Best Exercises for TOP Body Heavy Women
“Top heavy” women who carry excess weight mostly in their upper body often avoid strength training exercises for this area for fear of making it even bigger.
Myth: Training the upper body with weights, in women who are top heavy all over, will make them bigger.
This skewered logic assumes that resistance workouts will convert the excess fat in a woman’s upper body to muscle.
This is physiologically impossible, as muscle and fat are two different types of tissue.
For instance, a back exercise will not increase the size of the fat cells in a woman’s back.
An upper-body exercise will not enlarge the fat cells in her heavy arms or elongate the long bones in her shoulders.
Myth: If top heavy women woke up one day with a lower body to match (excess fat in the lower body too!), it would then be okay to strength train the upper body.
Isn’t it odd that women who are large only in their upper body, with “skinny” legs, shy away from upper-body strength training, but if they ALSO had heavy legs and “fat” hips, they’d probably be strength training their upper body with less fear of getting larger?
In other words, the belief that lifting weights will bulk up a top heavy woman only seems to apply to those who have skinny legs, but not to those who are heavy both in their upper and lower body.
The fat loss and size reduction virtues of strength training apply equally to women who are big on top but thin on the bottom and women who are big on top AND the bottom!
Myth: Women who collect excess fat only in their upper body are more prone to developing masculine muscles via weight training.
This is similar to the previous myth, in that somehow, the idea persists that disproportionately thin legs predispose a woman to excess muscle development from resistance workouts.
Myth: A woman who hasn’t been strength training, but whose upper body is disproportionately bigger than her lower body, has a lot of natural muscle in her upper body.
Why is it that when a woman is pear shaped (all the fat collects in her lower half), she sees this as excess fat, but when her legs are trim but her upper half is disproportionately large, she thinks this is excess muscle?
Wrong. In some women, excess fat just happens to accumulate in the back, stomach, torso and upper arms. It’s fat, not muscle.
And let’s say these women began eating way more than they usually do. Eventually, excess fat would begin appearing in their legs.
There’s no such thing as a 250 pound woman who has a size 8 lower body.
I’ve seen 160 pound women with size 8 legs, but not 250 pounds. Not even 200 pounds (assuming they’re not 6’4”).
Best Exercises for Women with Large Upper Bodies
Best exercises if you have the so-called top heavy body (and I don’t mean breast size, but broad back, an “apple” shaped body, heavy arms):
#1. Deadlift
#2. Squat
#3. Lat pull-down
#4. Bench press
#5. Leg press
#6. Kettlebell swing
There are several other exercises, but these are an excellent start.
Deadlift. This king calorie burner works virtually every muscle group in one movement. No gimmicks.
Just pick a barbell off the floor, pushing upward with your legs as you straighten your back, keeping your arms straight.

The starting position for the deadlift
The fat burning will occur where your body has excess fat: the upper part.
It crushes stored body fat only when moderate to heavy weight is used. Deadlifting 70 pounds for 20 reps won’t cut it.
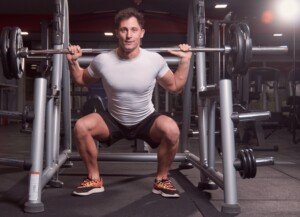
Squat. With a barbell across your back, a squatting program will raise your body’s energy needs (as will the deadlift and the other exercises here).

The back squat
Your body will dip into stored fat for this energy.
If it’s in your legs, your legs will get trimmer. If it’s in your back, stomach and upper arms, those areas will get trimmer.
There are other varieties of squats, but the barbell version allows for the most weight to be moved.
Lat pull-down. Though this works the very area that some women think they’re already too big, this doesn’t mean it will make it bigger.

The lat pull-down. Freepik
Remember what I said: It’s physiologically impossible for strength training to convert fat cells to muscle cells.
The lat pull-down, like the other exercises here, is a compound move, and will raise your body’s energy needs…
And so will the bench press, which targets three muscle groups. This will melt fat where you need to have it melted.
The leg press will help shrink fat cells in your back, torso, stomach and upper arms because, again, this is a compound move which will drive up your body’s energy needs.

The leg press. George Stepanek, CreativeCommons
Legs and glutes are the largest muscle groups. They drive up the body’s energy needs the most, which is why slamming the legs will shrink fat cells in the upper body.
Kettlebell swing. My formula is to perform 15 to 25 reps with a kettlebell that’s heavy enough to bring you to breathlessness in this rep range.

The kettlebell swing. Shutterstock/Jacob Lund
If you can talk right after the set, the bell isn’t heavy enough. After 15-25 reps, you should be friggin’ panting for 45 seconds.
These are among the best exercises for women who have thin legs but a big or “top heavy” upper body, but only when the right rules are followed:
Use a weight heavy enough for an eight to 12 repitition max, and use correct form and technique. Avoid these mistakes with the lat pull-down.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Smelling Urine when None Is Around

There’s at least one explanation why you smell urine when none is around or in sight.
I know this because one day I began smelling urine.
But I knew none was around because anyone in my home would (like most humans do) use the toilet to relieve themselves.
I don’t own cats or other pets.
Where was this urine odor coming from?
It wasn’t originating in the bathroom. The smell of urine was strongest in three places of my home:
• Right upper shelf area of my bedroom closet
• Heating vent in kitchen
• Heating vent in office
The foul smelling stench, which definitely had other components to it aside from urine, had come on suddenly; one day I just began noticing it.
Above the shelf in the closet was a trap door, that when opened, revealed some piping.
I surmised that this mysterious odor of urine was somehow connected to the pipes (a broken pipe releasing sewage?) that ran through the townhome four-plex, perhaps originating underground.
It certainly wasn’t from anything inside my home, but rather, something that was making its way through the pipes and into the ventilation system.

Thus, the smell of urine was in different rooms, and strongest the closer my nose got to the heating vents that ran along the baseboards, and of course, that trap door in my closet.
I’m going to make a long story short and tell you outright what the cause of this urine stink was:
The two men next door to me were hoarders. For years the hoarding had been escalating (but nobody knew), until finally, whatever stench there was inside their unit began permeating common building fixtures, making its way into MY unit.
I ultimately discovered this when I stepped outside and hovered near their window and sniffed out the same odor.
The people on the other side of them reported to me that, though they didn’t smell the combination of urine, feces and garbage inside their unit, they certainly smelled it badly enough on their deck that it interfered with enjoying their deck.
The woman next to them told me that one of the men would put pants that had feces on them into the common-room washer and dryer, and clumps of feces would remain behind, inside the machines.
(I had my own washer and dryer, thank goodness.)
If you begin detecting the odor of urine inside your house, but you’re positive that there’s no puddles of urine left by a cat, dog, toddler or someone else just playing a prank…
…consider the possibility that it’s the awful odor coming from the people who live right next door to you — especially if the stink is strongest near trap doors that open to pipes, or at heating vents and air ducts, which are conduits for the concentration of vapors (for lack of a better term) of the wastes.
How I Got Rid of the Smell of Urine
I aggressively pursued eviction of these two men, who were renters to the son of the previous owner of their unit.
The son had inherited the unit from his father who had passed away, and he didn’t want to be bothered with the situation; as long as he got his rent check every month.
My persistence paid off, and the son, plus a friend, one day showed up wearing gas masks and began clearing out the place.
(It ultimately had to be “gutted out” and rebuilt from the inside.)
They said there were piles of garbage everywhere, plus numerous paper cups filled with urine — all over the place.
A cop whom I had initially called to come over and speak to these men had told me that when he pulled into the lot, he had smelled the odor right then and there — and thought there was a corpse inside the unit.
He spoke to one of the men at the doorway, remaining outside, then told me, “That odor is FOUL!”
The men were evicted, but the landlord offered to put one of them up in a motel for a month, while the other went to a nursing home, where the environment was certainly a lot cleaner and safer.
If you suddenly begin smelling urine … and there’s none in sight … consider the possibility that nothing is wrong with your nose, but rather, there’s a hoarder nearby.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer for Bally Total Fitness.
.
Top image: Shutterstock/9nong
Lost Weight but Still Have Fat Belly: Cause, Solutions

The weight is all lost but the fat in your belly remains, but once you know the cause you’ll be able to cure this problem.
I’m first going to tell you the solutions to the problem of still having excess fat in your gut despite having lost all the weight you wanted.
But be forewarned: You will be stunned at the solutions to getting rid of BELLY FAT after you’ve lost all your desired weight:
- Intense strength training that targets the legs, back and chest
- High intensity interval training (HIIT), a form of cardio exercise

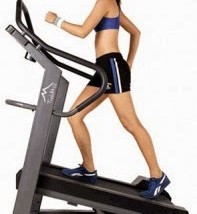
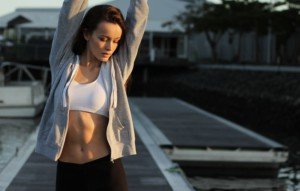
Squats target the entire lower body but also the core.
Pretty shocked, right? Nowhere in these solutions do I mention “belly,” “abs” or “stomach.”
Once you understand why hitting the legs, back and chest hard with strength training, and engaging in twice-weekly HIIT will solve your problem, you will be very eager to embark on these solutions to get rid of that remaining fat in your belly once and for all.
Why Your Belly Is Still “Fat” Despite Having Lost All the Weight

Shutterstock/Ben Gingell
Most likely, you lost all of your weight (reached your goal according to the scale), with the simple formula of calories in vs. calories out.
This approach was also likely combined with more exercise than you normally do in your life.
Most people who go on a diet for weight loss increase their physical activity in some way.
But even though they’re now consuming fewer calories and have added an hour of walking in the park to their efforts (or maybe it’s a group fitness class, use of cardio equipment and even some strength training), the net result is ONLY weight loss.
But isn’t that what you want? Well of course, but here’s the problem with ONLY weight loss: This doesn’t mean your body composition has changed.
You’ve whittled down the number on the scale, but your body composition is essentially the same. You may even be termed what is known as “skinny fat.”
You fit into that size 8 dress, but that mushy gut is still there.
If you’re a man, you have that potbelly or paunch going on, even though the rest of you looks trim.
Your body’s energy needs are not high enough to use the fat in your belly for fuel.
You can read all you want about hormones like leptin, ghrelin and estrogen, but the bottom line — the simplest explanation — is that your body just doesn’t have a need to plunge into the fat storage of your stomach and convert it to fuel.

Sled pushing will attack belly fat.
The solution is to increase your body’s energy demands.
That hour walk, that “body pump” class, those three-times-weekly stints on the elliptical machine, and your current strength training program (if you even have one!) are just not enough to…
…DRIVE UP YOUR RESTING METABOLISM.
Cure for Belly Fat After You’ve Lost Weight
You must give your body a reason to ransack the fat depos in your stomach: Slam your legs, back and chest with resistance workouts.
But wait…maybe you’re already doing that — or so you think.
As a former personal trainer, I can’t begin to tell you how many men and women (new clients) reported to me that they were already hammering their body with various routines…
…but it turned out they were doing nothing of the sort. They weren’t lying; it’s just that they didn’t know what intensity really meant.
A 3.5 mph walk on a treadmill at 15 percent incline while holding on does not qualify as an intense workout. An old lady can do this if she holds on hard enough.

Think of it this way: “If an old lady can do it, it probably won’t burn much fat.” Shutterstock/lunopark
And doing lat pull-downs with a weight so light that you can do 20 reps even though you stop at 12, well, that’s hardly intense, either.
And spending half your gym time doing isolation exercises (dumbbell kick-backs, biceps curls, crunches, side bends, sit-ups) won’t pump up your body’s energy needs, either.
Trash the abdominal exercises. These target very small muscles which use very little energy.
Stop spending so much time on the triceps and biceps targeting routines.
Stop trying to balance on one leg while lifting little dumbbells out to your side.
The largest muscle groups are the quads, hamstrings, glutes, back and chest.
If you subject these muscle groups to crushing routines, this will dramatically spike your body’s energy needs.
So much so, in fact, that your metabolism will remain elevated even while you sleep.
In fact, in the hours right after a grueling weightlifting regimen, your body is in a state of deficit.
Now here’s the million dollar question: Where is your body going to get the energy it needs to recover from these strenuous workouts?
STORED BODY FAT
Where is most of your body fat stored? Your belly!
If you pummel your quads, hams and glutes with intense squats and leg presses, your body’s energy needs will skyrocket.
I’ve seen it with my own eyes: Skinny fat clients, with thin arms and legs but a plump midsection, slamming their legs with squats and leg presses and other big movements—and over a period of weeks, by golly, their stomach shrinks!
And this was without any ab-targeting exercises like crunches!
The Followng Exercises will Slice and Dice the Fat in Your Belly
- Barbell and dumbbell squat
- Deadlift (king fat-burner!)
- Leg press
- Seated row
- Standing barbell row
- Lat pull-down
- Bench press
- Dumbbell press
- Standing overhead barbell press
- Kettlebell swing

Deadlift. Freepik.com

Kettlebell swing. Shutterstock/The Faces
Barbell squat. Shutterstock/HD92

Leg press. Freepik/master1305

Lat pull-down (narrow “V” grip). Zennis Se/Pexels
Stick with this plan for 30 days and see what happens to your waistline.
Don’t just go through the motions with these exercises. You really need to work hard.
I can go on and on about how many times per week, how long per session, but this article is getting long enough without doing that.
But here’s a real simple rule: If you can complete 13 repetitions, even with difficulty, increase the resistance.
If you cannot complete eight reps, reduce the resistance.
Your rep range should be eight to 12; an 8-12 rep max. You should be battling it out for that last repetition.
Rest times should average 60-90 seconds in between sets.
Stick to this program and the pudge in your belly will go away, and you’ll also get leaner (less body fat) in your arms and legs too: a more “buff” look, though your NET weight loss may stay about the same as your body composition changes.
Here is how HIIT can strip off fat.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Shutterstock/ESB Professional
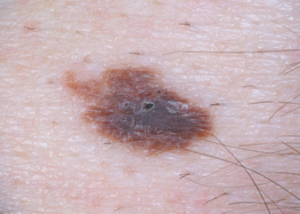
Why Is Pencil Eraser Size for Melanoma Symptoms Important…

Why is the pencil eraser size so emphasized when many melanomas are so much smaller?
Nearly every pamphlet on melanoma, and also just about every quoted dermatologist for a magazine or online article about melanoma, will state that one of the signs to watch for with this skin cancer is that of the “pencil eraser” sized mole.
But just what does this mean? Because many normal moles—moles since childhood—are the size of a pencil eraser.
My nephew has a back full of moles the size of a pencil eraser.
Are normal moles that are the size of a pencil eraser simply more likely to develop into melanoma when compared to moles that are only one millimeter?
“This [reference to pencil eraser] comes from data looking back at risk factors of melanoma,” says Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology; she practices at Westlake Dermatology located in Austin, Texas.
“The most common risk factors that are discussed are the ABCDEs of melanoma:
1 Asymmetry
A jagged or notably uneven edges and/or an overall odd shape.

Or, if the mole is bisected, one side is clearly not equal to the other, but keep in mind that moles, especially larger ones, are rarely perfect circles, and an oblong mole can still be symmetrical).
2 Border that’s irregular.
Again, few moles are perfect circles as though drawn with a compass.
But sometimes, a border is noticeably erratic.

3 Colors: multiple
It’s common for a normal mole to contain two or three shades of brown, especially larger moles.
But be VERY leery of new color configurations or a newly appearing odd color like maroon, reddish brown, red, purple, grey or black.
4 Diameter
This is larger than a pencil eraser.
5 Evolving

CDC, Carl Washington, MD, Emory Univ. School of Medicine, Mona Saraiya, MD, MPH
“These are some of the most common features of melanoma based on numbers,” says Dr. Gordon.
“However, some melanomas have none of these features, and all melanomas start smaller than a pencil eraser, so if you notice a new spot that seems to be changing or doesn’t look like any of your other moles, then get it checked!”

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Might a Bluish Black Freckle Be Melanoma?

Does that bluish black freckle (or what IS it?!) have you panicking it might be melanoma?
“The bluish color in many pigmented lesions represents pigment that is deeper in the dermis than the pigment that appears brown or black,” explains Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology; she practices at Westlake Dermatology located in Austin, Texas.
“This is called the Tyndall phenomenon and it is all physics. Blue nevi can be benign but also can be atypical or melanomas.”
The Tyndall effect is when light gets scattered by the matter that it hits. In this case, the matter is the pigmented cells of a freckle or mole (nevus; plural: nevi).
There is no connection between this scattering and the likelihood that a mole or freckle will morph into melanoma.
It’s just that people aren’t used to seeing skin pigmented spots showing as bluish black.
That all said, Dr. Gordon points out that these pigmented spots are not exempt from the rules of self-skin exams.
A bluish black mole or freckle needs to be checked for any changes that could signal cancer, but do NOT panic simply because the spot has a blue or blackish tinge to it.

Dannii Brighton, CC
These colors, in and of themselves—if the spot has always appeared this way — do not signal the presence of melanoma or the increased risk of this cancer.
The key, says Dr. Gordon, is the ABCDE’s of melanoma:
- Is the spot or mole noticeably or newly assymetrical?
- Is the border jagged or odd looking?
- Is the color changing? Yes, changing is the key word, since normal moles can be grey, light tan, blackish and even red.
- Is the diameter the size of a pencil eraser? Larger moles are more likely to become malignant.
- Is the mole evolving, changing in some way, developing a crust or bleeding or itching, for instance?
Make note of the colors of your moles.
Have a dermatologist especially check the ones that concern you, especially the bluish black ones.
For added peace of mind, request that the doctor examine your moles with a dermatoscope — a handheld lens that magnifies and illuminates the pigmented area.

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
How Fast Can Melanoma Spread After It First Appears?

Melanoma on the bottom of a foot.
You of course may not think the tiny speck is melanoma, but over time, it’s going to get bigger or spread superficially.
How long does this take to happen, or to put it another way, how fast does this spreading or growth occur?
“Melanomas can either have not spread past the skin or already be metastatic by the time you find a 1 mm lesion,” says Dr. Jennifer Gordon, who is board certified by the American Board of Dermatology; she practices at Westlake Dermatology located in Austin, Texas.
Dr. Gordon points out, however: “A 1 mm lesion would be rare to be already metastatic.”
This would be the nodular type of melanoma, which is an uncommon sub-type of this skin malignancy.
“I realize this offers little comfort, but it is the unfortunate truth,” continues Dr. Gordon. “There are multiple types of melanomas, such as:
- Melanoma in-situ
- Lentigo maligna melanoma
- Superficial spreading melanoma
- Nodular melanoma
- Desmoplastic melanoma, etc.”
This is why a new, though tiny, spot or speck should not be ignored, even if it looks normal.

Melanoma
“Ultimately I believe genetics will help determine the behavior of these, but until we have that data we have to look at patterns,” explains Dr. Gordon.
“In general, survival rate of melanomas depends on depth of the cancer.”
This depth is determined by a dermapathologist who examines a biopsy of the suspicious spot, which includes a surrounding margin of skin also taken out, under a microscope.
The rule of thumb is that the height of the melanoma above the surface of the skin is equal to its depth below the skin surface.
Dr. Gordon explains, “In general, smaller lesions (and the earlier you detect them) — the thinner they are and the better outcomes people have.
“Some melanomas will grow in a spreading pattern on the skin [the superficial spreading type], but some will grow in a deep pattern that are more aggressive [nodular type].
“There is no easy way to decipher the spread of melanoma until it is biopsied and sometimes until further tests are performed.”

Dr. Gordon’s interests include medical dermatology, particularly the treatment and prevention of melanoma and other skin cancers in athletes. For 2016, 2017 and 2018 Texas Monthly Magazine selected her as one of the Texas Super Doctors Rising Stars.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Does Melanoma Make You Get More Normal Moles Every Year?

So if you’ve been diagnosed with melanoma, will this make more normal or regular moles appear on your skin year after year? (more…)
Can Lifting Weights Only Once a Week Build Muscle?

Is strength training only once a week worth it for muscle gain?
Here’s a better question: Why would you want to limit strength training to just once a week?
Here is the answer to the first question: Strength training once a week will induce a training effect, even in older people.
Many bodybuilders strength train one muscle group per week, and see plenty of gains. However, they do so very intensely.
I blast my chest muscles, for instance, once a week. But on other days I’m also exercising, but not the chest muscles.
The Human Performance Laboratory at Ball State did a study with literally once-a-week exercise.
It was strength training, however, and the researchers found that the study subjects (men over age 70) maintained the effects of strength training.
However, the experiments started the 10 men off with a three-times-weekly progressive resistance program for three months.
After that, they were divided into two groups: One group continued strength training but for just once a week for six months, and the other group stopped altogether.
After six months, the first group had maintained the benefits picked up during the three-month progressive program, and the second group lost significant thigh muscle size and strength.
These findings don’t mean you should settle for a once a week program. There are over 600 muscles in the human body.
Once a week strength training is not practical if you want your entire body to be affected.
I’ve heard of people spending several hours in the gym for one session, once a week, hitting all the major muscle groups.
But I can’t imagine doing bench press, dumbbell press, squats, dips, deadlifts, lat pull-downs, pushups, leg press, rows and chin-ups all in the same workout. There is no way I could go all-out on these routines in the same session.
If you’re used to giving a routine all you have, you’ll be trashed long before you’ve covered all the major muscle groups.
Of course, you can go lightly, but I’m an advocate of intense exercise. If you strength train lightly all muscle groups, once a week … again, expect minimal results.
If you are hell-bent on working out lightly, then you should do it three times a week, and not two days in a row.
The Ball State study involved low volume, high-intensity strength training, which does not surprise me; high-intensity workouts can maintain their effects with just once a week.
Apparently, the men in the study exercised only their legs. The study summary did not mention other muscle groups.
As for that second question, why would you limit strength training to once a week, the allegedly No. 1 reason is lack of time, even among retired folks.
Ask yourself where is all your time going week after week.
How much of that time is spent ‘Net surfing or watching TV?
How much of that time is spent dawdling around at shopping centers or gossiping with neighbors?
People actually have more time today to exercise than they did a generation ago, because these days, just about everything is done with the click of a button.
People who work 40 hours a week state they don’t have time to exercise.
This includes people without young kids.
Make strength training a priority, and you’ll magically find time for it. And make it at least twice a week.
 Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified by the American Council on Exercise. At Bally Total Fitness she trained clients of all ages for fat loss, muscle building, fitness and improved health.
.
Top image: Depositphotos.com
Source: sciencedaily.com/releases/2002/05/020514072950.htm
Which Is Better for the Heart: Brisk Walking or Step Aerobics?
If all you do for cardio fitness is take an evening walk or use a treadmill, you are not getting adequate aerobic exercise. (more…)
Which Is Better for Fitness: Fast Walking or Slow Jogging ?

Let’s take a pace of 4.5 mph, and then ask yourself if jogging this will yield more fitness benefits than walking this speed (which would be a very fast walk).
For most people, walking very fast feels like more work than jogging the same speed.
This is especially true when an incline is involved (hill outside, or treadmill without holding on).
Why does fast walking seem harder than slow jogging at the same speed?
There’s a very logical explanation for this: the gastrocnemius muscle in the lower leg. This is the main calve muscle.
At around 4.5 mph, jogging makes more efficient use of the gastrocnemius, better use of it than while walking.
This was shown by Dr. Gregory Sawicki and Dr. Dominic Farris, biomedical engineers at North Carolina State University.
The researchers used ultrasound imaging, high-speed motion-capture methods and a force-measuring treadmill to investigate the “gastroc” muscle’s behavior during jogging/running and walking.
This powerful muscle makes adjustments based on whether a person walks or runs.
The gastroc “speeds up,” i.e., alters its length more and more rapidly as a person walks faster and faster.
However, this correlates to decreasing power as a person walks faster: less efficiency.
Now, when people start jogging at around 4.5 mph, the gastroc “slows down,” that is, the length changes more slowly.

This yields more power while working less: higher efficiency. This explains why it’s easier to run at 4.5 mph for 10 minutes than it is to walk at this same speed, unless a person is a trained “race walker.”
This phenomenon can be applied to slow incline walking vs. same-speed jogging.
“The muscle can’t catch up to the speed of the gait as you walk faster and faster,” says Dr. Sawicki.
“But when you shift the gait and transition from a walk to a run, that same muscle becomes almost static and doesn’t seem to change its behavior very much as you run faster and faster, although we didn’t test the muscle at sprinting rates.”
A fitness walking program should include fast walking, and a jogging program should include it as well.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.