For more than three decades, National Breast Cancer Awareness Month (BCAM) has propelled public education on the causes and risks of breast cancer, the importance of early screening and diagnosis, and the growing number of treatment options available today.
An important part of BCAM is National Mammography Day, which today marks its 25th anniversary of serving as a reminder that the best defense against breast cancer is early detection.
While this awareness month empowers many women, some still find themselves hesitant to discuss their breast health with physicians or family members.
Maybe they feel the topic is irrelevant due to their age, or perhaps fear the unknown or have a desire to avoid medical tests that could bring unexpected news.
However, this longstanding campaign has worked to eradicate the taboo nature of cancer discussions and open the door for all women to have candid conversations about their breast health.
In addition, it sets the stage and inspires thousands to receive regular exams and tests that can lead to earlier diagnosis and better health outcomes.
The Starting Point to Better Breast Health
Each new year, many people set goals and resolutions related to improving their health. But do these include breast health?
About one in eight women will develop breast cancer over the course of her lifetime.

Freepik.com
It’s expected that during this year alone, more than 330,000 new cases of both invasive and non-invasive breast cancer will be diagnosed in women across the country.
More importantly, perhaps, is that two-thirds of women with breast cancer have the potential to be saved through early detection and progressive treatments, according to Breastcancer.org and Bremfoundation.org.
Given these statistics, it’s important to take steps every day that can have a major impact on your long-term breast health:
- Take care of yourself – Studies show that lack of sleep, high-fat diets and lack of exercise can increase your risk of developing breast cancer or experiencing a recurrence.
- It’s essential to get the recommended eight hours of sleep, eat a healthy diet and exercise regularly. If you do happen to notice any abnormalities, contact your doctor immediately.
- Perform self-exams – The first step in early detection is paying attention to your own body.
- You should regularly check your breasts (at least monthly) for any abnormalities. These self-exams can be done in the shower, in front of a mirror or lying down.
- Get an annual screening – Regular mammograms, which are simply an X-ray of the breast, are the next line of defense in early detection, as they can help identify breast cancer in women who may not even be showing any signs or symptoms.
- Unfortunately, many women skip their annual screening. It’s crucial to never miss a mammogram, as they can detect early stages of breast cancer long before you have any signs or symptoms.
- Research your family background – Breast cancer can be hereditary, as gene defects (called mutations) can be passed on from a parent.
- As such, it’s important to speak with family members about their health history to determine if breast cancer runs in the family.
- If so, you may want to consider genetic testing to learn more about your risk.
The 411 on Mammograms
While we’ve discussed that getting your annual screening is the best proactive step for monitoring your breast health, it’s important to know that not all mammograms are created equal.
For years, physicians have relied on 2D mammograms (once considered the gold standard for detection of breast cancer), which only produce four images of the breast: two from top to bottom and two from side to side.
This type of screening has numerous shortcomings, including showing overlapping normal breast tissue as potential areas of concern.
Tomosynthesis for Early Detection of Breast Cancer
If you’ve had a 2D mammogram before, it’s likely you’ve experienced fear and anxiety from false positives, and may have even required unnecessary follow-up procedures, including additional mammograms, ultrasound or even invasive, painful biopsies.
Today, however, 3D mammograms, also referred to as digital breast tomosynthesis (DBT), are used more frequently for testing.
The 3D mammogram uses the same X-ray technology as 2D mammograms, but allow radiologists to view hundreds of images of the breast in “slices” from many different angles.
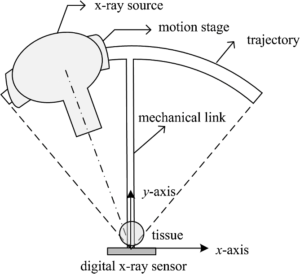
Tomosynthesis
This approach provides more detail about the breast tissue and offers greater clarity in detecting true abnormalities.
Since 3D mammograms produce so many images, however, radiologists must spend significantly more time reviewing and interpreting each exam.
The upside? With innovative technologies available today, radiologists can use solutions that leverage artificial intelligence to help them reduce the amount of time spent reading a patient’s breast images, as these technologies automatically detect and pinpoint areas that might be concerning.
These capabilities are crucial today and offer radiologists the extra layer of security and confidence they need to ensure no significant findings have been missed when reading mammograms.
In addition, various studies have shown that 3D mammography not only offers higher cancer detection rates, but also results in fewer re-calls for patients.
This simply means they do not have to come back to their doctor for additional imaging or other tests as often.
The Correlation Between Breast Density and Breast Cancer
Even though much of the early diagnosis and prevention focus is on regular self-exams and mammograms, some other important aspects of breast health are also not as widely discussed.
One of those is breast density, a comparison of the amount of fat to the amount of tissue on a mammogram.
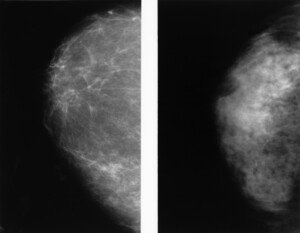
Fatty breast on left; dense on right. Cancer.gov
Breasts that contain more glandular and fibrous tissue than fatty tissue are considered “dense” and often make it more difficult for a radiologist to examine.
- High breast density is more common than you may imagine.
- Up to 50 percent of women ages 40-74 have dense breasts, with younger and thinner women being more susceptible.
In fact, research has shown women with dense breasts can be six times more likely to develop breast cancer.
Compounding these odds is the fact that it is harder for mammograms to detect breast cancer in dense breast tissue.
Both breast cancer and breast gland tissue appear white in mammograms, making it more of a challenge to discern whether a woman may have cancer.
However, new technologies today can actually help radiologists better evaluate and score breast density to identify patients who may be at a higher risk of developing breast cancer.
How do you know if you have dense breasts?
Ask your doctor or the clinician doing your mammogram to tell you (another reason why getting your annual exams are very important!).
Currently there are 35 states that require varying levels of notification following a mammogram to notify you about breast density following a mammogram.
If you do have dense breasts, annual 3D mammograms are a must.
You may also need more sophisticated screening, such as an MRI and molecular breast imaging (MBI).
Additionally, breast ultrasounds can help find some breast cancers in dense breasts that cannot be seen on mammograms. More information about risk-based screening can be found at Bremfoundation.org.
Be Your Own {Breast} Health Advocate
All in all, it’s important to serve as your own personal breast health advocate and ask your doctor any questions related to breast care, cancer or density.
If you are concerned that you may have breast cancer – based on family history or abnormalities, you discover during self-exams – do not wait for answers or help.
It’s critical to not only educate yourself, but also to take the steps necessary to ensure you are receiving the best possible care.
This National Mammography Day, we hope you feel empowered to ask the difficult questions and inspired to schedule your annual mammogram.
In addition, we suggest you start a dialogue with other friends and family members about breast health and density, motivating others to perform self-exams and get their yearly screenings as well.
These baseline tests are vital to early detection and are your best defense against breast cancer.

Rachel F. Brem, MD, is Director of Breast Imaging and Intervention, Professor & Vice Chair, Department of Radiology, The George Washington University Medical Center.
.










































