How Often Is ALS Misdiagnosed As Benign Fasciculation Syndrome?

There are cases in which someone with ALS was misdiagnosed with BFS.
Imagine the devastation when the patient finally receives the correct diagnosis.
From a clinical standpoint, early ALS can resemble benign fasciculation syndrome – at least from the subjective reporting of the patient.
How often is ALS mistaken for BFS by a doctor?
“Although ALS can be misdiagnosed as BFS, this is not common,” says Bonnie Gerecke, MD, director of the Neurology Center at Mercy in Baltimore.
There is no data on how often ALS is misdiagnosed as BFS.
Now it happens that initially, the patient may be told that their symptoms seem to be related to a number of conditions, one of which is benign fasciculation syndrome.
But this is not a diagnosis; it’s an initial assessment.
Dr. Gerecke explains, “The hallmark of BFS is muscle twitching in the absence of other pathological signs and symptoms.
“If a patient presents with muscle twitching and no other symptoms and has a normal examination other than for twitching, it is usually not difficult to recognize this syndrome.
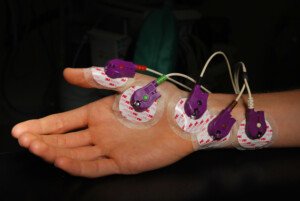
EMG test. Paul Anthony Steward, CreativeCommons
“ALS is associated with weakness and muscle wasting and not just isolated muscle twitching.”
A neurologist will have the patient perform some tests in the office to measure for weakness, and of course, the EMG will be very telling about whether or not nerve conduction is normal.
BFS is not progressive, but ALS is – and sometimes rapidly – and the associated weakness as it progresses is significant.
The bottom line is that it is rare for a person with ALS to be diagnosed with benign fasciculation syndrome.
But to learn just how this can happen, read this interview with Michael Cartwright, MD, a board certified neurologist at Wake Forest Baptist Medical Center in Winston Salem, NC. You will be very surprised by how he says ALS is diagnosed.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
ALS Muscle Twitching vs. BFS Muscle Twitches: Key Differences?

The term “twitching” is ambiguous; there are different kinds.
Certainly, there are variations between ALS muscle twitching and that of BFS.
What are the differences between the twitching muscles of ALS and those of BFS?
“In benign fasciculation syndrome, the muscle twitching is often widespread throughout the body,” says Bonnie Gerecke, MD, director of the Neurology Center at Mercy in Baltimore.
“For example, one can experience twitching in an arm, eyelid, torso or foot,” continues Dr. Gerecke, referring to BFS.
“The twitches in benign fasciculation syndrome are brief and can be frequent.”
You may feel these as very short-lived creepy-crawly sensations, or squiggly worm sensations, right under your skin.
These are especially apparent while you’re sitting still at a computer, while reading or watching TV, and can occur seemingly relentlessly.
With BFS, the twitching will stop the second you begin moving the affected area.
So if the twitching keeps recurring in a hamstring or quad muscle while you’re at the computer, it will stop when you get up and walk, march in place, or even remain seated but bounce the leg up and down.
With benign fasciculation syndrome, you may notice a predictable trigger, namely, whenever your calve muscle twitches, it’s always after you’ve run on a treadmill or used a stationary bike.
Or the twitching that runs rampant in your upper legs and butt always occurs after a rigorous hike. However, benign fasciculations can also occur randomly.
“In ALS, the muscle twitching often starts in one region and spreads locally,” says Dr. Gerecke.
“For example, there can be twitching isolated to the right hand and then it may spread to the right arm and then the left hand and the left arm.
“Also, in BFS, the twitching is not associated with other signs or symptoms [other than maybe cramping of the muscles].
“In ALS, when a patient experiences muscle twitching, there is almost always associated muscle atrophy (shrinkage of muscles) and muscle weakness.”
Early ALS muscle weakness is often asymmetric, may be subtle but may also be more suddenly obvious, and it is also painless.
Be on the lookout for new-onset clumsiness, tripping or difficulty with routine tasks.
- A very concerning sign is when these issues are getting worse.
- BFS does not make tasks difficult or cause stumbling or clumsiness.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Alexander Raths
Break Deadlift Plateau in Middle Age with One Exercise

It is just ridiculously aggravating when you’ve hit a plateau in the deadlift, especially if you’re middle aged and wondering if this is a sign you’ve reached your all-time limit. (more…)
Will the Rack Pull (Top Deadlift) Thicken a Woman’s Back ?

The rack pull is a great strength training move that very few women do out of fear it’ll bulk their back.
Absolutely false; rack pulls will burn fat and do several wonderful things for a woman – without bulking up her back. (more…)
Bulbar Onset Symptoms vs. Laryngeal Cancer: Symptom Comparison

Laryngeal cancer is one of the scariest diseases, but it would be appealing to someone who’s just been diagnosed with bulbar onset ALS.
Symptoms overlap in these two conditions.
“Both conditions can be associated with hoarseness,” says Bonnie Gerecke, MD, director of the Neurology Center at Mercy in Baltimore with a special interest in neuromuscular disorders, ALS and EMG.
So if you’ve had an unexplained, persistent hoarse voice lately … and no other symptoms with it … it’s understandable how you can be in a state of panic.
Bulbar Onset Symptoms
“There are many different bulbar onset symptoms,” says Dr. Gerecke.
“These include the following: dysarthria (slurred speech), dysphagia (trouble swallowing), trouble chewing, drooling, moving the tongue in the mouth and hoarseness.”
Difficulty speaking (dysphonia) is also a symptom, and this may occur without slurring. The tongue will also shrink due to eventual atrophy.
And of course, there’s the tongue fasciculations, but these are not the same “twitches,” tremoring or quivering that a healthy person sees when they stick out their tongue and inspect it.
It’s impossible to keep the tongue perfectly still when inspecting it, especially if you’re scared of what you’ll see.
The tongue is not designed for meticulous control of movement. It’s not like a finger that you can hold perfectly still.
The tongue twitches of bulbar onset ALS are undulating and wormlike.
Laryngeal Cancer Symptoms
Dr. Gerecke says, “In contrast to bulbar symptoms due to ALS, patients with laryngeal cancer often experience pain when swallowing. They may also experience sore throat, a lump in the neck and cough.”
Bulbar Onset Symptoms that Laryngeal Cancer Will Never Cause
• Speech characterized by “effortful, slow productions with short phrases, inappropriate pauses, imprecise consonants,” says a report in the BMC Ear, Nose, and Throat Disorders (Nov. 2001).
• Slurred speech
• Breathy speech
• Trouble chewing, a feeling of weakness when doing so
• Difficulty moving the tongue within the mouth
• There may be lip involvement very early on, affecting swallowing.
• Saliva control when eating. There is excess saliva regardless of eating as the ALS progresses.
• Tongue atrophy
• Tongue fasciculations
Laryngeal Cancer Symptoms that Bulbar Onset ALS will Never Cause
• Sore throat
• Constant coughing
• Pain when swallowing, though there is no mechanical difficulty.
• Ear pain
• Lump in the neck
• Weight loss
Symptoms Shared by Bulbar Onset ALS and Laryngeal Cancer
• Hoarse voice, though not all laryngeal cancers cause this.
• Trouble swallowing
• Trouble breathing (ALS causes this via a vocal cord spasm)
Benign conditions such as LPR can cause some of the symptoms listed here.
Laryngeal cancer is a very uncommon disease, and bulbar onset ALS affects about one in 300,000 people.

Dr. Gerecke has a special interest in ALS, myasthenia gravis, myopathy/muscular dystrophy, peripheral neuropathy and radiculopathy. She is board certified in general neurology and neuromuscular medicine.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/ShotPrime Studio
Sources:
ncbi.nlm.nih.gov/pmc/articles/PMC60006/
cancer.org/cancer/laryngealandhypopharyngealcancer/detailedguide/laryngeal-and-hypopharyngeal-cancer-signs-symptoms
als.ca/sites/default/files/files/Bulbar%2520ALS.pdf
Can a Groove in the Thigh Muscle Ever Be an ALS Symptom ?

The groove or indentation appears in one thigh only, so this may mean the muscle is starting to waste away or atrophy from ALS, and unfortunately, this is the erroneous thought process that many people have when inspecting their body out of ALS fear. (more…)
Can You Be Anorexic but Not Thin or Underweight?

First of all, not all women who appear “too thin” have an eating disorder.
Anorexia nervosa is a term that many laypeople associate with a particular body appearance: emaciated or one that appears “way too thin” — such as the body of film star Angelina Jolie. (more…)
Why Don’t Stomachs of 600 Pound Life People Ever Rupture?

There are cases of people who’ve fatally ruptured their stomach from eating enormous amounts of food in a short period of time.
The “600 Pound Life” subjects apparently have not suffered this fate. (more…)
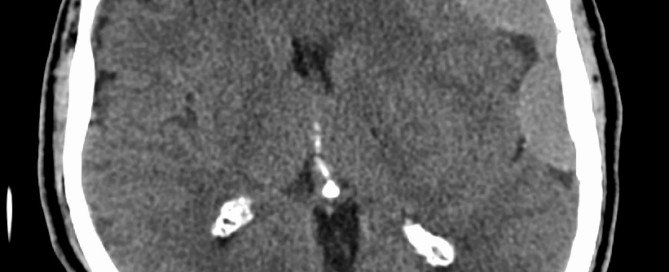
Can Chronic Subdural Hematoma Increase Risk of Alzheimer’s?
You may already know that a chronic subdural hematoma can cause permanent physical disability.
But what about an increased risk of Alzheimer’s disease?
Can the bleeding that contacts the brain set in motion a chain of biochemical events that ultimately lead to the development of Alzheimer’s disease or some other form of dementia?
A chronic subdural hematoma is a gradual or slow bleeding in the brain that occurs over weeks, following some type of trauma such as hitting one’s head on a car door frame, a slip-and-fall or a whiplash injury that jars the brain.
A cSDH is far more likely to occur in elderly people because, due to age-related brain shrinkage, there’s more room between the brain and dura, making it easier for veins to be torn.
However, it can also happen from head trauma to people in their 50s and 60s.
Blood thinning drugs, too, can cause a cSDH in elderly people.
Symptoms of Chronic Subdural Hematoma
The symptoms resemble those of a stroke and include cognitive impairment.
The patient won’t have all the possible symptoms since symptoms depend on the location of the bleeding.
However, a gradual onset of what seems like early Alzheimer’s can definitely be a symptom in an elderly person who, several weeks prior, banged their head from a fall or even just “nicked” it on an open cupboard door.
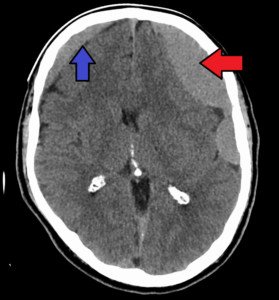
In fact, sometimes the diagnosis is highly suspicious for dementia —until a CT scan reveals the bleeding.
So on one hand, it’s accurate to say that a chronic subdural hematoma can cause symptoms mimicking dementia or Alzheimer’s disease.
But once the collection of blood and fluid is drained via a burr hole procedure, the patient usually has a full recovery. The “dementia” was temporary.
But is it possible for this insult to the brain tissue to raise the risk of future development of Alzheimer’s disease?
”Chronic subdural hematoma is very common in people within the older age group,” says Dr. Urvish K. Patel, MD, MPH, a research associate in the Department of Neurology at Creighton University School of Medicine/CHI Health.
“Due to an ageing population, chronic subdural hematoma is projected to become the most common adult neurosurgical diagnosis.
“Due to oxidation-reduction reactions in chronic subdural hematoma and exerting its effects using cytokines and inflammatory mediators, cSDH leads to neurotoxicity and inflammation-related brain atrophy.
“In such circumstances, it increases the risk of Alzheimer’s disease and dementia.”
Causes of Alzheimer’s Disease
In under five percent of cases, a genetic variant that’s present since birth will lead to the disease, though the mechanism is not known.
In the remaining 95 percent of cases, nobody knows just what exactly causes Alzheimer’s. What’s known, however, is what it’s associated with.
• Plaques. It’s believed that the presence of beta-amyloid plaques kills brain cells, but again, the mechanism of cell death is not known.
• Tangles. A protein called “tau” is key to the system of support and transport of nutrients to brain cells.
In the brains of Alzheimer’s patients, tau protein is tangled up inside brain cells, crippling the system.
Commonly Known Risk Factors for Alzheimer’s
• Age 65+
• Immediate family member has the disease.
• MCI: mild cognitive impairment in older age that’s more than what would be expected for that age.
• History of severe head trauma (e.g., car accident, ladder fall).
• Lack of exercise
• Obesity
• High cholesterol
• High blood pressure
• Smoking
• Poorly managed type 2 diabetes
• Lack of vegetables and fruits
• Sub-high school education level
Age-related changes in the brain are also suspect as causative factors in Alzheimer’s. These include:
• Brain shrinkage
• Inflammation
• Free radicals
• Breakdown of a cell’s energy production
Delayed Treatment of a Chronic Subdural Hematoma
This heightens the chance of permanent deficits, as was the case with a 60-something man at my gym who was initially misdiagnosed a month after he fell and hit his head, then finally properly diagnosed a month after that.
By then the continuing buildup of blood and fluid in his brain had caused irreversible damage to the right side of his body — but left him cognitively intact.
A cSDH can be missed on a CT scan.
For optimal brain health, one should avoid the modifiable associated risk factors with Alzheimer’s.
 Dr. Patel’s areas of interest are outcomes and survival studies and clinical trials in neurology, neuroepidemiology and translational medicine research.
Dr. Patel’s areas of interest are outcomes and survival studies and clinical trials in neurology, neuroepidemiology and translational medicine research.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Can Anabolic Steroids Cause Bleeding in the Brain?
Long-term use of anabolic steroids can cause damage to the brain.
There are many causes of bleeding in the brain.
Some of these bleeds occur slowly and some are instantaneous and thus immediately life-threatening. (more…)