Being that it’s not acute and can be caught in time, how is it that sometimes people die from a chronic subdural hematoma?
After all, this condition is relatively very easy to treat.
Now in the case of an acute subdural hematoma, it’s simple to see why this can kill a person within minutes: sudden gushing of blood inside the brain, quickly sweeping over brain tissue.
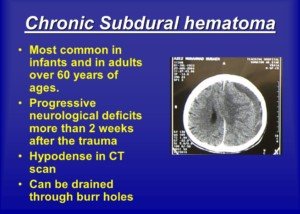
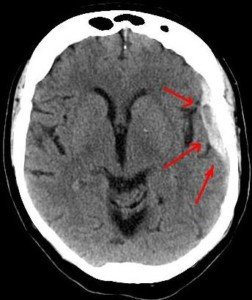
A chronic subdural hematoma is what its name suggests: It occurs over a period of weeks; it’s slow in progression—very slow—enough so that the first symptom may not appear until three months following the insult – which is typically a fall or bump to the head.
Nevertheless, people DO die as a result of a chronic subdural hematoma.
Typically a cSDH is treated with a non-invasive surgery: burr hole craniostomy with a closed-system drainage.
Reasons for Fatal Chronic Subdural Hematoma

Credit: Alpha Prod
• Severe delay in seeking treatment; patient is comatose upon admittance to hospital.
• Postop complication: acute SDH.
• Postop: intracerebral hemorrhage (not the same as acute SDH).
• Postop: infection
• Postop: cerebral edema/swelling (caused by compressed brain surface caused by impaired vein drainage)
• Postop: disseminated intravascular coagulation (blood clots forming in the brain).
• Pneumonia following the burr hole procedure. A paper in Neurosurgical Review, March 2002, cites pneumonia as the most common postop complication.
The less healthy the patient is preop, the more vulnerable they’ll be to pneumonia. Excessive inertia postop also raises the risk of pneumonia.
Treatment Delay
In an industrialized culture, delay in treatment is rare, simply because the symptoms are difficult to ignore – especially when the patient lives with someone.
However, shut-ins or those who have very little contact with people and who are not of sound mind are at risk for serious delay of seeking treatment.
People in non-industrialized cultures are also at high risk of delayed treatment.
Another risk factor for delayed intervention of a cSDH is when the patient has already been diagnosed with a condition that can mimic a cSDH.
Family members may pass off the cSDH symptoms as just part of the current condition.
If bleeding inside a brain — albeit the slow nature of a cSDH — is left untreated, then yes, it will probably become fatal.
Intracerebral Hemorrhage
This very rare complication post-evacuation of the blood and fluid buildup of a chronic subdural hematoma can be fatal.
It can arise from impaired blood clotting (coagulopathy), leading to fast-onset hemorrhaging.
Why this would be a postop complication isn’t always clear, but a pre-existing issue with blood clotting, when combined with cSDH treatment, can lead to the hemorrhaging.
However, there may be no pre-existing pathology other than the actual cSDH itself.
Other possible causes:
• Damage to blood vessels caused by the brain shifting sideways which is caused by the hematoma.
• Sudden increase in blood flow, combined with defect in blood flow regulation.
• Bleeding into a previously undetected bruise in the brain.
• Chronic enlargement of small arteries and buildup of carbon dioxide.
As frightening as this sounds, treatment of chronic subdural hematoma has a good prognosis in general.