WHY Kids Are Scared of the Dentist; Solutions for Parents

Knowing why children are afraid of the dentist will really help you correct this problem.
“In my opinion, I believe that kids are very much influenced by their parents,” says Cyndi Blalock, DDS, owner of Cardinal Dental in St. Peters, MO.
“If their parents are afraid of the dentist, most likely the child will grow up with similar fear,” continues Dr. Blalock.
It’s simple: Children internalize their parents’ anxieties. And there are adults out there who are scared out of their wits of the dentist. This is evident in online forums. Also, why do you think there’s a such thing as “sedation dentistry”?
Dr. Blalock explains, “There have been many times that I have had a parent in the room and they themselves were so nervous that they began making scary comments about what I was doing.
“Or I told the parent that the child has a cavity, and their immediate response was, “Well, you’re getting a shot in the mouth.”
While that may be the truth, I have ways that I can numb a pediatric patient without them ever know that a shot was used to do it!
“But if the parent tells them they’re getting a shot, its an uphill battle for me to try to will over a child and convince them that I’m not going to hurt them. After all, mom said this is going to hurt!”
Parents need to choose their words carefully and not think that this is coddling their child or will make their child a wimp.
Words are powerful. If you think that kids are just overly sensitive, imagine how you’d feel (assuming you’re a woman), if your husband or mother one day said, “That dress makes you look fat.” Words…
Dr. Blalock says, “Sometimes if a child has had a previous bad medical experience such as an illness resulting in hospitalization, surgery or injury, he or she will have a harder time not being fearful of the dentist. The fear of the unknown can also contribute to it.”
Don’t act nervous even about your own upcoming dental treatment.
If your child hears you expressing your own fears about an upcoming dental appointment, don’t be surprised if this leaves an unshakeable impression.
Even if you say nothing, your child will see your body language as you sit in the waiting room, fidgeting, looking unnerved.
Though this article is mainly about why children can develop a fear of the dentist, it’s also important to hear what Dr. Blalock advises to resolve or prevent this problem.
She explains, “Encourage your child to not be fearful of the dentist. Instead of instilling fear of the dentist into your child, instill trust in them.
Most dentists really do not enjoy hurting people, contrary to how we are portrayed in the movies and in the media. Never use the word ‘shot’ to your child.”
Here are more words to avoid using: drill, scrape, poke, dig and needle. Friendlier words are: polish, make sparkle, instrument and check things out.
 The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Vitali Michkou
Can Wisdom Teeth Removal Cause Nerve Damage?

A dentist says that nerve damage can be caused by the removal of wisdom teeth.
Here is what Cyndi Blalock, DDS, explains: “Yes, it can, if the patient is built with a inferior alveolar nerve running close to the impacted wisdom tooth.”
Dr. Blalock is the owner of Cardinal Dental in St. Peters, MO.
She continues, “While this is a rare situation, it is a known complication.
“I don’t remove impacted wisdom teeth, but I do counsel my patients on the possibility of nerve damage if it appears that the roots of the wisdom teeth are close to the nerve canal.”
Nerve Damage from Wisdom Teeth Removal
Nerve damage from wisdom teeth removal can manifest as tingling or numbness in the affected area.
While such symptoms may be temporary and resolve as healing progresses, there is a risk of permanent nerve damage in some cases.
In addition to the inferior alveolar nerve, another nerve might sustain damage: the trigeminal nerve, which is one of the 12 cranial nerves — the fifth one.
In this case, the tongue would be affected – with pain, tingling or numbness.
These sensations may also involve the teeth, gums, lower lip and even the chin.
The trigeminal nerve is a major facial nerve. It has three main branches: the ophthalmic, maxillary and mandibular nerves.
These branches provide sensory information from the forehead, upper jaw and lower jaw, respectively.
The trigeminal nerve also controls muscles involved in chewing.
However, the damage from a wisdom tooth extraction is usually temporary, though this can go on for up to a few months. In rare cases of severe damage it’s permanent.
A nerve injury from root canal removal (involving either the inferior alveolar or trigeminal nerve) would cause symptoms of only sensation rather than function.
There would not be any weakness in the muscles of your tongue and lip.
Before you decide to forego having your impacted wisdom teeth removed due to fear of a nerve injury (which, remember, is usually temporary), remind yourself that making this decision could result in worse problems.
• Partially grown-in wisdom teeth that are not extracted can cause a bacterial infection.
When these teeth do not fully erupt or are only partially emerged, they create an environment where bacteria can accumulate around the gum line.
This condition, known as pericoronitis, can cause pain, swelling, and infection of the surrounding tissues. If left untreated, the infection can potentially spread and lead to more serious complications.
• Teeth that have remained non-erupted can cause a cyst – which can damage gum and bone.
These cysts, known as odontogenic cysts, form in the jawbone or surrounding gum tissue and can cause damage to both the gum and bone.
As the cyst grows, it can erode surrounding bone structures, potentially leading to pain, swelling, and further complications.
• If the teeth grow in, but are crooked, this can impair bite alignment, leading to jaw pain.
Bottom line: If your dentist advises you to have your wisdom teeth removed, have this done.
 The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/FotoDuets
Brushing Teeth: Cold vs. Warm Water

How often do you brush your teeth and wonder if it really makes a difference whether the water is cold or warm, as far as the ability to clean your teeth?
Of course, cold water is uncomfortable to the nerve endings for many people, and for that reason alone, many will not brush with cold water.
However, they will brush their teeth with non-cold water — meaning, it’s not necessarily warm, let alone warm-hot.
Others swear by a temperature that’s closer to hot (but not hot enough to be uncomfortable) — perhaps something more like very warm.
It can be quite comfortable for some individuals, but that question remains:
Does temperature of the water really matter as far as the efficacy of getting your teeth clean?
“If your teeth are hypersensitive, brushing with lukewarm water may be best,” says says Cyndi Blalock, DDS, owner of Cardinal Dental in St. Peters, MO.
“Sometimes very cold or very hot can irritate sensitive teeth, so I would recommend using a temperature somewhere in the middle,” continues Dr. Blalock.
“Do not go to extremes with temperature; brushing shouldn’t be a painful experience.
“If it is, seeking the care of a dental professional would be a good idea, as there may be more dental issues going on.”
 The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
The health of Dr. Blalock’s patients is a top priority at Cardinal Dental. She provides a comfortable and caring environment where she can effectively customize a dental plan to suit the needs of you and your family.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Benign Differential Diagnosis for a Winged Scapula

You may have what looks like a winged scapula, but it may be something else that’s benign.
In my case, the diagnosis was “functional weakness of the parascapular muscles.”
The name is odd in that I had no weakness. I had no limitations in range of motion, no stiffness, aching or pain.
I lift hard and heavy at the gym, so any weakness or deficit would have been easily noticed.
One day I noticed what looked like a winged scapula upon viewing my shirtless back in a mirror.
However, I did not see any pronounced appearance of the scapula upon doing the three classic tests for a winging scapula: 1) wall pushup, 2) shoulder abduction and 3) shoulder flexion.
The doctor I saw, a non-surgical sports medicine specialist, had me do these three things too (I had by then already done them numerous times). Oddly, he used the word “subtle” more than once to refer to my condition.
He said I could keep doing what I’m doing at the gym (I told him exactly what I do), but suggested physical therapy and gave me the number for that. I made an appointment after I got home.
Nevertheless, the doctor does not expect this situation to become a performance problem; it’s a cosmetic problem, if anything.
Functional weakness of the parascapular muscles means that for some reason, those muscles are being activated differently than the ones on the other side.
The doctor also pointed out that on many of his other patients, the disparity (pseudo-winging) would not even be noticeable, due to higher levels of body fat in those patients.
But I told him my weight was the same two months prior, when I did not have this condition (which I would have easily noticed back then if I did have it then, when I was viewing my bare back during a self-skin exam).
Nothing had happened to me between then and this doctor visit; no injury, fall or collision involving my shoulder or back.
Things just somehow got a little off-kilter or out of balance. The doctor said there is no damage to the thoracic nerve, tendons or muscles. The X-rays were normal. “Everything looks pretty darned good,” he told me.
Don’t be alarmed that you might have something sinister going on with your “winged” scapula just because you fail the three tests for the condition.
There are some alarming conditions out there that involve lumps on the scapula, such as chondrosarcoma — but I do not know if this cancer would make the scapula appear to wing. Furthermore, chondrosarcoma is exceedingly super rare!
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Source: ajronline.org/doi/pdf/10.2214/ajr.124.1.113
Scariest Top 4 Benign Medical Symptoms

Sometimes the most frightening body symptoms are actually very benign conditions.
So what are the four scariest medical symptoms that are benign or usually benign?
TWITCHING MUSCLES. Another name for twitching muscles is fasciculations.
Benign fasciculation syndrome (BFS) describes a harmless condition characterized chiefly by “twitching” muscles, but often accompanied by muscle cramps and fatigue, and sometimes tingling sensations (which can actually be from anxiety over the condition).
A person can experience only the twitching, and it can persist harmlessly for years.
“Muscles may randomly twitch for many reasons,” points out Carolyn Dean, MD, ND, and medical advisory board member for the Nutritional Magnesium Association (nutritionalmagnesium.org).
She adds, “They can twitch due to anxiety or stress, a sleepless night, too much coffee or after exercise.”
Why is this benign symptom scary? The benign muscle twitching becomes annoying enough for one to search about it online.
Search results bring up information about ALS, an always-fatal neurodegenerative disease; sites (such as alsa.org and mayoclinic.org) list muscle twitching as a symptom.
Some folks with benign twitching muscles may also fear they have multiple sclerosis or Parkinson’s disease–which actually can cause tremoring and trembling.
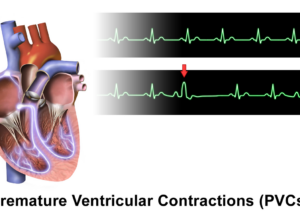
PVCs. The dreadful premature ventricular contraction (sometimes called premature ventricular complex) makes many people think a heart attack is about to happen.

Freepik.com
PVCs are difficult to ignore and feel very abnormal. Descriptions of PVCs vary somewhat, including “flip flopping” of the heart, skipped beats, extra beats, pounding beats, heart going through chest, fluttering and thumping.
Why is this largely benign condition scary? If you’ve never had a PVC, you wouldn’t really know.
Anyone who’s had reams of PVCs will tell you it’s downright frightening, at least prior to being told by their cardiologist that their heart is healthy. Imagine feeling your heart “jumping around” in your chest.
Though it’s strongly advised that anyone with a “flip flopping” heartbeat should be examined by a cardiologist, this doesn’t mean that PVCs are harbingers of heart attacks.
It simply means that a cardiac evaluation is fully capable of ruling out an abnormality, and this should reassure the patient.
“PVCs are not considered a precursor to heart attack,” says David N. Smith, MD, a board certified cardiologist with Premier Cardiovascular Care and Wellness in SC.
However, another cardiologist states: “Three or more PVCs in a row are defined as non-sustained ventricular tachycardia, and an evaluation for underlying disease is mandatory when they occur,” says Norman E. Lepor, MD, cardiologist and internal medicine specialist Norman E. Lepor, MD, who’s with Cedars Sinai in Beverly Hills, CA.
BEETURIA. This will freak anyone out if they don’t quickly connect some dots. The first time this happened to me, my first thought was, “Did I recently eat something bright red? Yes! I had beet juice!”

Freepik.com
Beeturia is when undigested beet juice appears in the urine, coloring it red, pink or orange—making one think they have blood in their urine. How scary is that?
“Stool beeturia” is when there’s red in one’s bowel movements. This was my first experience with undigested beet juice.
The crimson pigment in beets is called betain, and a small percentage of people do not digest this fully. The condition is benign.
Why is this benign situation scary? People think they have blood in their urine or stools. Blood in the urine or stools can mean serious diseases, including non-malignant but serious conditions.
Undigested beet pigment in the toilet bowl is especially frightening to men because they’re typically not used to how blood looks in the toilet bowl, whereas menstruating women know exactly what this looks like.
However, women not familiar with beeturia will find this alarming until they realize it’s just beet pigment. Read here to learn how to tell the difference between beet pigment and blood in your stools.
SLEEP PARALYSIS. Many people are terrified by this. You awaken and literally can’t move. You try to move any part of your body, but can’t. You are paralyzed.

Shutterstock/Africa Studio
However, sleep paralysis is benign. However, many men and women fear this every time they go to bed, and no matter how often it happens, they never get used to it. Sleep paralysis may last a few minutes but is benign.
Why is this scary? Well heck, you can’t move. People think they’re dying or have nerve damage. They have no control. They can’t even speak. Sometimes sleep paralysis is accompanied by hallucinations.
They must wait to spontaneously pop out of it. There are two popular explanations for the benign phenomenon of sleep paralysis.
Protects sleeper from physically acting out a dream.
This mechanism is off-kilter in sleep paralysis. Normally, muscles are “paralyzed” by a protective mechanism while you dream.
So if you’re dreaming you’re a boxer, this mechanism prevents you from punching the wall and breaking your fingers.
The mechanism is supposed to turn off before you awaken. If it’s delayed, you’ll be aware of the paralysis. Isn’t that fascinating? And the hallucinations reflect the delayed exit from a dream state.
Return from an out-of-body experience.
Paranormal enthusiasts note that when an individual remembers dreaming right before they experience sleep paralysis, this means that the “dream” was actually an out-of-body experience, which is why the “dream” is typically lucid—in which the individual is flying—not in an aircraft, but via their body.
The paranormal community also believes that sleep paralysis is a launching pad to out-of-body travel; it’s a sign that your astral body is preparing to exit the physical body.
There are a number of other very scary but benign or usually benign medical symptoms, but these top four surely are right out there as causing a lot of anxiety and “freaking out.”
But I must say this: Of these four frightening symptoms, only TWO of them are benign 100 percent of the time: sleep paralysis and beeturia.
This means that muscle twitching CAN be a sign of a neurological disease or Lyme disease (but it usually isn’t).
And what you think are harmelss PVCs can actually be a heart rhythm disorder that requires treatment.

Dr. Smith is a published author, national lecturer and Yale-trained physician-scientist certified by the American Board of Internal Medicine in Cardiovascular Disease.

Having performed over 4,000 coronary angiograms and angioplasties, Dr. Lepor has focused on prevention and treatment of coronary heart disease.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/ PORTRAIT IMAGES ASIA BY NONWARIT
Sources:
webmd.com/sleep-disorders/guide/sleep-paralysis
iacworld.org/english/research/sleep-paralysis-and-its-causes
Can Bodybuilding Ever Be Unhealthy?
No matter how big your muscles get, you will not become unhealthy as a result.
If you actually think huge muscles are unhealthy, then ask yourself why, when you’re at the busy medical clinic for a routine checkup, you don’t see one bodybuilder after another standing in the long check-in line or anywhere in the building.
And of course, this assumes that the very muscled person is NOT taking performance enhancing drugs.
There will always be those who believe “That’s not healthy” when referring to a photo of a bodybuilder on stage.
This isn’t about the dangers of steroids. It’s about muscles—“lots of” muscles, and whether or not that’s unhealthy.
Ironically, but not surprisingly, the people who think that advanced muscle development is not healthy tend to have low levels of muscle development, and in fact, often don’t even work out.
At least that’s the case with all of the people I’ve ever heard throughout my life say that a very muscular body isn’t healthy.
What about stiff joints from all the bulk?
It’s a myth that bodybuilders have stiff muscles and joints. Though the typical male physique athlete can’t drop into the splits, neither can the average man off the street.
Having a lot of muscle has not been linked to an increased risk of any kind of disease, nor has it been associated with an increased risk of falls.
Bodybuilders train their legs and hence, have strong knees and dense bones — and this protects against easily-fractured bones from falls or other accidents.
“It’s not healthy to be like that” sounds more like an attempt by the average Joe or Jane to justify why they’re so out of shape.
They may perceive the V taper as unnatural and harmful, because it’s inconceivable to them how someone could have such a tiny tight waist yet looming shoulders.
Furthermore, bodybuilders and physique athletes tend to have far healthier diets than do average people. So where this “unhealthy” label originates is nothing short of baffling.
Bodybuilders typically stay away from heavily processed foods.
Their sources of protein are usually grilled chicken and fish, tuna salad and sometimes various cuts of steak—all in whole form rather than in boxes full of synthetic additives and added sugars.

They do enjoy eggs and eat plenty of steamed vegetables, brown rice, yams and boiled potatoes.
If they eat bread, it’s often whole grain rather than white (though many bodybuilders avoid bread altogether).
Breakfast for the bodybuilder is typically a vegetable omelet, sometimes with just egg whites, plus oatmeal with berries—you get the picture, whereas the typical American breakfast is anything from pancakes, sausage and English muffins slathered in sugary jams, to cereals full of artificial colors and lots of added sugar. Not to mention the pastries.
As a former personal trainer for a large health club, I was inspired to write this article after a man told me, “It’s not healthy to be like that,” when I showed him a photo of male bodybuilders on stage.
Needless to say, this man, a coworker of mine at the time I was working in an office, ate multiple bags of various munchies throughout every single day, and drank a lot of soda.
I don’t know about you, but I’d rather have a bodybuilder’s physique and diet than live on the junk that this man did. I might also mention that he had a big belly and rather scrawny arms and legs.
Which body below is healthier? I know which man I’d rather have find me if I were buried under rubble from an earthquake.

I can easily picture the man on the right quickly becoming exhausted after shoveling snow, risking throwing out his back, and awakening the next day sore from head to toe.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ALL best fitness is HERE
What Makes You Poop Right Before Doctor Appointments?

Ever notice that minutes before a doctor’s appointment, you feel a bowel movement coming, regardless of time of day?
I’ve noticed this. Whether the doctor appointment is in the morning, around noon or later in the afternoon, seems that 20 minutes or less before the appointment time, I have to have a bowel movement.
I then find myself under the stress of hurrying to void everything and get super cleaned up and back in the waiting room before the nurse calls my name.
What is it about a doctor appointment that makes some people prone to having to make a poop so close to the appointment time, whether morning or afternoon?
This is not related to eating habits prior to leaving the house. In fact, for early morning appointments, there won’t even be that much in my stomach.
I also don’t have a bowel movement every day; my normal is to skip a day or even two days. But this skip never happens on a doctor appointment day.
The Explanation in Layman’s Terms
Your body doesn’t know the difference between the fear of coming face to face with a wolly mammoth in the wilderness and the fear while waiting for your gynecological or prostate exam.
The body prepares to fight the perceived threat, or run from it. Either way, your body wants to get rid of any excess baggage so that the fight or escape can be carried out as efficiently as possible.
One way to rid excess baggage is to create enough nausea to force a person to vomit.
This is why some people upchuck when suddenly confronted with a very unsettling or gross situation.
Clearing out the stomach through the mouth lightens things up a bit (although marginally), but remember, in the face of a perceived danger, the body does all it can to optimize the fight or escape.
If your large colon just happens to contain poop during the body’s fight or flee response, it’ll want to dump that excess baggage as well.
Anyone who works out at a gym or runs for exercise knows that carrying around poop can kind of make things feel like a drag.
This is why fitness enthusiasts and athletes hope to “dump a load” prior to a workout or game.
Likewise, a fight or escape from danger is optimized if the bowel movement is expedited via the stress hormones.
The Same Explanation in Doctor’s Terms
“It’s fairly well-known that stress can increase the frequency of bowel movements,” says Dr. David Beatty, MD, a retired general practitioner with 30+ years of experience and an instructor of general medicine for 20+ years.
Anxiety or stress won’t create more poop, though. But it’ll alter frequency for your usual amount of poop.
“The vast majority of people would regard going to see the doctor as anxiety provoking,” continues Dr. Beatty. “I absolutely hate being on the receiving end of medical care.
“When we are under stress our body pumps out a cocktail of hormones.
“These are adrenaline, noradrenaline, cortisol, glucagon and growth hormone.
“The last three don’t have any effect on defecation that I’m aware of.
“Adrenaline and noradrenaline trigger the sympathetic nervous system, which prepares the body to fight or run.
“Heart rate increases and blood is pumped to the skeletal muscles and away from the digestive tract.
“Stimulating one of the sympathetic nerves relaxes the internal anal sphincter.
“This implies higher adrenaline and noradrenaline levels would relax the anal sphincter and thereby increase the urge to go to the toilet.”
 Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
Dr. Beatty has worked in primary medicine, surgery, accident and emergency, OBGYN, pediatrics and chronic disease management. He is the Doctor of Medicine for Strong Home Gym.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com senivpetro
Why Older Women Shouldn’t Use Walking Sticks when Fitness Walking

The use of walking sticks, including among older women, seems like more of a fad or gimmick than an orthopedic necessity.
As a former personal trainer, I’m opposed to the use of walking sticks (hiking poles) by an otherwise able-bodied person, including older women.
First off, use of the sticks (touching them to the ground when walking) will not burn more calories than if you didn’t have them.
Maximum calorie burn comes from the largest muscles of the body doing all the work.
If you use the poles to momentarily support yourself with each stride, this subtracts work from the legs, which have the largest muscle groups.
The only way the walking sticks would burn more calories is if you didn’t let them touch the ground.
That’s because you’d then be carrying the hiking poles in a way that would not give support to your walking.
Besides, not all older women who use walking poles are trying to lose weight, so the weight loss issue isn’t all that relevant.
I have to believe that the “everyone else does it” mentality plays a role in the use of walking sticks.
Many older women use these devices when walking on even, stable terrain. I’ve seen people using these on smooth asphalt park trails.
So this isn’t about needing a stick to prevent falling down a steep scree slope.
So many people use walking sticks that I’m also not willing to assume that all of these people (including young ones) have “bad knees.”

Freepik.com
To improve fitness and mobility, and develop more efficient joints and a more efficient core, you must leave the walking sticks at home.
If you’re an able-bodied woman of mature age, ask yourself if you’ve become psychologically dependent on your walking poles.
Example of the Body’s Ability to Adapt
Years ago when I first began hiking steep hills, I noticed that going down on one side (I’d lead with one leg, facing 45 degrees away from the slope—a safe way to descend) was trickier than the other side.
I wanted to use the “good” side more. I didn’t have hiking sticks.
But I realized that in order to get the tricky side to match the good side, I’d have to spend more time descending on the tricky side.
My leg just didn’t feel as strong or as coordinated as the other when I was descending on the more efficient side.
Next week, same slope, I noticed that the “weak” side was improved. It took only one session, stick-free, to create a training effect, an adaptation to the challenging stimulus. Again, I used the weak side more.
The third time, a week later, the “weak” side was almost as efficient as the other side. After that point, on all subsequent hikes, both sides of my body were equally proficient.
Had I relied upon walking sticks…forget it; I would have descended alright, but would NOT have sparked more efficient neurological factors.
Walking sticks will rob the older woman of the chance to improve her neuromuscular function, her coordination and balance.
If you think you’ll fall without the poles for support, then take on an easier trail. But I must emphasize:
People use these sticks on level, smooth asphalt. The element of fad is at work here.
The best way for an older woman to fitness walk is to pump her arms and move briskly or as briskly as she can.
You will feel empowered without the walking sticks, which remove workload from your core.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Depositphotos.com
Double Kettlebell Swings for the Shoulders for Men and Women

It’s time to make room for the double for unique benefits for both men and women of any size and fitness level.
For a warmup, cool-down or a full-out working routine, you should consider doing double kettlebell swings for the shoulders.
For those who’ve never done these but have observed people doing them, different interpretations may come to mind.
For instance, is the kettlebell swing a back exercise? Is it chiefly a lower body workout? Or if the kettlebell is heavy enough, can it be considered a shoulder workout (frontal raise)?
The kettlebell swing is a compound exercise, hitting several muscle groups at the same time: shoulders, middle back, core (lower back and abs), glutes, quads and hamstrings.
There are also variations of this movement, but a not so common variation is that of the double kettlebell swing.
Kettlebell Swing Basics
To make this exercise recruit more shoulder muscle, you should use a weight that’s heavier than what’s typically used in the kettlebell swing.
Often, just one kettlebell is used, with both hands on the handle.
Usually, women use a 5 or 10 pound bell (2 and 4 kg, respectively), and men use up to 20 pounds (9 kg), when focused on simply doing this movement the way it’s been taught.
The traditional way is to stand with feet more than shoulder-width apart, toes pointed out a bit, arms hanging straight in front holding the bell.
With a soft knee bend, you swing the bell upward to shoulder level, then “unswing” it, letting gravity do most of the work. The back remains upright for the most part, and an arch in the lower back is maintained.
The KB slightly breaks the plane created by the legs, but doesn’t actually go through the legs.
However, a variation is to let the kettlebell travel right through the legs, in which case you must bend at the trunk. This variation recruits even more of the lower back.
In these above examples, the legs go into a small or “quarter” squat. They can go deeper, but it’s not necessary.
But another variation is to add a half-squat, with your thighs parallel to the floor. It’s important to keep an arch in your lower back at all times.
A half-squat will recruit more of the glutes and legs. The constant in any variation is that the shoulders are moving, and the frontal or anterior deltoid is the main shoulder muscle at work.
How to Make the Kettlebell Swing More Shoulder Dominant
The first way is to double up on the kettlebells. The start position is with both arms hanging in front, each holding a bell, and the lower part of the forearms are crossed over each other.
Raise the arms outward, forming a V, as in a hybrid of a frontal raise and lateral raise.
Bring the weights up to at least shoulder height, even a bit higher.
Using both arms in this trajectory right off the bat targets more shoulder muscle fiber (front and middle deltoids).
NOTE: The KBs are swung up, not lifted per se. Keep arms as straight as possible, just short of an elbow lockout.
How much weight should each kettlebell be?
The total weight should be heavy enough to allow you to perform between eight and 12 repetitions without any breaks in form.
If you must go up on your toes to get the weight up, or find that you’re bending your arms too much, then the total weight is too heavy.
So if you’re using a total of 50 pounds, try a 20-pounder in each hand.
Many gyms carry kettlebells up to 35 pounds (15 kg). The heavier the weight, the more muscle that gets built. Many people seem to think that “kettlebell exercises” mean only light bells.
Imagine how the deltoids will grow when one performs the double kettlebell swings for the shoulders with bells so heavy, that only 8-12 reps can be performed (always maintaining good form).
The Swinging
There are two ways to look at this. The first way is to swing the weight up and down with the classic, gravity-based momentum that’s used in the single-bell swing. The momentum is fueled by the hips and legs.
But the second way is to slow the swing down a little, so that you’re adding a lift to it going up, and a release to it going down.
This will recruit more shoulder muscle, and this technique is also more difficult when compared to the classic swinging for the same amount of weight.
You may also want to see how the double swinging goes with the arms separated. Either technique will yield benefits. And yet another variation is to alternate the arms. See what works best for you.
Stances
- Sumo stance. This is a very wide stance with feet pointed out. Do not point feet straight ahead, as this will cause the knee joint to inadequately track over the foot. Add a slight or half squat upon lowering the kettlebells.
- Regular stance. Assume whatever width you normally use when you do squats. If you don’t do squats, assume a width of at least shoulder or a bit more. Lower to a partial or half squat upon releasing the kettlebells. Try to keep back as erect as possible, though a forward lean is fine as long as there’s a continuous arch in the lower back; never round the lower back.
- Any stance, lowering weights through the legs. At the bottom of the movement, drive the kettlebells (with forearms crossed, since this is at the bottom of the repetition) through the legs. Try not to round the back because you will need to lean forward to do this.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/RomarioIen
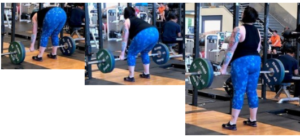
Weight Training for Plus Size Women Over 50

Training with weights will provide remarkable results for women over 50 who are plus sized.
Overweight women 50+ can just as easily pick up a dumbbell or barbell as thinner women in this age group.
There are many benefits from strength training for plus size women over 50. Every woman needs to lift weights — ESPECIALLY older ones.
“Weight training” is the PC term that refers to, quite simply, lifting weights. Call it what you wish, but it’s the same thing: moving against resistance.
This can be done with any of the following:
- Dumbbell and barbell
- Kettlebell
- Resistance machine
- Heavy medicine ball
- Tension band/tubing
- Suspension straps
- Body weight only (e.g., pushup)
Though plus size women over 50 years of age will struggle with pushups if they’re not trained…realize this: You do NOT have to try pushups.
However, body weight squats are a superb start that you can actually do on the very first try. The issue is how many you can do in a row. Aim for 8, then 12, then 15, then 20.
Strength Training Benefits for Overweight Women 50 Years or Older

Leg press. Shutterstock/Aleksey Boyko
Though a woman should begin lifting weights much earlier in life, it is never too late to reap the great rewards of exercising against resistance.
Though many women today continue to be averse to the idea of picking up a dumbbell, barbell or even pushing against a stack of metal plates on a sit-down machine, it is women, more so than men, who really need to push and pull against resistance.
This is because women are at a much greater risk of suffering from brittle bone disease (osteoporosis) than are men.
The hormone estrogen has a protective effect against bone loss.
The level of estrogen in a woman’s body drops significantly after menopause, and this heightens her individual risk for losing bone mass.
One way to preserve bone mass is to lift weights. Strength training makes muscles pull at bones.
When muscles pull against bones, this forces the bones to adapt to this stimulus. They adapt by increasing in density (i.e., mass).
Hence, greater bone mass results from weight workouts. The more bone mass a woman has, the less likely she’ll ever suffer a bone fracture.
A second benefit is that strength training will encourage fat loss.
Beginning at around age 30, a woman who has not been weight training begins to lose muscle mass, to the tune of about 5 pounds of muscle per decade.
By the time she’s 50, she’s lost up to 10 pounds of muscle.
Resistance exercise can replace this loss of valuable tissue. Loss of muscle is directly correlated to gain in fat.
In fact, it outright causes fat gain, because muscle requires a lot of energy (calories) just to exist.
If a woman loses muscle, incoming calories get stored as fat because there’s no longer enough muscle mass to use up all those incoming calories.
Does weight training for plus size women over 50 differ from that for trainees much younger?
No, not at all. The same rules apply:
• Warm up
• Practice good form at all times.
• Do mostly compound routines. Compound exercises work several muscle groups at once (examples follow).
• Don’t work the same muscle groups two days in a row.
• Separate weight days from cardio days.
• Lift moderate to heavy weights (whatever feels “moderate” or “heavy” to the trainee).
• Sessions should last 30-60 minutes.
• After warming up, you should do sets with enough resistance to make 8-15 repetitions very challenging.
If the trainee wishes to push even harder (by either using more resistance or by pushing through to the last repetition that’s absolutely possible), that’s great, too.
Some people have more of an “iron will” than others and enjoy pushing to exhaustion. One should not push to exhaustion on every set, however.
• Beginners should spend several weeks using light weights and working at an effort of moderate intensity before advancing to higher intensity.
• Practice progressive overload. This means gradually increase the resistance over time as the muscles and joints get stronger.
• Exhale on the exertion (the push or pull) and deeply inhale on the release. Never hold the breath during a routine.

Squat. Shutterstock/Reshetnikov_art
Best compound exercises for building bone, losing fat, toning and strengthening muscles and becoming as physically fit as possible:
• Deadlift (barbell or dumbbell). Works middle and upper back, shoulders, arms, legs, buttocks and core (lower back and abs).
• Squat (barbell, dumbbell, kettlebell). Works legs, buttocks and core; works shoulders when dumbbells and kettlebells are used.
• Leg press. Works buttocks and legs.
• Lat pull-down/seated row/barbell row. Works back and arms.

• Bench press/dumbbell press/pushup. Works chest, shoulders and arms.
• Shoulder barbell/dumbbell press. Works shoulders and arms.
• Clean & press. Works middle and upper back, legs, buttocks, core, shoulders and arms.
Best isolation exercises. Isolation routines utilize one main muscle group and require action from only one joint. These burn much less fat than do compound exercises.
- Biceps curls with barbell or dumbbell
- Triceps push-downs with a rope and pulley system
- Chest flyes with a “pec deck” machine
- Shoulder side and front raises with dumbbells
- Leg extensions
- Hamstring curls
Being overweight is sometimes used as an excuse to avoid lifting weights.
However, it’s time to see being full-figured as a reason to embrace working out with weights.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.