Does a Punch Biopsy for Mole Removal Hurt?

Here’s why a punch biopsy for a mole removal does NOT hurt.
You don’t need a doctor to tell you that having a mole removed via punch biopsy does not hurt. I’ve had two of these.
Actually, one of the punch biopsies was done on a harmless skin barnacle (I had requested the procedure just to play safe, because the dermatologist didn’t sound 100 percent sure that the lesion was a skin barnacle).
Anyways, the actual punch technique itself does not hurt. Prior to performing the punch biopsy, the dermatologist will anesthetize the area, which of course requires a needle to inject the anesthetic.
But in both cases, I did not perceive true pain, like the kind of pain you feel when you accidentally get pricked by a needle.
If you sew or otherwise handle needles and have accidentally gotten pricked, trust me, the anesthetizing injection feels nothing like that.
Once the area is numbed, you will not feel the “punch.” A punch biopsy is when a margin of surrounding tissue which includes below the surface of the mole is removed. As a result, stitches are necessary.
There is no pain, or at least, in my two cases there wasn’t, after the numbing drug wears off.
It doesn’t even sting or burn. In fact, the only problem I had was irritation from the adhesive of the Band-Aid.
Do not fear having a punch biopsy performed for mole removal. It does not hurt.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Top image: BruceBlaus
Breast Density Cancer Danger: Truth or Hype?

Dense breast tissue is a risk factor for breast cancer, but there’s another big problem with dense breasts: Mammograms are harder to read.
So though there may be inconsistent research findings regarding just how much of a risk factor for breast cancer that dense tissue creates, we can’t exactly sweep under the rug the fact that dense tissue in breasts can hide a malignant tumor.
“Mammographic density is referring to the ratio of breast tissue to fat on a mammogram image,” says Jennifer Hartman, a clinical nurse practitioner specializing in breast health, women’s health and cancer genetics.
“When looking at a mammogram image, fat appears dark and breast tissue is white.
“When you have dense breast tissue your mammogram image will appear with more white patchy areas than dark areas.
“Increased breast density on mammography is a problem for two reasons.
“First, breast cancer can often appear as white masses on mammograms, so if your image already has dense white patches, it makes it more difficult to find a white breast cancer nodule.
“The more dense you are, the greater the chance a small breast cancer could be missed.
“3D mammography (tomosynthesis) is definitely much better at cutting through those dense areas to find cancer than traditional 2D mammography, but it is still not perfect.
“Second, increased breast density has been associated with an increased risk of breast cancer.
“These concerns have led to 38 states currently [as of 2023] requiring that we notify patients of their breast density so they can be aware of these risks.
“Any woman with dense breast tissue should talk to their healthcare provider about their options which may include education, risk assessment and additional imaging.”
Striking Points to Consider Regarding Dense Breasts
• Body weight does not determine level of breast density or fattiness.
• Neither exercise, dietary habits, weight loss or weight gain will affect how fatty or how dense a woman’s breasts are. Breast composition is luck or un-luck of the genetic draw.
• Size, shape, feel or “perkiness” of breasts is not predictive of how fatty or dense they are.
• Only a mammogram can reveal whether breasts are mostly fatty; have scattered density; are heterogenously dense; or are extremely dense.
What should you do if you learn your breasts are dense?
It’s strongly advised to trade the 2D mammograms for the 3D (tomosynthesis).
If your health plan doesn’t provide 3D technology, then don’t let that stop you; find an independent imaging clinic and get the tomosynthesis.
Yes, you’ll pay out of pocket, but your breast health is worth every penny. So is your peace of mind.
You may also want to consider annual whole-breast screening ultrasounds.
If you must get these from an independent clinic and pay out of pocket, then DO SO.
You may need authorization from your doctor, though.
Simply inform your doctor that you have dense breasts and want to be extra vigilant.
Do not be “afraid” to request your doctor’s authorization — which should be in writing and faxed over to the clinic.
What does a “tomo” screening feel like?
I’ve had many. They feel the same as the 2D version.
Think of tomosynthesis this way: A 2D mammogram is like standing in one spot at the edge of a forest and, from that position, looking inside the woods to find a bird perched in a tree.
But tomosynthesis has you flying above the forest to look for the bird!
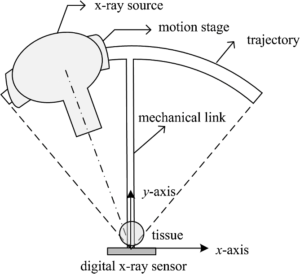
Tomosynthesis
As for the ultrasound as an additional surveillance, the whole-breast screening ultrasound is very simple from the patient’s perspective: Just lie there while the technician places the device over your breasts.
A negative 3D mammogram and breast ultrasound in the same year will be extremely reassuring!
 Jennifer Hartman, NP, specializes in surgical breast oncology and has 14+ years of nursing background involving (but not limited to) high-risk breast care, cancer genetics, breast cancer survivorship, gynecological care and homeless healthcare.
Jennifer Hartman, NP, specializes in surgical breast oncology and has 14+ years of nursing background involving (but not limited to) high-risk breast care, cancer genetics, breast cancer survivorship, gynecological care and homeless healthcare.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Freepik.com
Source: sciencedaily.com/releases/2015/12/151202084226.htm
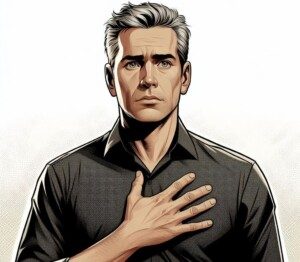
ANGINA: What It Feels Like, Duration, Triggers…

What does the chest “pain” of angina feel like and how long, or short, might be the duration?
What are possible triggers?
“Angina is a term for chest pain due to coronary heart disease,” says Waqar Khan, MD, who’s been providing state-of-the-art cardiology services to the Houston area for over 20 years, and is author of “Be Heart Smart: Understand, Treat, and Prevent Coronary Heart Disease.”
Dr. Khan explains, “It may feel different to different patients — but more commonly it feels like pressure in the chest, but it may also feel like sharp pain , dull ache, tightness or squeezing type of chest pain.”
In other words, angina can present itself in many flavors. You can’t rule out angina as the source of your chest pain just because it is any particular flavor — such as sharp, dull, squeezing, tight or heavy.
The all-encompassing descriptor for the experience would be chest discomfort.
If chest discomfort occurs when you physically exert yourself or exercise, and it subsides when you stop the activity, this is suspicious for angina — whether the discomfort is a dull ache, a pressure, a jabbing pain or a heaviness.
Keep in mind that angina can also occur while a person is at rest.
This is called unstable angina, and if you suspect this…you need to see a doctor immediately.
This is a warning that a heart attack may occur in the near future — very near, in fact.
The way unstable angina feels would be the same as how it feels when triggered by exercise or activity.
This could be sudden intense pain in the chest. Or, it could feel like that proverbial elephant sitting on the chest.
Some patients have described it as an intense squeezing or tightening — something totally unnatural.
However, angina doesn’t always feel “intense” or “severe.”
You should pay attention to exactly what you’re doing whenever the chest pain starts in to see if there’s a pattern or if changing body position relieves the chest discomfort.
Below are articles about angina. You’ll note that a few of the titles are similar; however, a different cardiologist was interviewed for those.
Physical Activity
– Can you get angina while sedentary even if exercise doesn’t trigger it?
Duration of Symptoms
– How short can an angina episode last?
Miscellaneous
– How is angina brought on by sudden strong emotions?
Digestive Connection
– Angina and vomiting: a connection?

Waqar Khan, MD, has a private practice and serves as an affiliate faculty member at Baylor College of Medicine in Houston, TX. Amazon.com/Be-Heart-Smart-Understand-Coronary/dp/1732268606
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/pikselstock
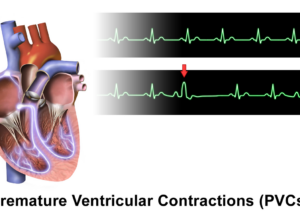
Premature Ventricular Contraction Fear: Should You Worry?
Are PVCs worth being scared out of your wits over?
Below are links to some of the premature ventricular contraction articles on this site.
All are interviews with Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
Can PVCs be life threatening if your heart is otherwise normal?
How often must PVCs occur before they begin harming the heart?
If you’re having PVCs while calm, can they still be from stress you had a while ago?
How to Calm Yourself from Anxiety that Might Be Causing Your PVCs
To calm yourself when worrying about premature ventricular contractions, start by taking slow, deep breaths to relax your body and steady your heart rate.
Practice mindfulness or meditation to shift focus away from intrusive thoughts.
Go on a kickass hike. This worked for me during a time that I was getting anxious about palpitations.
After completing the hike two hours later, I couldn’t help but think, “Gee, I must have a pretty healthy heart to have done all that with energy to spare!”
- Use physical activity as reassurance, but NOT as diagnostics.
If you’re getting a thumping or fluttering heartbeat that doesn’t seem tied to anxiety, it would be smart to get checked out by a cardiologist.
Neverthelss, you should keep exercising or start an exercise regimen: both strength training and some form of aerobics.
If you develop chest pain or nausea while exercising, then quit immediately and consult with your doctor.
How’s your sleep lately? The heart loves sound sleep. Make sure you’re doing all you can to get restorative sleep.
Caffeine and alcohol can bring on palpitations. Cut back on caffeine, and ideally, how about abstaining entirely from alcohol?
Though that may seem like a formidable task, at least make a high effort to cut back on liquor.
Don’t use alcohol as an excuse to bond socially in groups.
Another thing you can do to combat anxiety is to find a new hobby — one that relaxes you and takes your mind off your worries.
Or maybe you can revisit an old hobby that you haven’t participated in for years, such as playing a musical instrument, drawing or listening to a particular form of music.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/CHAjAMP
STEVIA Raw Chocolate Coconut Balls Simple Recipe

STEVIA Raw Chocolate Coconut Balls Simple Recipe
You will need:
– 12 level tablespoons almond meal (not “ground almonds,” but meal; this is very finely ground almonds)
– 8 level tablespoons coconut shreds
– 8 level tablespoons raw cacao powder
– 6 level tablespoons coconut oil
– 3 organic Medjool dates, pitted
– 8 packets Stevia (SweetLeaf brand; yes, it makes a difference)
– One-quarter teaspoon pure vanilla extract
One of the things that makes this recipe for Stevia raw chocolate coconut balls so unique is that it doesn’t require that many dates.
Other recipes on the ‘Net call for a lot of dates relative to other ingredients, and as a result, the balls end up tasting “datey” or even like cornflakes.
Instructions for Stevia Raw Chocolate Coconut Balls
In a big bowl, put all the dry ingredients first. A “level” tablespoon is literally level, not heaping.
To make it level, scoop up enough of the dry ingredients so that the spoon is heaping.
Then with a butter knife, skim it across the rim of the spoon (and please, use a standard measuring spoon, not a soup spoon).
The purpose of heaping the spoon is to make sure no air pockets are formed when you skim. In fact, skim by “bouncing” the knife as you go.
After the dry ingredients, put in the coconut oil (never refrigerate; not necessary; it has an extremely long, if not indefinite, shelf life as long as it’s securely sealed).
If you put the coconut oil in before the dry ingredients, the dry ingredients will stick to the spoon—unless you don’t mind cleaning up the spoon first.
With a butter knife, scoop out the oil (assuming it’s solid; it liquefies if room temperature is 76 degrees) and stuff into the tablespoon, then skim the surface.
Make sure there are no air pockets. Skim really good so that the surface of the oil is flush or even with the rim of the spoon. With butter knife, then dig it out thoroughly and put in the bowl.
Add the Stevia. I’ve tried other brands of Stevia, and trust me, SweetLeaf is the best. The other brands are bland and don’t do much for sweetening.
Add the vanilla extract.
With a food processor, grind up the dates. IMPORTANT: Grind up so that the end product has almost the consistency of peanut butter, in that it’s spreadable.
It doesn’t have to be creamy smooth, but almost so. If there’s a chunky-particle appearance to it, it needs more processing.
Add this spreadable date goop to the bowl.
With a sturdy steel or wooden mixing spoon, mix everything by aggressively pressing the bottom of the spoon, from the edge of the bowl towards the center, rotating the bowl with the other hand.
If your food processor can handle mixing all the ingredients, then process the dates first (so that you can visually confirm spreadability), then add the remaining ingredients. My food processor can’t handle powder; it jams the blades.
But if you’re mixing in a bowl by hand (electric mixers won’t work), you must be patient and aggressive; it takes some elbow grease.
Just keep furiously mixing, and you’ll note that the clumps of coconut oil and dates will NOT be evenly distributed.
Press on these with the spoon to further break them down and distribute them throughout the dry mix. You don’t want any one ball to have a large clump of just date or coconut oil in it.
Keep mixing till it looks like everything is evenly distributed, no isolated clumps of date goop or coconut oil.
IMPORTANT: The final mixture will appear too dry to form into balls. Do NOT add anything. If you add even another one-quarter tsp of vanilla, the balls may be too sticky.
Grab enough of the mix to make a ball, and squeeze in your palm to compact it first, then mold into a sphere between two rotating palms, a ball.
With fingers, first compact the mix a little, then begin rolling—and use enough mix to make balls almost the size of a ping pong ball.
This recipe makes 12 balls, depending on the size you roll them.
Again, the mix will appear too dry to mold into balls, but it will mold very nicely and they will hold in place.
If you want the balls to be sticky enough to roll in coconut shreds, almond meal or chia seeds, add another quarter teaspoon of vanilla. If this doesn’t quite do it, add another quarter teaspoon.]
Once nicely molded, place on a plate and refrigerate for later on if you prefer them cold, but they taste just divine at room temperature.
In fact, when refrigerated, these Stevia raw chocolate coconut balls take on a denser quality, but at room temperature, have a consistency resembling non-refrigerated squares of fudge.
These Stevia raw chocolate coconut balls are SUPER good for your body! And doggone it, you won’t believe how great they taste!
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Causes of Waking with Racing Heart After Falling Asleep

Waking in the middle of the night with a racing heart can have minor to serious causes.
Have you been awakening in the middle of the night to find that your heart is racing? Below is information for both men and women.
“One of the common causes is simply sinus tachycardia or a fast, normal rhythm,” says cardiologist Dr. Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
“This condition does not need to be treated and does not regularly reoccur.”
In other words, it’s just something that occurred while you happened to be asleep, and the change in pulse was enough to awaken you.
This same situation can happen during the day but go unnoticed if you’re up and about.
If you’re noticing these incidents, document when they occur and record your pulse, to see if over time, there’s a pattern or if these incidents of a “racing” heart are happening less frequently — or more frequently—than it seems.
Another possible cause of awakening with a racing heart in the middle of the night is atrial fibrillation, says Dr. Marcovitz.
A-fib is a potentially serious disorder, as it can increase the risk of blood clots and cause symptoms including faintness.
During an A-fib episode, the heart rate bounces all over the place; it’s not steady.
In sinus tachy, the sped-up rate is steady, as in, for instance, a steady rate of 110 beats per minute (which may fluctuate a few beats up or down every minute).
In A-fib, the pulse is not steady, and a heart rate monitor would show the numbers quickly jumping from (for instance) 110 to 174 to 142 to 170 to 94 to 152. Do not try to diagnose yourself with A-fib.
“Feeling frightened and/or having a dream or nightmare, especially if the dream involved running or physical activity, whether you remember it or not, is another possible cause” of being awakened in the middle of the night with a racing heart, says Dr. Marcovitz.
“This late night response, however, should only occur very occasionally.
If it occurs more frequently, including throughout the day, see your doctor for possible connection to a heart monitor, which will evaluate for treatable causes,” including A-fib.
Another possible cause is a panic attack while you’re asleep. Yes, this can happen.
Years ago I was dreaming I was with my brother; nothing too eventful was playing out.
But in the dream I became aware that my heart was pounding—and fast. This then awakened me — and my heart was racing and pounding.
What I believe happened was during the REM stage of sleep (rapid eye movement; dreaming), my body physically had a spontaneous panic attack.
And it worked its way into the dream I just happened to be having, kind of like how the need to urinate can work its way into a dream (e.g., you’re searching for a restroom but can’t find one).
So, I literally awakened with a racing heart. I was so afraid for my heart — even though I did a lot of exercise — that I called 9-1-1 and an ambulance took me to the hospital.
In the ambulance my heart rate was in the 130s. At the ER it turned out that my heart was just fine (according to an EKG, stethoscope exam and troponin test).
Other Causes of Awakening in the Middle of Night with a Racing Heart
“Sleep apnea, anxiety and high blood pressure may also cause a person to awaken with a fast or racing heart rate,” says Dr. Marcovitz.
“These are potential causes for which a person should be evaluated.”

Dr. Marcovitz has 40+ years of experience in helping people improve their heart health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Photographee.eu
PVCs after Eating Not Caused by Food

A cardiologist says that PVCs or heart palpitations after eating are not caused by the food or the physical act of eating.
“Blood flow is shunted to the intestine after eating, so we can digest our food,” says cardiologist Dr. Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
“More blood also flows to the digestive organs. This is usually not a cause of palpitations or PVCs after eating.”
So why do some people experience PVCs after eating?
They should make a documentation of this when it occurs: time of day, who was present with them during the meal, the planned activity after the meal, and any other stressors that were present while eating or shortly after.
PVCs can be brought on by anxiety and stress.
When you’re anxious or stressed, your body’s fight-or-flight response can trigger these irregular heartbeats.
This is because stress and anxiety increase adrenaline levels, which can affect heart rhythm.
So think about this: Do your PVCs usually occur after a meal with people you were arguing with?
Do they usually occur after the last bite, and within how many minutes?
Do they usually occur when the after-meal planned activity is something stressful, like going over your bills?
Eating, in and of itself, and food, do not cause premature ventricular contractions, says Dr. Marcovitz.
The rhythm control center of the heart, known as the sinus node, is not directly linked to the digestive system.
Instead, it is located in the right atrium of the heart and is responsible for initiating and regulating the heart’s electrical impulses, which control the heartbeat.
However, the body’s autonomic nervous system, which affects both heart rate and digestion, can influence how they interact.
For example, stress or a heavy meal can affect heart rate (steady beats per minute, not PVCs) due to changes in autonomic nervous system activity, but the sinus node itself does not directly connect to the digestive system.
What Another Cardiologist Says About PVCs and Eating
Chester M. Hedgepeth, III, MD, PhD, Executive Chief of Cardiology at Care New England, says that certain foods can cause palpitations, and that there are six causes for why you may feel what seems like PVCs during and soon after eating.

Dr. Marcovitz has 40+ years of experience in helping people improve their heart health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/Monster e
Are PVCs Connected to GERD in any Way?

There is probably a link between PVCs and GERD.
PVC stands for premature ventricular contraction, and GERD refers to gastroesophageal reflux disease.
Are PVCs associated with GERD?
“I think they are,” says cardiologist Dr. Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
She continues, “I find a lot of people who have GERD tell me they have PVCs. When you lay down at night, if you have GERD, small microscopic droplets of food may travel up the esophagus into airways, thus causing PVCs.”
The link between heart “palpitations” and acid reflux may also occur via other pathways.
For instance, both the “skipped heartbeat” sensation and acid reflux can be caused by anxiety.
So the symptoms, then, have a common cause in this case, but the symptoms do not act upon each other.
Do your PVCs calm down when you take a medication for heartburn?
Which usually comes first, a bout of GERD or a string of PVCs?
Take a note of timelines, concurrent stressors and your activities at the time the symptoms act up.
Over time you may discover a common denominator that can help you relieve yourself of these issues.

Dr. Marcovitz has 40+ years of experience in helping people improve their heart health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: Shutterstock/SZ Photos
Strong Heartbeat Awareness: Causes & Solutions
Dang, there goes that “cardiac awareness” again:
You REALLY feel your heart beating, or maybe this goes on for long stretches of time—even though you’re not physically exerting yourself.
“Some people are just more aware of their heartbeat than others,” says cardiologist Dr. Pam Marcovitz, MD, an internal medicine cardiologist with Frankel Cardiovascular Center in MI.
This awareness of the heart’s pumping action applies equally to men and women.
“People also seem to notice their heartbeat when they lie down to go to sleep at night, because they are quiet,” continues Dr. Marcovitz.
“If you’re heart rate is normal, it might simply be a heightened awareness, rather than a stronger than average heartbeat.”
Something inside of you is continuously pumping. Of course you will feel this at rest from time to time.
It may be more prevalent if your chest is snuggly against an arm while you’re in bed.
See what happens when you relax the snug. Experiment with different positions to see if any particular position heightens the cardiac “awareness” or diminishes it.
Ask Yourself this Question
Has your heartbeat always been strong or noticeable, but only recently you’ve been growing concerned about it?
“Becoming vigilant about noticing your heart rate may cause anxiety in and of itself, which in turn can increase heartbeat,” says Dr. Marcovitz.
“Some people are prone to panic attacks and hyperventilation, which can cause a stronger heartbeat.
“To address these challenges, take some deep breaths. If you’re hyperventilating, breathe into a paper bag. Simply try to relax.”
Another tactic is to remind yourself that it’s better to hear a beating heart than to hear what a non-beating heart would sound like!
Of course, if your heart were not beating — you would not be conscious to be aware of this since the brain needs a continuous supply of blood to function.

Dr. Marcovitz has 40+ years of experience in helping people improve their heart health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.
Top image: ©Lorra Garrick
Should You Do Deadlifts on Back or Leg Day or BOTH ?

A big question in the muscle building world is whether deadlifts should be done on leg day or back day, but … why choose?
If you’ve been deadlifting only once a week and have not been making much progress, you may want to consider doing this exercise twice a week.
As for deadlifting only once a week, there are people who get great results when they are done only on leg day, and others when it’s done only on back day.
And many athletes swear that deadlifts, due to the bigness of this movement, should be done twice a week: back AND leg day.
You’re going to have to experiment. The correct answer to the question is not drilled into steel.
But one thing is for sure, whether you perform deadlifts on only leg day, only back day — or BOTH days:
It should be either your first exercise or second if your first is the back squat.
The Deadlift Is a Giant
This compound giant really take it out of you, and you want to be as fresh and as charged up as possible before starting your deadlift routine.

Freepik.com
Some people also find that doing some pull-ups or chin-ups before the deads can help, but that’s up to you.
As long as you don’t deadlift AFTER you’ve pre-fatigued your back and arms with working sets of rows and pull-downs.
And on leg day, you don’t want to hammer your body with multiple leg routines prior to doing deadlifts.
As mentioned, on leg day it’s fine if your first exercise is the barbell squat–moving right into the deadlift as the second exercise.

Freepik.com
Waiting towards the middle of your session to deadlift will also be psychologically dismantling.
Just get them out of the way very early on in the workout whether it’s a leg day or a back day.
I recommend twice a week for the deadlifts, even though again, find out what works best for you.
But the thing is, if you perform deadlifts twice a week, and at some point you must miss one of these workouts, at least you will have the other one for that same week going for you.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.