabetic condition.
If you’re a lean, physically fit athlete, and especially if your diet restricts processed foods, trans fats, sat fats, white sugar and high fructose corn syrup, it will be very easy to believe that you can never, ever develop insulin resistance.
The body relies upon glucose for energy—not just the energy needed to play sports or pump iron, but the energy required on the cellular level: cellular metabolism.
When you eat carbohydrates (in the form of sugar or starch), they enter the bloodstream and raise blood sugar levels. In response, the pancreas secretes the hormone insulin.
There are insulin receptor sites on the surface of cells (e.g., muscle and liver cells).
The insulin binds to these receptors, causing uptake of the glucose by the cells from the bloodstream.
The glucose will be used as energy for cellular metabolism, or stored as glycogen in the liver for later use.
But what if these insulin receptors aren’t up to this task?
This is insulin resistance, according to Dr. David Edelson, MD, board certified in internal and bariatric medicine, one of the top obesity experts in the U.S., and founder and medical director for HealthBridge.
The receptors “seem to ignore the insulin, or require higher levels before they will respond,” he says. And what if there’s a short supply of these receptor sites? That, too, is insulin resistance.
Because the cells are not taking up the glucose the way they should, the pancreas may end up pumping out even more insulin, thus stressing this gland. In the early phases of insulin resistance, says Dr. Edelson, this will result in too much insulin in the blood (hyperinsulinemia).
Over time, this can cause “fatigue, fat gain around the midsection and eventually full-blown metabolic syndrome, but in the beginning there may be no noticeable symptoms,” says Dr. Edelson.“After a while, the pancreas can’t keep up.”
The result is that blood sugar levels remain elevated. Left untreated, there is a 30 percent chance that insulin resistance will morph into type 2 diabetes. IR also raises the risk of heart disease, stroke and kidney damage.
If you’re a mean, lean and buff iron-pumping machine, and have a plant-based, mostly whole-foods organic diet, “You can still develop insulin resistance at some time in your life,” says Dr. Edelson.
However, it’s crucial to remember that remaining lean and fit through a healthful diet and rigorous exercise will substantially lower the odds of developing insulin resistance.
To learn what a lean, fit athlete or gym enthusiast with a clean diet can do to absolutely minimize the chance of getting insulin resistance, go to Part II of this article for Dr. Edelson’s recommendations.

Dr. Edelson is widely recognized as one of the nation’s top weight loss experts, and was listed in NY Magazine’s “Best Doctors of 2014” issue.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/vladee
What Can Lean, Fit People Do to Prevent Insulin Resistance?

David Edelson, MD, says that even lean, fit athletes can develop insulin resistance but there are ways to help prevent it.
First of all, examine your sleeping habits. Spiegel et al, found that “In laboratory studies of healthy young adults submitted to recurrent partial sleep restriction, marked alterations in glucose metabolism including decreased glucose tolerance and insulin sensitivity have been demonstrated.” (Journal of Applied Physiology)
If you find this shocking, the June 2010 Journal of Clinical Endocrinology and Metabolism published a report titled:
“A Single Night of Partial Sleep Deprivation Induces Insulin Resistance in Multiple Metabolic Pathways in Healthy Subjects.”
This title was the exact conclusion of the study’s authors, Donga et al.
If your fasting glucose reading is between 100 and 125 mg/dL (which in and of itself does not qualify for a diagnosis of insulin resistance, but it’s something to take notice of), or, you have been diagnosed with IR, perhaps it’s due to disrupted sleep. (A normal fasting glucose is 60-99 mg/dL.)
Insulin resistance in lean people who rigorously exercise can also result, in part, from a genetic predisposition, says Dr. Edelson.
He is board certified in internal and bariatric medicine, and one of the top obesity experts in the U.S., and founder and medical director for HealthBridge.
Dr. Edelson explains, “IR is a genetic trait that you either have or do not have.”
Insulin resistance is classically triggered by one or more lifestyle factors (e.g., a diet high in processed sugars, starches, high fructose corn syrup, trans fats, low in omega-3s, plus lack of exercise, poor sleep and excess belly fat).
But there’s more. A vitamin D3 deficiency can lead to insulin resistance.
The D3 deficiency can be caused by a number of factors, including inadequate dietary intake, lack of sunlight exposure, and inflammatory bowel disease.
Studies support the correlation between inadequate D3 and IR (e.g., Chiu et al, American Journal of Clinical Nutrition, 2004).
How a Lean, Fit Person Can Reverse and Help Prevent Insulin Resistance

Shutterstock/BLACKDAY
Dr. Edelson says that the lean, fit athlete who already has insulin resistance can take the following supplements to reverse the condition, to “more naturally turn back on the insulin receptor site so it will respond better to insulin in the bloodstream,” he says.
• Fish oil. This is a potent tool for reversing, and preventing, insulin resistance.
Suggested daily dose for mild to moderate IR: 1,500-2,500 mg. Adding wild Alaskan salmon to the diet will also help.
• Cinnamon. Though studies on humans are limited, studies on animals suggest that this spice may be a heavyweight in the reversal of insulin resistance.
Sprinkle it on fish, chicken, grass fed beef, wild game, apples, and add a touch to your protein shakes.
• Chromium picolinate (“chrome-pic”). This mineral was reported in Diabetes Education (2004) to be highly effective against IR.
The report states: “Chromium picolinate, specifically, has been shown to reduce insulin resistance and to help reduce the risk of cardiovascular disease and type 2 diabetes.
Supplements containing 200-1,000 mcg chromium as chromium picolinate a day have been found to improve blood glucose control.”
The report adds that chrome-pic supplements are safe.
What about claims that supplementation with niacin (vitamin B3) can improve glucose metabolism?
Dr. Edelson explains, “There has been some concern that niacin may actually worsen IR. It has long been known that niacin can raise fasting glucose levels.
“Recent articles seem to indicate that this effect is due to niacin provoking IR.
“As such it is even possible that niacin supplementation in food items such as breakfast cereals may actually be worsening the obesity crisis.
“A recent article in the World Journal of Gastroenterology points to this effect.”
Additionally, there are other measures that the trim athletic individual with insulin resistance can take.
According to Kristine Gedroic, MD, who specializes in integrative medicine in Morristown, NJ, diet should be re-evaluated, even though the patient may think he or she has a very healthful regimen.
“Many complex carbohydrates are less than ideal,” says Dr. Gedroic.
“For those with true IR, I advise only carbohydrates that are cooked in a pan or from nature, i.e., steel cut oats, brown rice, quinoa, millet and potatoes.
“No flour products of any kind until the insulin resistance reverses.
“Sugar substitutes must also be removed from the diet (though Stevia, which is natural, is acceptable), along with chewing gum, which can activate digestive function artificially.
“After those basic interventions are made, this type of patient often needs a comprehensive endocrine assessment.
“Many times when the pancreas has been stressed producing insulin for whatever reason, the liver, adrenals and possibly thyroid gland may be suboptimal too.”
The key is prevention of insulin resistance, and lean, physically fit people who believe they have a clean diet are not exempt from being aware of this prediabetic condition.

Dr. Edelson is widely recognized as one of the nation’s top weight loss experts, and was listed in NY Magazine’s “Best Doctors of 2014” issue.
 Dr. Gedroic is founder of the Gedroic Medical Institute, which has successfully restored health to thousands of patients with nearly every chronic condition.
Dr. Gedroic is founder of the Gedroic Medical Institute, which has successfully restored health to thousands of patients with nearly every chronic condition.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/FXQuadro
Burn Fat with the Squat to Lunge Workout!
Here are easy instructions for the squat to lunge workout which will burn fat off your thighs, belly and all over your body. Video follows.
The squat to lunge workout is exactly what the name says: squat, then go into a lunge.
This can be done from end to end in an empty basketball court, or from end to end in an empty fitness class studio, or from one point to another on the gym floor.
Use a fixed weight barbell, as these are smaller than Olympic bars and less cumbersome.
This routine is not for beginners or people who are not proficient with the back squat form.
Stand with feet at least shoulder width apart or whatever your preferred stance is for the back squat. To start the exercise, perform a half squat.
After rising to the start position, step forward with one foot into a lunge stance, perform a lunge, rise, then bring the back foot up to flush with the forward foot.
Next, step forward with the other foot now, into a lunge, lower accordingly, rise, and then bring that foot flush — except instead of the feet being close together like they typically are after completing each lunge during walking lunges, after that second foot completes the sequence, it comes up to create the foot-to-foot distance that you’d use for the back squat. At this point, you squat.
Summary: Then the cycle begins all over. So it’s as follows:
· Squat
· Return to start position
· Lunge with right foot
· Bring left foot to flush with right foot
· Lunge with left foot
· Bring right foot flush but at least shoulder width from left foot
· Squat
Ideally, a person should be able to execute smooth movement so that motion is fluid rather than robotic with the lunge portion.
Once you can execute the sequence with confidence, it’s time to get a barbell across the upper back.
How much the barbell should weigh is not something you’ll likely be able to figure out on the first try.
Let’s suppose someone starts with a 50 pound barbell. This may seem light to an individual who squats reps with 185. But the walking lunge really changes things.
Furthermore, one must get used to walking lunges with a barbell across their back; many who do walking lunges with weights use only dumbbells held with straight arms at the sides.
With the barbell, execute the aforementioned sequence. Don’t be surprised if you become fatigued very quickly. Intense fatigue is important for burning fat.
Squats should be at least parallel (half squat), and lunges should be deep. The more it “hurts,” the more fat you’ll burn.
Make sure you don’t “good morning” the squatting portions; keep good form and an upright back.
Burn More Fat by Increasing Intensity
Use a heavier barbell as you get better at this exercise. You should be able to sustain this movement for at least one minute before having to stop.
Longer than two minutes means that the emphasis is shifted towards endurance.
Another way to increase intensity is to perform the squat after every single stride.
And yet a third intensity technique is to perform this fat burning routine backwards.
It’s best to do the backwards version in a fitness studio so you can watch in a mirror.
Do this routine twice a week to increase your body’s ability to burn fat.
Remember, staying in your comfort zone will not burn fat. This exercise will promote fat burning through the entire body.