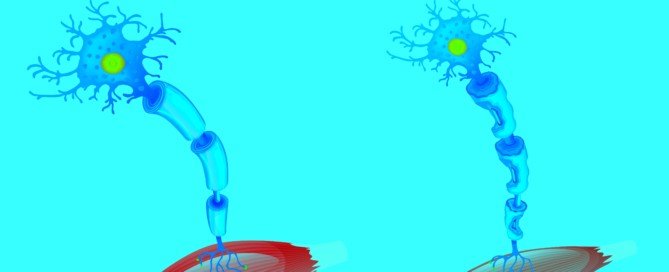
ALS Weakness vs. BFS Weakness: Comparison of Symptoms
Here’s a comparison between the muscle weakness of ALS and that of benign fasciculation syndrome (BFS).
There are striking differences between the muscle weakness of ALS and that of BFS. (more…)
Is It Okay to Eat Lots of Sugar if Glucose Level Is Normal?

Do you have the green light to eat a ton of sugar in one sitting if your blood sugar level is in the normal range?
For example, you’re healthy and have a glucose monitor device at home. (more…)
How to Stop Worrying About Your Moles

Anxiety over your moles can get bad enough to disrupt productivity at work, ruin social events & cause insomnia.
However, you can overcome this nagging problem. (more…)
How Dangerous Is Blood Sugar in the 400’s?

You know it’s bad, but HOW bad is a glucose reading in the 400’s?
This can be “a very unhealthy place and could be a medical emergency,” says Alison Massey, MS, RD, LDN, registered dietitian and certified diabetes educator with over 10 years of experience in various community and clinical settings.
“The American Diabetes Association blood glucose target for healthy blood glucose management is 80-130 mg/dL before meals and less than 180 mg/dL 2-hours after eating,” says Massey.
“If blood glucose levels are in the 400’s mg/dL and won’t go down, an individual with diabetes may need to go to the emergency room.
“It is important for individuals to know how to handle elevated blood glucose levels, and if levels are elevated daily above the recommended ADA targets, they should discuss this with their healthcare provider.”
The Danger of Blood Sugar Readings in the 400’s
Over 400 is considered extremely high. There’s no such thing as “400 is as bad as 250.”
A glucose reading of 400 means there’s a heck of a lot of sugar in the bloodstream.
It poses two dangers:
• Hyperosmolar hyperglycemic nonketotic syndrome. The body will try to saddle the urine with the excess sugar.
The dehydration that results from this can cause seizures, coma or death.
Symptoms of HHNS: extreme thirst, high fever, vision loss, sleepiness, hallucinations, one-sided weakness.
• Diabetic ketoacidosis. Excessively high glucose levels cause acid buildup in the blood.
This, like HHNS, is a medical emergency and can cause coma or death.
Symptoms include frequent urination, sleepiness, nausea, trouble with breathing and confusion.
So these two conditions can occur with a one-time incident of a blood sugar reading in the 400’s. But what if this recurs?
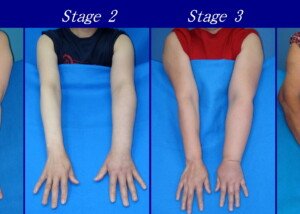
You might be facing retinopathy, which could result in blindness.
If that doesn’t scare you, what about kidney failure? How about loss of limbs?

Shutterstock/Tridsanu Thopet
These complications occur to many diabetics. Why? Because they do not properly manage their disease.
This includes failure to maintain regular glucose checks.
Diabetics need to do everything that their doctor and nurse tells them to do —everything to a T.
Diabetes doesn’t HAVE to shorten lifespan.
Blood sugar doesn’t jump into the 400’s for no good reason.
Alison Massey has been working in the field of nutrition since 2010 helping individuals make sustainable changes to improve their health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/donskarpo
Source: healthguideinfo.com/diabetes-complications/p97836/
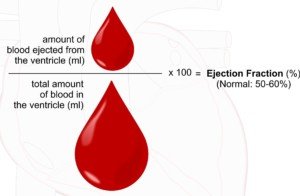
Edema, Swelling in Legs from Obesity vs. Heart Failure

How does one tell if the “edema” in their lower legs is strictly from obesity vs. congestive heart failure?
Though an obese person may also have heart failure, there are obese people who do not have this condition, yet have plenty of swelling in their lower legs. (more…)
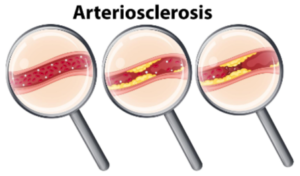
Does Echocardiogram Show Plaque Buildup in Arteries?
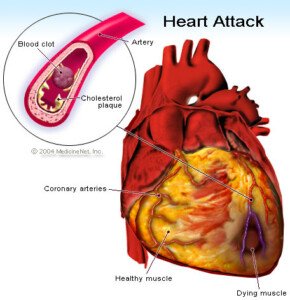
An echocardiogram is an ultrasound of the heart that, unlike a catheter angiogram (the gold standard for showing plaque buildup in arteries), is non-invasive and carries no risks.
The CT angiogram (CAT scan with contrast dye) shows soft-plaque buildup, but it also emits radiation.
A CT scan without contrast dye (the type used in identifying a person’s coronary calcium score) shows only hard-plaque buildup.
Hard or calcified plaque is stable and not prone to fragmenting or rupturing and forming a clot in a coronary artery.
But if the buildup of this plaque is great enough, it will cause narrowing of the coronary arteries, leading to angina.
Soft plaque is unstable; it can rupture and plug up a coronary artery in seconds, causing a heart attack.
Though calcium score correlates to the likelihood of varying levels of coronary artery disease, the score does not definitively mean that your arteries are clogged up with soft plaque.
Can an echocardiogram actually show soft plaque?
“No, an echocardiogram is an ultrasound that looks at the heart muscle and heart valves,” says Dr. Lowell Steen, MD, Interventional Cardiologist at Loyola University Medical Center, Director of the Interventional Cardiology Fellowship Training Program, and Medical Advisor to 120/Life, a functional beverage with a blend of six natural ingredients that promote normal blood pressure.
“It cannot look at coronary artery plaque. However, it can indirectly tell if someone is suffering from blockages or has had a silent heart attack. If the heart looks weak, blockages are often the reason.”
When my mother had an echocardiogram following chest pain and shortness of breath, the cardiologist said that it was “abnormal,” and that he didn’t feel good about her going home (she wanted to just go home and forget it all).
He did not say, “It shows a blockage,” or, “It shows that your arteries are clogged.”
An echocardiogram is much better at showing the following:
• Aneurysm
• Enlarged cardiac muscle
• Chamber abnormalities
• Valve problems
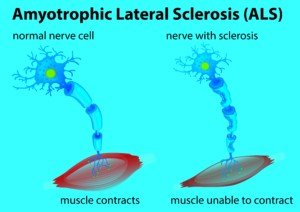
• Ejection fraction
• Inflammation
The doctor didn’t want to make a move on my mother based on just the echocardiogram.
But it was a first step; due to the abnormal finding, he wanted her to undergo the invasive catheter angiogram.
In my mother’s case, it was not determined she was having or had had a recent heart attack, despite her symptoms.
And her cardiac troponin result was in the indeterminate range.
But things were serious enough that he wanted the catheter angiogram.
The catheter angiogram, as mentioned, gives doctors a very clear picture of where blockages are, how much and whether or not bypass surgery is called for, vs. a stent placement.
It was impossible for the echocardiogram to reveal that my mother had five severely blocked coronary arteries, requiring a quintuple bypass surgery.
 Dr. Steen’s clinical expertise includes angioplasty, chest pain, coronary artery disease, heart attack, high blood pressure, valve disease, and vascular disease and intervention. 120life.com
Dr. Steen’s clinical expertise includes angioplasty, chest pain, coronary artery disease, heart attack, high blood pressure, valve disease, and vascular disease and intervention. 120life.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: vecteezy.com
Source:
hopkinsmedicine.org/healthlibrary/conditions/cardiovascular_diseases/echocardiography_echo_85,P00212/
Stabbing Chest Pain when Lying on Left Side: Heart or Muscle?
Chest Pain with Hoarse Voice: May Be Cancer or Aortic Aneurysm
Causes of Congestive Heart Failure in Younger Adults

Congestive heart failure isn’t just an “old person” disease; it strikes young adults—and for specific reasons.
The reasons differ from those for elderly people.
What Is Congestive Heart Failure?
Failure of the heart to adequately pump blood throughout the body. This failure can be systolic or diastolic.
• Systolic: The heart doesn’t pump or “squeeze” hard enough with each beat, and hence, an insufficient amount of blood gets pumped with each beat.
However, there’s a normal supply of blood in the heart ready to be pumped out.
• Diastolic: The pumping action is normal, but there’s an inadequate supply of blood in the heart to be pumped out. Thus, an insufficient amount of blood gets pumped with each beat.
Shutterstock/ellepigrafica
In elderly people, the two biggest causes of CHF are coronary artery disease and high blood pressure.
Should most younger adults worry about getting congestive heart failure?
If you take good care of your body and have no birth defect with your heart, the answer is NO.
Common Causes and Contributors of Congestive Heart Failure in Young Adults
“This is most commonly caused by cardiomyopathy, which is a condition characterized by a weak heart muscle,” says Morton Tavel, MD, Clinical Professor Emeritus of Medicine, Indiana University School of Medicine, and author of “Health Tips, Myths and Tricks: A Physician’s Advice.”
“The weakness can be a result of any of a number of causes, ranging from viral infections, toxic drug exposures or genetic predispositions,” adds Dr. Tavel.
• This familial (genetic) dilated cardiomyopathy usually becomes relevant in middle age, but it can strike young adults, even children. This is the condition that is often behind the sudden deaths of young athletes during sports play.
• Myocarditis (inflammation of cardiac tissue)
• Lesions on the cardiac tissue caused by drugs or alcohol
• High blood pressure
• Chronic kidney disease
• Low “good” cholesterol (HDL) may be a contributor.
• Obesity — and the more obese, the higher the risk.

Obesity puts significant strain on the heart. Shutterstock/Nomad_Soul
So in general, if you as a younger adult should worry about something cutting your lifespan short, it would be more logical to worry about car accidents.
Congestive heart failure in younger adults (20s to 40s) is often not considered by doctors as a possible cause of their new patients’ symptoms.
Symptoms typically start out as fatigue, tiredness (not sleepiness), shortness of breath (getting “out of breath” despite mild exertion or even casual exertion), rapid resting pulse, and slight and unexplained weight gain (from fluid buildup).
Progression of fatigue can occur over several weeks, joined by nausea, vomiting, swollen ankles and a distended stomach.
Fatigue, weakness and feeling drained of energy have several benign causes, and often, stress or a change in lifestyle (e.g., new baby) is blamed.
Incidence in U.S. of Congestive Heart Failure in Younger Adults
• The five-year risk of CHF among 40-year-old whites is estimated to be 0.1% to 0.2%.
• In one study, the incident rate in blacks was 20 times that of whites (1% of black men and women who were part of the study; average age 39).
• There is no explanation for the racial disparity, but chronic kidney disease is more common in blacks.
Take-home Messages
• Average people under 50 who lead a healthy lifestyle and have no evidence of congenital heart problems should not worry about “getting” congestive heart failure—but they should take measures to help prevent it.
• No matter how young an adult you are, KNOW YOUR BLOOD PRESSURE. If it’s high, get it under control.
• Know your cholesterol profile and get it under control if undesirable.
• Clean up your diet. The kidneys don’t like being burdened with the toxins that are found in highly processed foods, namely added sugars.
• Maintain a medically acceptable body weight.
• Exercise! Exercise strengthens the heart.
In case you’ve developed a heart condition, it’s very important to wear a medical ID bracelet so that in emergency situations people nearby will know how to help you.
Lauren’s Hope is producing interchangeable medical ID bracelets that are attractive, durable, stylish and can be worn by young adults without drawing any attention to their illness.

Dr. Tavel’s medical research includes over 125 publications, editorials and book reviews in peer-reviewed national medical journals. He was formerly director of the cardiac rehabilitation program at St. Vincent Hospital in Indiana. mortontavel.com
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/goodluz
Sources: Oxford Journal, New England Journal of Medicine
eurheartj.oxfordjournals.org/content/early/2013/07/29/eurheartj.eht278
nejm.org/doi/full/10.1056/NeJMoa0807265#t=article
nejm.org/doi/full/10.1056/NeJMoa0807265#ref3
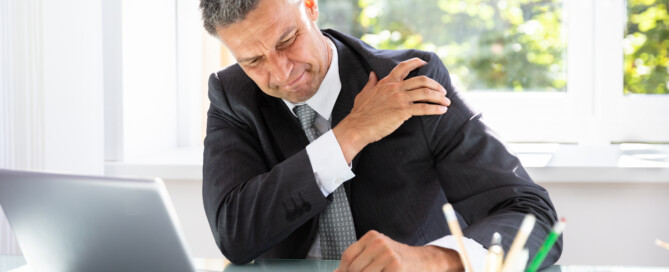
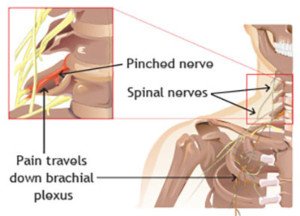
Shoulder Pain from Heart Attack vs. Pinched Nerve in Neck

There are distinctions in the shoulder pain from a heart attack vs. a pinched nerve in the neck.
But does this mean you can self-diagnose?
Shoulder pain from a heart attack can come on fairly suddenly, but so can pain caused by a pinched nerve in the neck (cervical vertebrae).
Biggest Difference Between Heart Attack Shoulder Pain & Pinched Nerve
Shoulder pain from a heart attack in progress (or very imminent one) will likely be accompanied by other key symptoms — either all, some or one other:
• Pain, squeezing, crushing or a vice-like sensation in the chest
• Feeling like you can’t get enough oxygen, shortness of breath, being winded even while at rest
• Nausea or upchucking
• Clammy cold and/or sweaty skin
• Lightheadedness, faint feeling
• Jaw pain
• Upper back pain, arm pain
A pinched nerve in the neck, though quite capable of causing a lot of shoulder pain, will not cause a feeling of being out of breath, shortness of breath, nausea/vomiting, breaking into a sweat, feeling faint, or pain in the chest or jaw.
What if a heart attack is causing just one symptom: shoulder pain?
A hallmark difference between heart attack shoulder pain and benign shoulder pain is that in the case of a cardiac event, the pain does NOT change with body position.
Shoulder pain from a pinched, compressed or irritated nerve that branches out of the spinal cord at the neck level will often fluctuate with body position.
“A pinched nerve can occur in the shoulder region in a defined area known as the thoracic outlet,” says Eugene Charles, DC, Diplomate of applied kinesiology and author of “Journey to Healing: The Art and Science of Applied Kinesiology.”
“The thoracic outlet is a narrow space between the collarbone and first rib located near your lower neck and upper chest where blood vessels, nerves and muscles pass through.
“It is surrounded by the neck flexor, upper trapezius and pectoral muscles. When this ‘pinching’ occurs, it’s known as thoracic outlet syndrome (TOS).
“When this happens on your left side it’s often confused with a heart attack (which you should go to the ER and rule out first).
“TOS differs from a heart attack in that these symptoms last longer and are affected by movement — meaning, if you slouch the symptoms intensify, and when you stretch out they dissipate.”
Furthermore, shoulder pain from a pinched nerve often comes with tingling, a “pins and needles” feeling, numbness and/or weakness down the arm, and/or these same symptoms in the hand or fingers.
These symptoms may come and go, and seem to correlate with body positions, whereas shoulder pain from a heart attack will not come and go with a change in body position.
There’s often some kind of pain in the neck and/or arm if there’s shoulder pain from a cervical nerve problem.
It’s usually a burning or sharp sensation. Some patients report that the pain is agonizing. Shoulder pain from a heart problem is not agonizing.
Shoulder pain from either a heart attack or a neck nerve issue often radiates or spreads down the arm.
This is what’s so scary, especially if there’s no numbness, tingling or “pins and needles” feeling present – AND especially if there’s jaw and/or chest pain!
“Let me start off by saying that this is NOT an area where self-diagnosis is a good idea,” says Roger Mills, MD, cardiologist and former professor of medicine, University of Florida, and author of “240 Beats per Minute. Life with an Unruly Heart.”
“If there’s a serious question in your mind, best to let a qualified medical professional evaluate the symptoms,” continues Dr. Mills.
“Second, my concern is not so much heart attack pain but the intermittent exertional discomfort called angina that signals a blood supply-demand mismatch in the heart.
“Angina is not always ‘chest pain,’ and chest pain is not always angina.
“Patients may sense the discomfort of angina in the shoulder (left or right), in the neck or jaw, or in the upper abdomen.
“The characteristic features of angina are that the discomfort comes on with exercise and is relieved by rest, and it is often associated with some sense of pressure or shortness of breath.
“In contrast, the sharp radiating pain from nerve root irritation may occur at rest, or with certain specific changes in position.
“The typical description [from a patient] is, ‘It hurts when I do this’ accompanied by a turn of the head or change in posture.”
What should you do?
“If you are experiencing a heart attack, time is heart muscle,” says Dr. Mills.
“Most medical centers in the U.S. now have programs that can significantly reduce the damage to your heart.
“Don’t sit at home and wait to see if it goes away.”
Though you may believe that the shoulder pain is from a recent incident in the gym, Dr. Charles advises,“When this occurs on your left side it can often mimic a heart attack. As a precautionary measure, you should immediately go to the ER and make sure it is not.
“Once cleared, you can go to your physical medicine specialist, such as a doctor of chiropractic or osteopathy, and be examined to see if your symptoms are from TOC.”
A trip to the ER will get you a blood test that can show if you had a heart attack.
A heart attack damages cardiac muscle, releasing a protein into the bloodstream which will be detected by the blood test.
If you’re cleared from having had a heart attack, you may be also be advised to see a neurosurgeon who specializes in the treatment of pinched nerves.
An MRI will show nerve compression in the neck.
Dr. Charles has helped thousands of patients and taught over 1,200 doctors during his 30+ years of practice. He has also created the Power Kinetics® Exercise Program and line of nutritional vitamins and performance supplements. amazon.com/Journey-Healing-Science-Applied-Kinesiology/dp/0964421763

Dr. Mills is the former medical director of the heart failure and heart transplant service at the University of Florida, was a staff cardiologist at The Cleveland Clinic and has authored over 100 peer-reviewed publications. “240 Beats a Minute” is available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: Shutterstock/Andrey_Popov
Source: orthoinfo.aaos.org/topic.cfm?topic=a00332
Best Strength Training Machine for Those with Diabetes

A person with diabetes walks into a gym and is overwhelmed by the different pieces of strength training equipment.
Strength training doesn’t have to be confusing or complicated. (more…)
How a Diabetic Can Build Big Muscles

Is there a difference between how a diabetic should train for building muscle and someone without diabetes?
Do the exercises differ? What about the bench press? (more…)