
Save yourself endless hours of online research about sleep apnea treatment and being overwhelmed; here’s what you need to know to effectively face head-on what you know is coming.
I first began suspecting I had obstructive sleep apnea when I began corresponding with a sleep medicine doctor to help with some sleep apnea articles I was writing.
To research ideas for topics I spent countless hours lurking on two sleep apnea forums.
I also spent hours digging through Google Scholar for sleep apnea papers in medical journals.
I kept discovering new topics via the forums and also coming up with them on my own—because it looked as though this was going to be “my” medical condition, based on a few symptoms I’d been having for years (waking soon after falling asleep gasping for air, and overnight bathroom trips).
This “what you need to know” information will prevent you from being overwhelmed should you be diagnosed with obstructive sleep apnea.
Diagnosed with Obstructive Sleep Apnea
• A home sleep study can diagnose, but will not yield as much data as a sleep lab study will.
• A home sleep study is simple to set up.
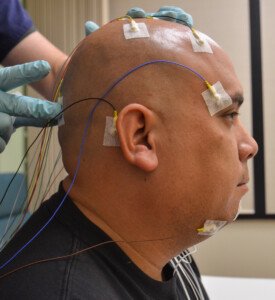
• A lab sleep study, though more comprehensive, also comes with the discomfort of sleeping out of your element and being attached to MANY wires, requiring the sleep technician to remove them every time you want to use the toilet.
• AHI refers to apnea hypopnea index (number of disordered-breathing events per hour).
• Mild OSA = AHI 5-15; moderate OSA = AHI 16-30; severe OSA = AHI over 30.
• A diagnosis of mild, moderate or severe obstructive sleep apnea is derived from the AHI, and NOT from degree of daytime symptoms.
• You will be called back for a “titration” to determine what settings and type of CPAP therapy will be most effective.
CPAP Treatment
• Considered the gold standard, CPAP is extremely effective.

Shutterstock/Oleg Golovnev
• Three mask designs: full face, nasal-only and nasal “pillows.”
• Nasal pillows slightly insert into each nostril. Some users believe this has widened their nostrils. Nasal pillows are not required for treatment; remember, you have options.
• Masks of each type come in various makes and models.
• Chin straps will help prevent mouth breathing.
• You have the right to repeatedly experiment with different makes/models and types until you find one that’s tolerable.
• CPAP machines may make annoying noise but should be on the quiet side. Work with your durable medical equipment (DME) provider on this.
• It’s common for masks to have leaks. You’ll learn the acceptable leak rate. Work with your DME on this. One of the best anti-leak masks may be the Mirage Activa.
• CPAP machines give morning feedback of overnight breathing events and other data.
• Don’t fret about machine maintenance and cleaning. You will get instructions.
• The hose should have a covering, namely to prevent moisture buildup. Online retailers sell CPAP hose covers in a variety of colors and designs.
• The mask straps that keep the device on your face come in many varieties.
• Many women report that the straps cause hair fall or breakage.
• Bella Loops are a type of strap that goes behind the ears and eliminates hair fall.
• A head cover (the type that chemotherapy patients wear) will also eliminate hair fall.
• Worried about having to repeatedly remove and put back on your mask as you make your nightly multiple trips to the toilet?
CPAP therapy should pretty much eliminate the trips because untreated sleep apnea causes the kidneys to repeatedly fill the bladder during sleep!
• Some patients report immediate, and amazing, results as far as alleviation of symptoms.
• Others report a gradual elimination.
• It may take a few months to settle into the right mask and get used to it.
• On and off CPAP use is never endorsed by doctors. Use it every night, though an occasional miss (e.g., unexpectedly stranded at someone’s house during a snowstorm) won’t harm your body.
Mandibular Advancement Device Treatment
• Can be effective for mild obstructive sleep apnea but not as efficacious as CPAP.
• Should be custom fitted by a dentist rather than purchased from a retailer.

• One study showed that it can be effective for moderate OSA in combination with a cervical collar, though not as efficacious as CPAP.
• Possible side effects include a sore jaw during the day, and altered teeth position, and saliva buildup overnight.
• Works by forcing the lower jaw forward (advancement) to keep the airway open during sleep.
• If you’ve ever struggled to tolerate, or have gagged on, a common mouth guard during contact sports, you will not tolerate the MAD.
Tongue Advancement Device Treatment
• You insert your tongue into a little containment that’s part of a bigger device that rests between your teeth overnight.
• It resembles a pacifier and cannot accidentally go into your mouth.
• Overall not as effective as MAD, but some patients with mild OSA may find success with it.
• Possible side effects include saliva buildup overnight and a sore tongue throughout the day.
Provent
• A disposable device that adheres to the nostrils via tape; a new one is used every night.
• Requires a doctor’s prescription.
• Creates back pressure when exhaling that travels to the airway to help keep it open.

• As a result, exhaling is a bit more tedious and will take time getting used to.
• Some patients report that it makes their nose feel stuffy or blocked.
MAD, TAD and Provent and are recommended only when patients have tried everything possible to tolerate CPAP and have failed.
These appliances do not provide feedback in the morning. To know how well, if at all, they are working, you need a sleep study while using them to see if they have lowered your AHI into the sub-five range. If so you’re good to go. If symptoms return you’ll need a re-evaluation.
What About Surgery?
Be extremely judicious here. The success rate of surgery isn’t exactly stellar. The more that needs to be removed, the less likely the procedure will eliminate the need for CPAP.
If it’s been determined that the only cause of your obstructive sleep apnea is enlarged tonsils, the outcome is favorable.
But if in addition to large tonsils you have a large soft palate, large uvula and other surplus pharyngeal tissue, the success rate will be much lower.
Many OSA patients who had surgery report that they eventually had to resume CPAP.
What About Weight Loss?
If you have only mild obstructive sleep apnea and are considerably overweight, losing all that weight might eliminate the OSA. Give it a try and then retake the sleep study for an updated diagnosis.

Fj.toloza992, CC BY-SA
It’s not likely that weight loss will cure moderate or severe OSA. Obesity is not an outright cause of moderate/severe obstructive sleep apnea. It’s an aggravator of a pre-existing OSA.
However, weight loss will lower the number of disordered-breathing events per hour of sleep. Always strive to lose excess body fat, even if it won’t eliminate CPAP.
What About Throat and Jaw Exercises?
These, plus blowing into musical instruments or singing, have never been proven to eliminate the need for CPAP or oral/nasal appliances.
What About Changing Sleep Position?
If you’ve been diagnosed with positional obstructive sleep apnea, it’s possible that permanently altering sleep position will eliminate the need for devices.
Positional OSA and the effectiveness of positional therapy is confirmed via a lab sleep study.
The therapeutic position is side sleeping and avoiding at all costs supine (back) sleeping. The best way to ensure you won’t roll over on your back while asleep is to sleep on a sofa.
Implements that you wear, that have “bumpers” on the back that alert you when you’re rolling onto your back, are not truly effective because they awaken you.
What About Pacemaker-Like Implants?
These innervate nerves to keep your airway dilated when a sensor detects disordered breathing.
These can be effective for some patients. Discuss this with a surgeon who has extensive experience with this type of surgery, which is a very relatively new treatment for OSA.
The list of potential permanent complications is quite unnerving. This includes impaired speech and chewing ability.
Facing a diagnosis of obstructive sleep apnea doesn’t have to be overwhelming and confusing. Knowledge is power.











